Patellar Fractures
***Editing in process***
Definition/Description[edit | edit source]
Patella fractures are caused by directly by trauma or a compressive force, or indirectly as the result of quadriceps contractions or excessive stress to the extensor mechanism.[1][2][3] Indirect injuries are commonly associated with tears of the retinaculum and vastus muscles.[1] Patella fractures make up about 1% of all skeletal injuries.[4][5]
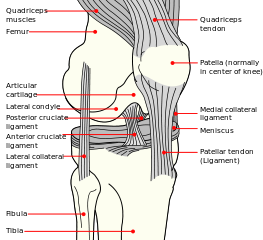
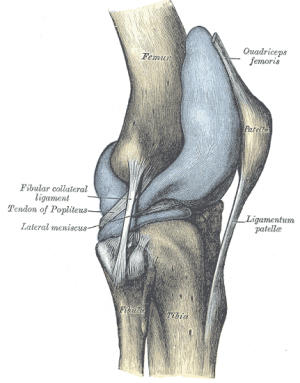
Clinically relevant anatomy[edit | edit source]
The patella is a triangular bone situated on the anterior surface of the knee at the distal end of the femur. It is the largest sesamoïd bone in the body and makes part of the knee joint.[6][7][8] Vastus medialis and lateralis, as part of the quadriceps group, control movement at the patella.[9] The extensor mechanism as a whole plays a major role in patella fractures. This consists of the quadriceps, quadriceps tendon, retinaculum, patella tendon, tibial tubercle and patellofemoral and patellotibial ligaments,[10] See the page on the patella for more details.
Epidemiology/Etiology[edit | edit source]
In a recent study, the average mortality rate at one year after patella fractures was 2.8%, increasing to 6.2% in the geriatric population. Patella fractures are not associated with an increased mortality rate, as the relative risk of death was 0.9.[11]
Complications[edit | edit source]
- Injuries (sprain/rupture) to ligaments and tendons attached to the patella:
- Long term complications include stiffness, extension weakness, and patellofemoral arthritis.[12]
- Avascular necrosis[13]
- posttraumatic arthritis.
- Osteochondral damage to patella-femoral joint
- Stiffness
- Non-union
- Malunion
- [1]
Characteristics/Clinical Presentation[edit | edit source]
Types of fractures[edit | edit source]
Patella fractures are classified as either displaced or non-displaced. Displaced fractures are unstable and can be further classified as:[14]
- Comminuted: As a result of direct trauma (mostly due to blows or falls on flexed knee)
- Can cause damage to the articular cartilage of patella and femoral condyles.
- Tansverse/stellate: As a result of muscle contraction/extensive stress on the extensor mechanism, e.g. explosive quadriceps contraction after jumping from height.
- Most common type
- Proximal blood supply may be compromised
- Usually as a result of hyper flexion of the knee
- Marginal: As a result of a fall on the knee
- Vertical
- Lower/upper pole
- Osteochondral
- Sleeve (only in paediatric patients)
The prognosis of the injury depends on the amount of chondral damage at the time of injury. Functional outcome depends on the ability to achieve pain-free and stabile range of motion in an early stage. [17]
Differential diagnosis[edit | edit source]
- Bipartite patella[1]
Diagnosis[edit | edit source]
Interview[edit | edit source]
- Details regarding accident
- Mechanism of injury
- Pain at knee
- Complaints of difficulty standing or snapping sensation at knee
Physical examination[edit | edit source]
- Observation:
- Whole extremity
- Swollen, bruised knee
- Deformity around knee
- Possible wounds (open fracture)
- Palpation (often done after local anesthetics to eliminate pain):
- Tenderness around patella
- Palpable gap (for displaced fractures)
- Rule out concomitant injuries:
- e.g. fractures of the acetabulum, femur and tibia
- Haemarthrosis
- Range of motion:
- Acute:
- Limited knee and painful knee flexion and extension
- Often unable to do straight leg raise
- Chronic:
- Full knee flexion with extension lag
- Acute:
- Distal pulses
- Assess compartment of the leg
- Neurological assessment
Special investigations[edit | edit source]
- X-rays:
- AP view:
- May be difficult to see patella
- Lateral view:
- Undisplaced - < 2mm separation
- Displaced - > 2mm separation
- Sky view
- Regular monitoring of healing process and any possible complications
- AP view:
- CT scan: Usually not needed
- MRI: Diagnosis of associated injuries to nearby tendons and ligaments
- Bone scans: To identify stress fractures
Outcome measures[edit | edit source]
- Knee injury and osteoarthritis outcome score
- Knee outcome survey
- Lower extrimity function scale
- McGill pain questionnaire
Medical management[edit | edit source]
In acute cases, local anesthetics can be given to eliminate pain.[18] This helps to aid in the assessment and diagnosis of the patella fracture.
Conservative management[edit | edit source]
Indication: Undisplaced fracture (mostly vertical and horizontal fractures) with extensor mechanism in place [1][17]
- Fracture immobilized with cast or splint (start off in full extension):
- As healing takes place, knee flexion can gradually be increased
- Must be worn until union (on X-rays) and clinical signs of healing (not tender on palpation) are present
- Crutch walking 6-8 weeks
- Rehabilitation
Surgical intervention[edit | edit source]
Indication: Significant displacement with extensor mechanism not intact.[1]
Aim: Restore extensor function, align articular incongruities, and allow early motion[17][20][23][24]
Management:[1]
- Open reduction and internal fixation using tension band wire technique
- Transverse fracture: Open reduction and internal fixation using tension band wire technique using pins and wires and 'a figure of eight' to press the pieces together
- Comminuted fracture: Partial vs complete patellectomy:[18]
- Quadriceps muscles is is attached to the patellar ligament to ensure function of the extensor apparatus during a complete patellectomy[18]
- Patellectomy: Relatively old procedure, last treatment of choice
- Repair of bilateral vastus muscles
- Rehabilitation same as with conservative management
Later stages:
Manipulation under anesthesia or the arthroscopic releasing of adhesions is required when athrofibrosis occurs.[17]
Physiotherapy management[edit | edit source]
Extensor mechanism in place
Extension splint. as fracture heals, gradulally increase knee flexion. quads strengthening in inner ranges. -SPORT
cons mx Crutches will be used during the 6 to 8 week healing process.[22][10]
Treatment with cold can be used to control pain and oedema. During the immobilization of the knee the patient is encouraged to train other leg muscles. After removing the cast or splint, and the fracture is considered healed, the therapy to regain range of motion starts.
There are instructions to prevent loss of motion and strength in adjacent joints. Ankle exer-cises are taught to promote circulation.
The range of motion, strengthening, and proprioceptive exercises of the involved joint should be initiated and progressed as indicated and tolerated by the individual. [25]
ignificant displacement, extensor mechanism not intact. ORIF tension band wire technique. Repari or bilater. vastus. same rehab as with no-operative-SPORT
Treatment procedure Post-Operative :
Phase
I:
0-2
Weeks
Knee
Immobilizer:
Worn
at
all
times
(taken
off
only
for
physical
therapy
sessions
converted
to
hinged
knee)
brace is worn
at
first
post‐op
visit
- Weight bearing: with the knee locked in extension
- Range of Motion: 0‐30 degrees
- Therapeutic Exercises:
•
Isometric
quadriceps/hamstring/adductor/abductor
strengthening,
• Ankle
theraband exercises
Phase
II:
2-6
Weeks
Knee
Brace:
Worn
with
weight bearing
activities
still
locked
in
full
extension,
may
be
removed
at
night
- Weightbearing:
- Range of Motion: add 15 degrees of flexion each week –
- Goal is 90 degrees by post‐op week 6
- Therapeutic Exercises:
• Isometric
quadriceps/hamstring/adductor/abductor
strengthening,
• Ankle
theraband
exercises,
• Initiate
straight
leg
raises
Phase
III:
6-10
Weeks
Knee
Brace:
Unlocked,
worn
with
weight bearing
activities
- Weightbearing: Full
- Range of Motion: progress to full ROM by post‐operative week 10
- Therapeutic Exercises: Isometric quadriceps/hamstring/adductor/abductor strengthening, Ankle theraband exercises, Initiate straight leg raises
Phase
IV:
10-12
Weeks
Knee
Brace:
Discontinue
- Weightbearing: Full
- Range of Motion: Full
- Therapeutic Exercises: Isometric quadriceps/hamstring/adductor/abductor strengthening, Ankle theraband exercises, Initiate straight leg raises, Start stationary bicycle
Phase
V:
36
Months: return
to
full
activities
as
tolerated
(Strauss J. (MD)(level of evidence : 5), Elizabeth Arendt(MD) ( level of evidence: 5) )
Treatment procedure Non-Operative :
Phase
I:
0-6
Weeks
• Knee
Brace:
Brace locked in extension 2-3 weeks, controlled motion brace at 2-3 weeks
o Weightbearing:
• PWB in brace and on crutches.
• May stand tandem.
• Duration of crutches as per surgeon
o Range
of
Motion:
ROM as per surgeon
o Therapeutic
Exercises:
• Start open kinetic chain strengthening and ROM of knee at 3-4 weeks or per surgeon order.
• Quadriceps
• Hamstring
• Glutei sets
• SLR
Open and close kinetic chains hip strengthening exercises.
• Patellar mobilization
Examples of a knee braces after a patellar fracture:
Open kinetic chain strengthening and ROM of knee:
Phase II: 6-12 Weeks
• Knee Brace: Discharge per surgeon order
o Range of Motion: Progress toward full knee flexion, extension
o Therapeutic Exercises:
▪ Stationary biking with seat elevated and no resistance for ROM
▪ Progress close kinetic chain exercise: mini squats, step up, retro step, etc
▪ Progress resistance on hip exercise.
▪ Advance proprioceptive exercise
▪ Begin lunges 8-10 weeks
(Strauss J. (MD)(level of evidence : 5), Elizabeth Arendt(MD) ( level of evidence: 5), Kathryn E. Cramer, MD et al (level of evidence 5 )
Examples of exercices:
Quadriceps: The patient sits on the floor with his injured leg straight and his other leg bent. He presses the back of the knee of his injured leg against the floor by tightening the muscles on the top of his thigh. He has to hold this position 10 seconds and then re-lax, the patient does 2 sets of 15seconds. (Bhave A et al. (Level of evidence :5), Creighton AR et al. (level of evidence : 5))
SLR : The patient has to lie on his back with his legs straight. Then he has to bend the knee on his uninjured side and place his foot flat on the floor. Once this is done, he has to tighten the thigh muscle on his injured side and lift his leg about 8 inches off the floor. The patient keeps his leg straight and his thigh muscle tight and then he brings his leg slowly back down to the floor. This exercise is also done in 2 sets of 15 seconds. Bhave A et al. (Level of evidence :5), Creighton AR et al. (level of evidence : 5)
Patellar mobilisation :
o Patient sits with his injured leg in front of him. His leg should be completely straight and relaxed. Patient has to use his hands to move the patella sideways toward the inside of his leg. Then he has to move it sideways toward the inside of his leg. Each position has to be hold for 15 to 30 seconds.
Fourati M.K. (level of evidence:2b), Elizabeth Arendt(MD) (level of evidence: 5),Bhave A et al. (Level of evidence :5), Creighton AR et al. (level of evidence : 5)
o Patient has to use his hands to move his patella toward him and then away from him for 15 to 30 seconds in each direction. Then he has to compare the movement of the injur
ed patellla with the movement of the uninjured patella. The main goal is to have the same amount of movement for bouth kneekaps.
Resources
[edit | edit source]
http://www.physioroom.com/injuries/knee/patella_fracture_full.php
http://www.summitmedicalgroup.com/library/adult_health/smapatellarfractureexecises_references/
http://www.mdguidelines.com/fracture-patella
http://www.ncbi.nlm.nih.gov/pubmed/?term=patellar%20fracture
http://www.healthline.com/human-body-maps/knee
References
[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Frobell R, Cooper R, Morris H, Arendt, H. Acute knee injuries. In: Brukner P, Bahr R, Blair S, Cook J, Crossley K, McConnell J, McCrory P, Noakes T, Khan K. Clinical Sports Medicine: 4th edition. Sydney: McGraw-Hill. p.626-683
- ↑ 2.0 2.1 Schuett DJ, Hake ME, Mauffrey C, Hammerberg EM, Stahel PF, Hak DJ. Current treatment strategies for patella fractures. Orthopedics. 2015;38(6):377-84.
- ↑ 3.0 3.1 Archdeacon, Michael T., and Roy W. Sanders. Chapter 54 - Patella Fractures and Extensor Mechanism Injuries. In: Browner BD, Jupiter JB, Krettek C, Anderson PA, editors. Skeletal Trauma, 4th edition. Elsevier Health Sciences, 2008.
- ↑ Crowther MA, Mandal A, Sarangi PP. Propagation of stress fracture of the patella. British journal of sports medicine 2005;39(2):e6.
- ↑ Sweetnam R. Patellectomy. Postgraduate medical journal 1964 Sep;40(467):531.
- ↑ Cedars-Sinai. Fractured Kneecap. Cedars Sinai organisation. https://www.cedars-sinai.org/health-library/diseases-and-conditions/f/fractured-kneecap.html (accessed 25/07/2018).
- ↑ Schunke M. Anatomische atlas Prometheus, algemene anatomie en bewegingsapparaat. Bohn Stafieu van Loghum: 2e druk. 2010.
- ↑ Everett L. Knee and Lower Leg. In: Marx J, Walls R, Hockberger R, editors. Rosen's Emergency Medicine: Concepts and Clinical Practice. 6th ed. Philadelphia: Mosby Elsevier, 2006.
- ↑ Orthopaedia. Collaborative Orthopaedic Knowledgebase, http://www.orthopaedia.com/display/Main/Patella+fractures (accessed November 10, 2010).
- ↑ 10.0 10.1 10.2 10.3 Duke Orthopaedics. Wheeless’ textbook of Orthopaedics. Fractures of the patella.http://www.wheelessonline.com/ortho/fractures_of_the_patella (accessed November 10 2010).
- ↑ Larsen P, Elsoe R. Patella fractures are not associated with an increased risk of mortality in elderly patients. Injury 2018.
- ↑ Insall JN. Fractured kneecap: treatments. Institute for Orthopaedics and sports medicine 2007.
- ↑ 13.0 13.1 Medscape. Patella Fracture Imaging. http://emedicine.medscape.com/article/394270-overview> (accessed 25/07/2018).
- ↑ 14.0 14.1 Whittle PA. Fractures of the Lower Extremity. In: Canale ST, Beaty JH, editors. Campbell's Operative Orthopaedics. 11th ed. Philadelphia: Mosby Elsevier, 2008.
- ↑ Melvin SJ, Mehta S. Patellar fractures in adults. Journal of the American Academy of Orthopaedic Surgeons 2011;19(4):198-207.
- ↑ 16.0 16.1 16.2 Walters J, editor. Orthopaedics - A guide for practitioners. 4th Edition. Cape Town: University of Cape Town, 2010.
- ↑ 17.0 17.1 17.2 17.3 17.4 Mehling I, Mehling A, Rommens PM. Comminuted patellar fractures. Current Orthopaedics 2006;20(6):397-404.
- ↑ 18.0 18.1 18.2 18.3 18.4 Günal I, Karatosun V. Patellectomy: an overview with reconstructive procedures. Clinical Orthopaedics and Related Research 2001;389:74-8.
- ↑ 19.0 19.1 McRae R, Esser M. Practical fracture treatment E-book. Churchill Livingstone/ Elsevier; 2002.
- ↑ 20.0 20.1 20.2 Fourati MK. Reeducation du genou après fracture de la rotule. Ann. Kinésitherapie 1986.
- ↑ Scolaro J, Bernstein J, Ahn J. In brief: patellar fractures. 2011;1213-1215.
- ↑ 22.0 22.1 American Academy Of Orthopaedic Surgeons. Diseases and conditions - Patellar (Kneecap) Fractures. http://orthoinfo.aaos.org/topic.cfm?topic=A00523 (accessed November 10, 2010).
- ↑ Shang ZG. Patellar fractures treatment and management. Unbound medline 2013;26(6):445-8.
- ↑ Strauss J. ORIF Patella Fracture Post-Operative Rehabilitation Protocol, Hospital for Joint Diseases, 2008.
- ↑ Medical Disability Guidelines , http://www.mdguidelines.com/fracture-patella (ac-cessed December 26, 2010)