Parkinson's - Physiotherapy Management and Interventions: Difference between revisions
(added updated references, edited for UK spelling and grammar) |
Oyemi Sillo (talk | contribs) No edit summary |
||
| Line 6: | Line 6: | ||
== Introduction == | == Introduction == | ||
A person with [[Parkinson's_Disease|Parkinson’s]] may be experiencing several symptoms at the same time; your history taking and physical assessment '''should elicit the main issue (s) to prioritise as part of the management strategy'''. While physiotherapy concentrates on the physical manifestations of a disorder, '''it is also important to pay attention to how other symptoms impact upon the person’s lifestyle'''. | A person with [[Parkinson's_Disease|Parkinson’s]] may be experiencing several symptoms at the same time; your history taking and physical assessment '''should elicit the main issue(s) to prioritise as part of the management strategy'''. While physiotherapy concentrates on the physical manifestations of a disorder, '''it is also important to pay attention to how other symptoms impact upon the person’s lifestyle'''. | ||
Remember also that optimal outcome is achieved through the collaboration with others from a team of health and social care professionals with expertise in other domains of Parkinson’s, from volunteers to family and friends. | |||
== Aims of Physiotherapy == | == Aims of Physiotherapy == | ||
| Line 26: | Line 26: | ||
=== Exercise === | === Exercise === | ||
Exercise has been proven to maintain health and well-being in Parkinson’s and now importantly it is shown to play a big role in addressing secondary prevention (focusing on strength, endurance, flexibility, functional practice and balance). Exercise for neuroprotection focuses on endurance and uses motor learning principles approaches, such as mental imagery and dual task training. Neuroprotection training, to be effective, should be introduced in the early stages | Exercise has been proven to maintain health and well-being in Parkinson’s, and now importantly it is shown to play a big role in addressing secondary prevention (focusing on strength, endurance, flexibility, functional practice and balance). Exercise for neuroprotection focuses on endurance and uses motor learning principles approaches, such as mental imagery and dual task training. Neuroprotection training, to be effective, should be introduced in the early stages but helps at all stages. It involves complex, powerful and intensive exercises. | ||
Exercise undertaken in a group setting has the added value of providing a social connection to those becoming increasingly isolated as the condition progresses, | Exercise undertaken in a group setting has the added value of providing a social connection to those becoming increasingly isolated as the condition progresses, and those who are newly diagnosed are able to observe the benefits of maintaining exercise and activity. A group environment also permits time for people to ask questions and discuss their symptoms and own management strategies with one another. | ||
Transition Care setting<ref>Transition Care Programme. Aging and aged care. Accessed from | Transition Care setting<ref>Transition Care Programme. Aging and aged care. Accessed from | ||
☀https://agedcare.health.gov.au/programs-services/flexible-care/transition-care-programme on 4\12\19 | ☀https://agedcare.health.gov.au/programs-services/flexible-care/transition-care-programme on 4\12\19 | ||
</ref> improves the independence and functioning of the patients in order to delay their entry into residential aged care. provides time-limited, goal-oriented and therapy-focused packages of services to older people after a hospital stay which includes low-intensity therapy—such as physiotherapy and occupational therapy—social work and nursing support or personal care. A qualitative research study<ref>Lawler K, Taylor NF, Shields N. [https://www.sciencedirect.com/science/article/pii/S1836955319300566?via%3Dihub Family-assisted therapy empowered families of older people transitioning from hospital to the community: a qualitative study.] Journal of physiotherapy. 2019 Jun 13.</ref> suggests better outcomes in older patients (above 80yrs) with family participation to assist physiotherapy care in a transition care setting.<br> | </ref> improves the independence and functioning of the patients in order to delay their entry into residential aged care. It also provides time-limited, goal-oriented and therapy-focused packages of services to older people after a hospital stay, which includes low-intensity therapy—such as physiotherapy and occupational therapy—social work and nursing support or personal care. A qualitative research study<ref>Lawler K, Taylor NF, Shields N. [https://www.sciencedirect.com/science/article/pii/S1836955319300566?via%3Dihub Family-assisted therapy empowered families of older people transitioning from hospital to the community: a qualitative study.] Journal of physiotherapy. 2019 Jun 13.</ref> suggests better outcomes in older patients (above 80yrs) with family participation to assist physiotherapy care in a transition care setting.<br> | ||
{| width="400" cellspacing="1" cellpadding="1" border="0" align="center" | {| width="400" cellspacing="1" cellpadding="1" border="0" align="center" | ||
| Line 38: | Line 38: | ||
| {{#ev:youtube|e7dmw4Wuhzs|300}}<ref>National Parkinson Foundation. Ask the Helpline: Why is Exercise Important for People with Parkinson's?. Available from: http://www.youtube.com/watch?v=e7dmw4Wuhzs [last accessed 24/09/16] (LoE) </ref> | | {{#ev:youtube|e7dmw4Wuhzs|300}}<ref>National Parkinson Foundation. Ask the Helpline: Why is Exercise Important for People with Parkinson's?. Available from: http://www.youtube.com/watch?v=e7dmw4Wuhzs [last accessed 24/09/16] (LoE) </ref> | ||
|} | |} | ||
Physical activity, in particular aerobic exercise, might slow down the motor skill degeneration and depression. Furthermore, it increases the quality of life of patients with Parkinson's.<ref>Wu, P.L., Lee, M., & Huang, T.T. Effectiveness of physical activity on patients with depression and Parkinson's: a systematic review. PloS one, 2017:12(7), eo181515.</ref> A randomised controlled trial showed favourable outcomes with exercise and horticultural intervention programs for older adults with depression and memory problems<ref>Makizako H, Tsutsumimoto K, Makino K, Nakakubo S, Liu-Ambrose T, Shimada H. [https://pubmed.ncbi.nlm.nih.gov/31906021-exercise-and-horticultural-programs-for-older-adults-with-depressive-symptoms-and-memory-problems-a-randomized-controlled-trial/ Exercise and Horticultural Programs for Older Adults with Depressive Symptoms and Memory Problems: A Randomized Controlled Trial.] Journal of Clinical Medicine. 2020 Jan;9(1):99.</ref>. | Physical activity, in particular aerobic exercise, might slow down the motor skill degeneration and depression that occurs in Parkinson's Disease. Furthermore, it increases the quality of life of patients with Parkinson's.<ref>Wu, P.L., Lee, M., & Huang, T.T. Effectiveness of physical activity on patients with depression and Parkinson's: a systematic review. PloS one, 2017:12(7), eo181515.</ref> A randomised controlled trial showed favourable outcomes with exercise and horticultural intervention programs for older adults with depression and memory problems<ref>Makizako H, Tsutsumimoto K, Makino K, Nakakubo S, Liu-Ambrose T, Shimada H. [https://pubmed.ncbi.nlm.nih.gov/31906021-exercise-and-horticultural-programs-for-older-adults-with-depressive-symptoms-and-memory-problems-a-randomized-controlled-trial/ Exercise and Horticultural Programs for Older Adults with Depressive Symptoms and Memory Problems: A Randomized Controlled Trial.] Journal of Clinical Medicine. 2020 Jan;9(1):99.</ref>. | ||
A randomised controlled clinical trial protocol to evaluate the effect of inspiratory muscle training on respiratory function in patients with mild-to-moderate Parkinson's suggests that inspiratory muscle training improves respiratory muscle strength, lung function, thoracic mobility and functional capacity.<ref>Montero Ferro A, P. Basso‐Vanelli R, Moreira Mello RL, Sanches Garcia‐Araujo A, Gonçalves Mendes R, Costa D, Gianlorenço AC. [https://www.ncbi.nlm.nih.gov/pubmed/31090181 Effects of inspiratory muscle training on respiratory muscle strength, lung function, functional capacity and cardiac autonomic function in Parkinson's disease: Randomized controlled clinical trial protocol]. Physiotherapy Research International. 2019 May 14:e1777.</ref> Similarly, a systematic review of research on the application of Respiratory Muscle Strength Training to Parkinson's Disease rehabilitation found that respiratory muscle training is a useful therapy for managing decreased respiratory muscles, dysphagia, ineffective coughing, speech disorders, and cardiorespiratory dysfunction in people with Parkinson's, with prolonged positive impact on respiratory muscle strength, swallowing function, and cardiovascular autonomic function.<ref>Zhuang, J. and Jia, J. (2022) “Effects of respiratory muscle strength training on respiratory-related impairments of parkinson's disease,” ''Frontiers in Aging Neuroscience'', 14. Available at: <nowiki>https://doi.org/10.3389/fnagi.2022.929923</nowiki>.</ref> | |||
Quality of life may be increased when performing strength training against an external resistance. Examples of such resistance exercises include: cycle ergometer, weight machines, therapeutic putty, elastic and, weight cuffs. Strength training can also improve physical parameters such as balance, gait, and physical performance. <ref>Ramazzina, I., Bernazzoli, B.,& Costantino, C. Systematic review on strength training in Parkinson's: an unsolved question. Clinical interventions in aging, 2017;12, 619.</ref> | Quality of life may be increased when performing strength training against an external resistance. Examples of such resistance exercises include: cycle ergometer, weight machines, therapeutic putty, elastic and, weight cuffs. Strength training can also improve physical parameters such as balance, gait, and physical performance. <ref>Ramazzina, I., Bernazzoli, B.,& Costantino, C. Systematic review on strength training in Parkinson's: an unsolved question. Clinical interventions in aging, 2017;12, 619.</ref> | ||
Executing a dual task (e.g. talking while walking) is often difficult in patients with Parkinson's. Training with motor-cognitive dual-task training improves dual-task ability and might improve gait, balance and cognition. <ref>Fritz, N.E., Cheek, F.M., & Nichols-Larsen, d.S. Motor-cognitive dual-task training in neurologic disorders: a systematic review. Journal of neurologic physical therapy: JNPT, 2015;39(3), 142.</ref>A 2021 study found that dual task training can improve gait performance, most notably increasing gait velocity, step length, and decreased freezing of gait in elderly patients. This study also found dual task training improved the physical well-being of the study participants.<ref>Wollesen B, Rudnik S, Gulberti A, Cordes T, Gerloff C, Poetter-Nerger M. [https://www.nature.com/articles/s41598-021-91858-0 A feasibility study of dual-task strategy training to improve gait performance in patients with Parkinson’s disease]. Scientific Reports. 2021 Jun 14;11(1):1-0.</ref> | Executing a dual task (e.g. talking while walking) is often difficult in patients with Parkinson's. Training with motor-cognitive dual-task training improves dual-task ability and might improve gait, balance and cognition. <ref>Fritz, N.E., Cheek, F.M., & Nichols-Larsen, d.S. Motor-cognitive dual-task training in neurologic disorders: a systematic review. Journal of neurologic physical therapy: JNPT, 2015;39(3), 142.</ref>A 2021 study found that dual task training can improve gait performance, most notably increasing gait velocity, step length, and decreased freezing of gait in elderly patients. This study also found dual task training improved the physical well-being of the study participants.<ref>Wollesen B, Rudnik S, Gulberti A, Cordes T, Gerloff C, Poetter-Nerger M. [https://www.nature.com/articles/s41598-021-91858-0 A feasibility study of dual-task strategy training to improve gait performance in patients with Parkinson’s disease]. Scientific Reports. 2021 Jun 14;11(1):1-0.</ref> | ||
Revision as of 07:22, 8 November 2022
Original Editor - Bhanu Ramaswamy as part of the APPDE Project
Top Contributors - Laura Ritchie, Kim Jackson, Wendy Walker, Mariam Hashem, Vidya Acharya, Ewa Jaraczewska, Rachael Lowe, Tony Lowe, Evan Thomas, Tarina van der Stockt, Lauren Lopez, Lenaertz Kiara, Admin, Stacy Schiurring, Oyemi Sillo, Naomi O'Reilly, WikiSysop, Simisola Ajeyalemi, Claire Knott and Lucinda hampton
Introduction[edit | edit source]
A person with Parkinson’s may be experiencing several symptoms at the same time; your history taking and physical assessment should elicit the main issue(s) to prioritise as part of the management strategy. While physiotherapy concentrates on the physical manifestations of a disorder, it is also important to pay attention to how other symptoms impact upon the person’s lifestyle.
Remember also that optimal outcome is achieved through the collaboration with others from a team of health and social care professionals with expertise in other domains of Parkinson’s, from volunteers to family and friends.
Aims of Physiotherapy[edit | edit source]
- Maintain and improve levels of function and independence, which will help to improve a person’s quality of life
- Use exercise and movement strategies to improve mobility
- Correct and improve abnormal movement patterns and posture, where possible
- Maximise muscle strength and joint flexibility
- Correct and improve posture and balance, and minimise risks of falls
- Maintain a good breathing pattern and effective cough
- Educate the person with Parkinson’s and their care-giver or family members
- Enhance the effects of drug therapy
Physiotherapy Intervention[edit | edit source]
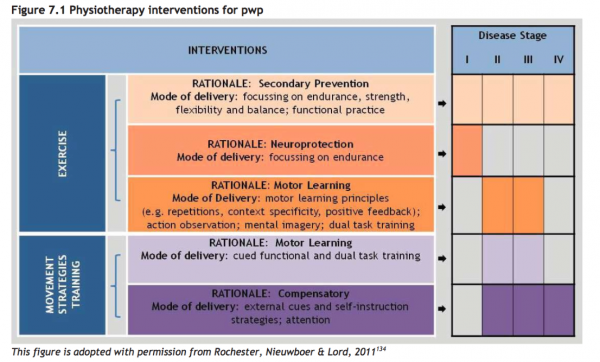
The Review version of the European Physiotherapy Guideline divides physiotherapy intervention for Parkinson’s into exercise and movement strategy training.
Exercise[edit | edit source]
Exercise has been proven to maintain health and well-being in Parkinson’s, and now importantly it is shown to play a big role in addressing secondary prevention (focusing on strength, endurance, flexibility, functional practice and balance). Exercise for neuroprotection focuses on endurance and uses motor learning principles approaches, such as mental imagery and dual task training. Neuroprotection training, to be effective, should be introduced in the early stages but helps at all stages. It involves complex, powerful and intensive exercises.
Exercise undertaken in a group setting has the added value of providing a social connection to those becoming increasingly isolated as the condition progresses, and those who are newly diagnosed are able to observe the benefits of maintaining exercise and activity. A group environment also permits time for people to ask questions and discuss their symptoms and own management strategies with one another.
Transition Care setting[1] improves the independence and functioning of the patients in order to delay their entry into residential aged care. It also provides time-limited, goal-oriented and therapy-focused packages of services to older people after a hospital stay, which includes low-intensity therapy—such as physiotherapy and occupational therapy—social work and nursing support or personal care. A qualitative research study[2] suggests better outcomes in older patients (above 80yrs) with family participation to assist physiotherapy care in a transition care setting.
| [3] |
Physical activity, in particular aerobic exercise, might slow down the motor skill degeneration and depression that occurs in Parkinson's Disease. Furthermore, it increases the quality of life of patients with Parkinson's.[4] A randomised controlled trial showed favourable outcomes with exercise and horticultural intervention programs for older adults with depression and memory problems[5].
A randomised controlled clinical trial protocol to evaluate the effect of inspiratory muscle training on respiratory function in patients with mild-to-moderate Parkinson's suggests that inspiratory muscle training improves respiratory muscle strength, lung function, thoracic mobility and functional capacity.[6] Similarly, a systematic review of research on the application of Respiratory Muscle Strength Training to Parkinson's Disease rehabilitation found that respiratory muscle training is a useful therapy for managing decreased respiratory muscles, dysphagia, ineffective coughing, speech disorders, and cardiorespiratory dysfunction in people with Parkinson's, with prolonged positive impact on respiratory muscle strength, swallowing function, and cardiovascular autonomic function.[7]
Quality of life may be increased when performing strength training against an external resistance. Examples of such resistance exercises include: cycle ergometer, weight machines, therapeutic putty, elastic and, weight cuffs. Strength training can also improve physical parameters such as balance, gait, and physical performance. [8]
Executing a dual task (e.g. talking while walking) is often difficult in patients with Parkinson's. Training with motor-cognitive dual-task training improves dual-task ability and might improve gait, balance and cognition. [9]A 2021 study found that dual task training can improve gait performance, most notably increasing gait velocity, step length, and decreased freezing of gait in elderly patients. This study also found dual task training improved the physical well-being of the study participants.[10]
A recent research study found out progressive resistance training (PRT) to be effective in decreasing bradykinesia and improving functional performance in patients with mild-to-moderate Parkinson's Disease (PD)[11]. A 2022 meta-analysis found that progressive resistance training in persons with Parkinson's improved freezing of gait, increased muscle strength and improved reported quality of life during rehabilitation.[12]
Movement Strategy Training[edit | edit source]
Basal ganglia disorders cause deficits in the generation of internal (automatic) behavior. Strategies (physical or attentional cues and combined strategies) can help overcome some of the resultant problems, hence have become an increasingly utilised method of intervention for people with Parkinson’s.
Music-based movement therapy is a promising intervention that needs some further research. It is interesting since it combines cognitive movement strategies, cueing techniques, balance exercises and physical activity. The focus is on enjoying moving and not on the mobility limitation which might appeal more to the patients than standard exercises.[13]A 2021 systematic review and meta-analysis found that music-based movement therapy can significantly improve motor function, balance, freezing of gait, walking velocity, and overall mental health as measured by standarised tests. The review did not show music-based movement therapy having a measurable effect on gait cadence, stride length, or quality of life in persons with Parkinson's.[14]
We can see immediately the effects of external cueing and attention on improving step length, freezing and turning during walking tasks, and in activities of daily living. A Systematic Review and Meta-Analyses suggests better outcomes with short-term physiotherapy on the symptoms of freezing of gait in Parkison's patient. However, further randomized control trial studies are still needed[15]. Literature suggests that robot-assisted gait technology has better results in addressing the freezing of gait for Parkinson's patients. However, more research is needed in this field[16].
Depending on the cognitive state of the individual, they may be able to learn how to self-instruct in the use of an internal cue or strategy. If less able, the cue or strategy has to come from an external source e.g. a visual strip on the ground, the rhythmic beat of a metronome.
Depending on the stage of the condition, the rationale for intervention choices will differ:
This figure has been copied with permission of Rochester L, Nieuwboer A, Lord S [17].
As mentioned in the subsection on Physiotherapy for Parkinson’s: referral and assessment, during the earlier stages of diagnosis, greater emphasis is placed on education and self-management. The individual should be encouraged to continue being active and participate in physical exercise for as long as possible. Significant respiratory complications develop in many people as their Parkinson’s progresses, so attention should be paid to monitor and manage encroaching weakness of respiratory muscles and rigidity of the thoracic cage.
The European Guideline provides a section that describes the use of motor learning (pages 78 to 80), expectations if practiced and executed as a strategy to train improvements in movement. It takes the form of cued functional and dual task training, compensatory strategy training uses external cues, self-instruction and attention. Examples include:
- Visual cueing – a focus point to step over and initiate gait; strips of tape on the floor to initiate or continue walking through areas that cause slowing or freezing
- Auditory cueing – counting 1-2-3 to initiate walking; stepping to the beat of a metronome or specific music at a specified cadence to continue the rhythm of a walk
- Attention – Thinking about taking a big step; making a wider arc turn. This is applicable in case of correcting a bad habit- such as walking with stiff hip or hip hiking.
- Proprioceptive cueing – rocking from side to side ready to initiate a step; taking one step backwards as a cue ready to then walk forwards
A Systematic Review of thirty-five studies by Delgado-Alvarado M et al. emphasizes the benefit of non-pharmacological and nonsurgical treatments for freezing of gait symptoms. The study results suggest passive therapies (transcranial magnetic stimulation or transcranial direct current stimulation), active therapies (cognitive or physical training), and the transient effect therapies (using visual, auditory, or proprioceptive cues to shift the patient's habitual movements to a goal-directed one) help to overcome the freezing of gait episode[18].
Most people who are diagnosed with Parkinson’s are aged 50 or over, but 1 in 20 of those diagnosed are younger than this. Those with young onset of Parkinson’s are more likely to exhibit early dystonia and motor fluctuations and dyskinesias, caused by prolonged use of dopaminergic treatment.
These non-pharmalogical interventions are effective in increasing the Health-Related quality of life (HRQOL) according to Lee's meta-analysis. But since there is a big heterogenity between the interventions, more research is needed to take firm conclusions.[19]
To deliver a patient-centered treatment, it's important to provide your patients with information and education and allow time for patients to discuss their options and ask questions. Limited clinical time may be a challenge, however, good communication and sharing information are as important as delivering an intervention.
Complimentary Technology[edit | edit source]
Using virtual reality in rehabilitation has positive outcomes on balance, co-ordination and gait speed in Parkinson's patients[20]
Example of a man using visual cues to improve his walking.
| [21] |
The phenomena of using blue tints for dyskinesia
| [22] |
Using GaitAid
| [23] |
| [24] | [25] | [26] |
| [27] | [28] | [29] |
| [30] | [31] | [32] |
Related pages[edit | edit source]
- Parkinson's
- Parkinson's - Clinical Presentation
- Parkinson's - Anatomy, Pathology, Prognosis and Diagnosis
- Parkinson's - Physiotherapy Referral and Assessment
- Key Evidence and resources
References[edit | edit source]
- ↑ Transition Care Programme. Aging and aged care. Accessed from ☀https://agedcare.health.gov.au/programs-services/flexible-care/transition-care-programme on 4\12\19
- ↑ Lawler K, Taylor NF, Shields N. Family-assisted therapy empowered families of older people transitioning from hospital to the community: a qualitative study. Journal of physiotherapy. 2019 Jun 13.
- ↑ National Parkinson Foundation. Ask the Helpline: Why is Exercise Important for People with Parkinson's?. Available from: http://www.youtube.com/watch?v=e7dmw4Wuhzs [last accessed 24/09/16] (LoE)
- ↑ Wu, P.L., Lee, M., & Huang, T.T. Effectiveness of physical activity on patients with depression and Parkinson's: a systematic review. PloS one, 2017:12(7), eo181515.
- ↑ Makizako H, Tsutsumimoto K, Makino K, Nakakubo S, Liu-Ambrose T, Shimada H. Exercise and Horticultural Programs for Older Adults with Depressive Symptoms and Memory Problems: A Randomized Controlled Trial. Journal of Clinical Medicine. 2020 Jan;9(1):99.
- ↑ Montero Ferro A, P. Basso‐Vanelli R, Moreira Mello RL, Sanches Garcia‐Araujo A, Gonçalves Mendes R, Costa D, Gianlorenço AC. Effects of inspiratory muscle training on respiratory muscle strength, lung function, functional capacity and cardiac autonomic function in Parkinson's disease: Randomized controlled clinical trial protocol. Physiotherapy Research International. 2019 May 14:e1777.
- ↑ Zhuang, J. and Jia, J. (2022) “Effects of respiratory muscle strength training on respiratory-related impairments of parkinson's disease,” Frontiers in Aging Neuroscience, 14. Available at: https://doi.org/10.3389/fnagi.2022.929923.
- ↑ Ramazzina, I., Bernazzoli, B.,& Costantino, C. Systematic review on strength training in Parkinson's: an unsolved question. Clinical interventions in aging, 2017;12, 619.
- ↑ Fritz, N.E., Cheek, F.M., & Nichols-Larsen, d.S. Motor-cognitive dual-task training in neurologic disorders: a systematic review. Journal of neurologic physical therapy: JNPT, 2015;39(3), 142.
- ↑ Wollesen B, Rudnik S, Gulberti A, Cordes T, Gerloff C, Poetter-Nerger M. A feasibility study of dual-task strategy training to improve gait performance in patients with Parkinson’s disease. Scientific Reports. 2021 Jun 14;11(1):1-0.
- ↑ de Moraes Filho AV, Chaves SN, Martins WR, Tolentino GP, Homem RD, de Farias GL, Fischer BL, Oliveira JA, Pereira SK, Vidal SE, Mota MR. Progressive Resistance Training Improves Bradykinesia, Motor Symptoms and Functional Performance in Patients with Parkinson’s Disease. Clinical Interventions in Aging. 2020;15:87.
- ↑ Yang X, Wang Z. Effectiveness of Progressive Resistance Training in Parkinson’s Disease: A Systematic Review and Meta-Analysis. European Neurology. 2022 Oct 20:1-9.
- ↑ de Dreu, M. J., Van Der Wilk, A. S; d;, Poppe, E., Kwakkel, G., & van Wegen, E. E. Rehabilitation, exercise therapy and music in patients with Parkinson's: a meta-analysis of the effects of music-based movement therapy on walking ability, balance and quality of life. Parkinsonism & related disorders,2012; 18, S114-S119.
- ↑ Zhou Z, Zhou R, Wei W, Luan R, Li K. Effects of music-based movement therapy on motor function, balance, gait, mental health, and quality of life for patients with Parkinson’s disease: A systematic review and meta-analysis. Clinical Rehabilitation. 2021 Jul;35(7):937-51.
- ↑ Cosentino C, Baccini M, Putzolu M, Ristori D, Avanzino L, Pelosin E. Effectiveness of Physiotherapy on Freezing of Gait in Parkinson's Disease: A Systematic Review and Meta‐Analyses. Movement Disorders. 2019 Dec 4.
- ↑ Alwardat M, Etoom M. Effectiveness of robot-assisted gait training on freezing of gait in people with Parkinson disease: evidence from a literature review. Journal of exercise rehabilitation. 2019 Apr;15(2):187.
- ↑ Rochester L, Nieuwboer A, Lord S. Physiotherapy for Parkinson’s disease: Defining evidence within a framework for intervention. Neurodegen Dis Man 2011; 1: 57 - 65
- ↑ Delgado‐Alvarado M, Marano M, Santurtún A, Urtiaga‐Gallano A, Tordesillas‐Gutierrez D, Infante J. Nonpharmacological, Nonsurgical Treatments for Freezing of Gait in Parkinson's Disease: A Systematic Review. Movement Disorders. 2019 Nov 26.
- ↑ Lee, J., Choi, M., & Yoo, Y. A Meta-analysis of nonpharmacological Interventions for People With Parkinson's. Clinical nursing research, 2017;26(5), 608-631.
- ↑ Triegaardt J, Han TS, Sada C, Sharma S, Sharma P. The role of virtual reality on outcomes in rehabilitation of Parkinson’s disease: meta-analysis and systematic review in 1031 participants. Neurological Sciences. 2019 Dec 6:1-8.
- ↑ Oxford Computer Consultants. Virtual Reality Glasses for people with Parkinson's (Paper Cues). Available from: http://www.youtube.com/watch?v=yKSJQ_f9cjM [last accessed 24/09/16] (LoE:5)
- ↑ RevZonenet. Dyskinesia and Blue Lenses - RevZone. Available from: http://www.youtube.com/watch?v=h3y13erwfxw [last accessed 24/09/16] (LoE:5)
- ↑ Amir Baram. Parkinson's Freezing improves walking with the GaitAid. Available from: http://www.youtube.com/watch?v=6XoHBqw8GnI [last accessed 24/09/16] (LoE:5)
- ↑ TouroInfirmary. LSVT Big & Loud Parkinson's Therapy at Touro Neuro Rehab Center. Available from: http://www.youtube.com/watch?v=9fUQ6jptaBY [last accessed 29/09/16]
- ↑ Advance Rehab Centre. LSVT Big. Available from: http://www.youtube.com/watch?v=3jPEtanYmI0 [last accessed 29/09/16]
- ↑ UStepWalker. The U-Step 2 Walker, a Parkinson's Therapy Aid. Available from: http://www.youtube.com/watch?v=mirtZhHJSB4 [last accessed 29/09/16]
- ↑ Parkinson's Dance: People with Parkinson's can;t do that..can they? Available from: http://www.youtube.com/watch?v=pL_LZgAEsnM [last accessed 29/09/16]
- ↑ SusieG5678. Dancing Feet Help Defeat Parkinson's. Available from: http://www.youtube.com/watch?v=koaA1T0MynM [last accessed 29/09/16]
- ↑ Tom Anthony. Dancing helps Parkinson's Patients. Available from: http://www.youtube.com/watch?v=UEAaWPHDRbk [last accessed 29/09/16]
- ↑ 205beers. Exercise program for Parkinson disease. Available from: http://www.youtube.com/watch?v=YEiupqJDugA [last accessed 29/09/16]
- ↑ captainpat. Parkinson's - Vigorous Exercise. Neil Sligar June 2011. Available from: http://www.youtube.com/watch?v=R_-nRQmO8ko [last accessed 29/09/16]
- ↑ Polestar Pilates. Polestar Pilates for Parkinson's Patients. Available from: http://www.youtube.com/watch?v=yWBn0Ozt2fU [last accessed 29/09/16]