Pain Neuroscience Education (PNE)
Original Editor - David Greaves, Lynette Fox, and Katie White as part of the Nottingham University Spinal Rehabilitation Project
Top Contributors - David Greaves, Lynette Fox, Becky Mead, Katie White, Kim Jackson, Maram Salem, Lucinda hampton, Uchechukwu Chukwuemeka, Vanessa Rhule, Rachael Lowe, Lauren Lopez, Evan Thomas and Rishika Babburu
Page Owner - Ina Diener as part of the One Page Project
Introduction[edit | edit source]
Pain neuroscience education (PNE) is a strategy that teaches patients to rethink the way they view pain. Pain neuroscience education utilises various stories and metaphors to help patients reconceptualise their pain experience. Clinicians may often underestimate the ability of a patient to understand the complexities of pain, as they are generally invested in learning about how to treat their pain[1].
PNE aims to increase pain thresholds during exercise, decrease fear related to movement and decreased brain activity in brain regions associated with pain. In practice, this often includes the use of educational pain analogies, re-education of patient misconceptions regarding disease pathogenesis and guidance about lifestyle and movements modifications that can be introduced.
Based on a large number of high-quality studies, it has been shown that teaching people with pain more about the neuroscience of their pain produces some impressive immediate and long-term changes. PNE has been shown to have positive effects in reducing pain, disability, and psychosocial problems, improving patient's knowledge of pain mechanisms, facilitating movement and decreasing healthcare consumption.[2]
Pain Neuroscience Education[edit | edit source]
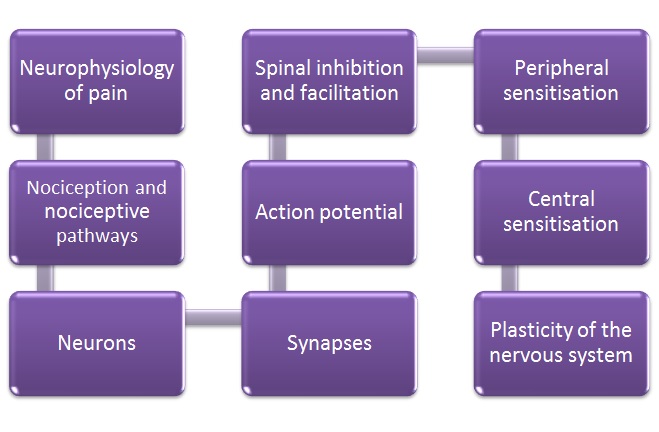
PNE consists of educational sessions for patients describing in detail the neurobiology and neurophysiology of pain and pain processing by the nervous system.[3] This educational approach has been used by physiotherapists therapeutically since 2002 in various countries (eg UK, US, Australia) and differs considerably from traditional education strategies such as back school and biomechanical models.[4]
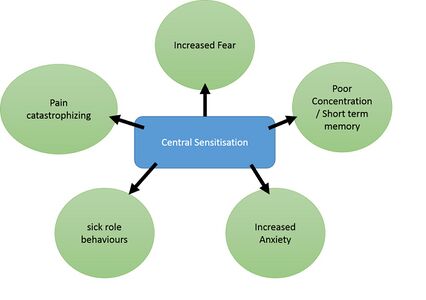
Chronic pain in PNE is seen as not being caused not by unhealthy or dysfunctional tissues but brain plasticity leading to hyper-excitability of the central nervous system, known as central sensitisation.[5]
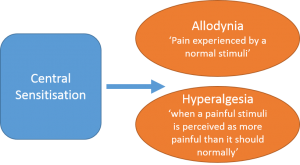
Central sensitisation is defined as an increased responsiveness of nociceptors in the central nervous system to either normal or sub-threshold afferent input resulting in:
- Hypersensitivity to stimuli.
- Responsiveness to non-noxious stimuli.
- Increased pain response evoked by stimuli outside the area of injury, an expanded receptive field.
Application[edit | edit source]
The application of PNE is most useful as part of a combination therapy for chronic pain that includes physiotherapy intervention (including exercise therapy) and may or may not include pharmacological treatment. Its application is best applied by trained and skilled clinicians with experience in managing patients with chronic pain conditions. Overall PNE serves as a method of reconceptualising a patient's perception of their pain experience, providing an avenue for reducing pain, disability and improving quality of life[1].
- eg A patient may have believed that damaged tissues were the main cause for their pain, and by receiving education about pain neurophysiology the patient understands that pain may not correctly represent the health of the tissue, but may be due to extra-sensitive nerves. As a result, patients have been found to have a reduction in fear avoidance behaviours and are more able and willing to move.[5]
This is a good 4 minute video explaining PNE
What is Pain[edit | edit source]
Mosely (2007) describes pain in a reconceptualised manner:
- Pain does not provide a measure of the state of the tissues
- Pain is modulated by many factors from somatic, psychological and social domains
- The relationship between pain and the state of tissues becomes less predictable as pain persists
- Pain can be conceptualised as the conscious correlate of the implicit perception that tissue is in danger[1]
What Does PNE Involve?[edit | edit source]
PNE first of all puts the complex process of describing the nerves and brain into a format that is easy to understand for everyone; no matter whether the target audience is of a particular age, educational level or ethnic group.[3]
This is made possible by using simplified scientific language used with additional methods of presenting information that may include the use of:
• Simple pictures
• Examples
• Booklets
• Metaphors
• Drawings
• Workbook with reading/question-answer assignments
• Neurophysiology Pain Questionnaires
Methods of PNE delivery vary but can typically involve around 4 hours of teaching that is provided to a group or individually, either in single or multiple sessions.[4]
Figure 6. showing the content of PNE education sessions with patients[3]
How is PNE Used in Clinical Practice?[edit | edit source]
A metaphor/story that can be found here: (http://www.instituteforchronicpain.org/treating-common-pain/what-is-pain-management/therapeutic-neuroscience-education) is used by Louw et al.[7] in clinical practice to teach patients about complex pain physiology including extra-sensitive nerves, inflammation, injury and how pain is created in the brain. It is such an example that helps patient to break away from a view of a particular tissue being the issue (e.g. generative disc) and helps the patient think towards the problem being related to pain and a sensitive nervous system.[7] Therefore, Instead of pain following spinal surgery being seen as the ‘problem has not resolved’ or ‘there is something still wrong with the disc’, PNE would explain pain is sensitive to act as a protector which is perfectly normal after surgery.
Indicators For the Use of PNE[edit | edit source]
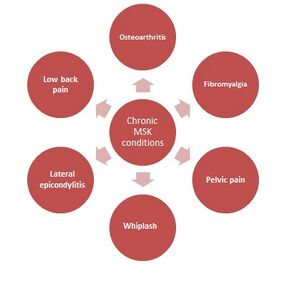
Chronic Musculoskeletal Conditions[8][edit | edit source]
These conditions are often characterised by brain plasticity that leads to hyperexcitability of the central nervous system (central sensitisation).
- PNE is recommended in
central sensitisation conditions like these,
as the patient may present with maladaptive
cognitions, behaviour, or coping
strategies in response to pain. - Typically they acquire a protective (movement-related) pain memory, which causes a barrier to adhere to therapeutic treatment such as exercise, decreasing the likelihood of a good outcome.
- Therefore these maladaptive behaviours, central sensitisation and previous failed treatments are all indicators for PNE
- Evidence showing benefits for pre op MSK patients.[7][9]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Project Physio PNE Available:https://www.project-physio.com/pain-neuroscience-education (accessed 19.4.2022)
- ↑ Zimney KJ, Louw A, Cox T, Puentedura EJ, Diener I. Pain neuroscience education: Which pain neuroscience education metaphor worked best?. South African Journal of Physiotherapy. 2019 Jan 1;75(1):1-7. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6739553/(accessed 19.4.2022)
- ↑ 3.0 3.1 3.2 Louw A, Diener I, Butler DS, Puentedura EJ. The effect of neuroscience education on pain, disability, anxiety, and stress in chronic musculoskeletal pain. Archives of physical medicine and rehabilitation. 2011; 92(12):2041-2056.
- ↑ 4.0 4.1 Clarke CL, Ryan CG, Martin DJ. Pain neurophysiology education for the management of individuals with chronic low back pain: A systematic review and meta-analysis. Manual therapy. 2011; 16(6):544-549.
- ↑ 5.0 5.1 Nijs J, Girbés EL, Lundberg M, Malfliet A, Sterling M. Exercise therapy for chronic musculoskeletal pain: Innovation by altering pain memories. Manual therapy. 2015; 20 (1): 216-220.
- ↑ Pain Neuroscience Education PAINWeek Available:https://www.youtube.com/watch?v=6RGP_usIbBU (accessed 19.4.2022)
- ↑ 7.0 7.1 7.2 Louw A, Diener I, Landers MR, Puentedura EJ. Preoperative pain neuroscience education for lumbar radiculopathy: a multicenter randomized controlled trial with 1-year follow-up. Spine. 2014; 39(18):1449-1457.
- ↑ Moseley GL, Butler DS. Fifteen years of explaining pain: the past, present, and future. The Journal of Pain. 2015;16(9):807-813.
- ↑ Zimney K, Louw A, Puentedura EJ. Use of Therapeutic Neuroscience Education to address psychosocial factors associated with acute low back pain: a case report. Physiotherapy theory and practice. 2014; 30(3):202-209.
Keller T and Krames ES. (2009). “On the Shoulders of Giants”: A History of the Understandings of Pain, Leading to the Understandings of Neuromodulation. Neuromodulation. 12 (2), 77-84.