Pain Neuroscience Education (PNE): Difference between revisions
Maram Salem (talk | contribs) No edit summary |
Maram Salem (talk | contribs) No edit summary |
||
| Line 12: | Line 12: | ||
== Introduction == | == Introduction == | ||
[[File:Pain | [[File:Pain areas.jpg|right|frameless]] | ||
Chronic pain is defined as pain that lasts more than three months. It is a very common and prevalent problem that affects most age groups worldwide. Chronic pain is a multifactorial disorder that is influenced by biology, psychology, environmental, and social factors.<ref>Mills SEE, Nicolson KP, Smith BH. Chronic pain: a review of its epidemiology and associated factors in population-based studies. Br J Anaesth. 2019 Aug;123(2):e273-e283.</ref> Pain Neuroscience Education (PNE) is a strategy that aims to teach patients to reshape their mindset and perception of [[Pain Behaviours|pain]] despite these factors. It provides patients a better understanding of their condition and motivates them to become active participants in their treatment programs. | Chronic pain is defined as pain that lasts more than three months. It is a very common and prevalent problem that affects most age groups worldwide. Chronic pain is a multifactorial disorder that is influenced by biology, psychology, environmental, and social factors.<ref>Mills SEE, Nicolson KP, Smith BH. Chronic pain: a review of its epidemiology and associated factors in population-based studies. Br J Anaesth. 2019 Aug;123(2):e273-e283.</ref> Pain Neuroscience Education (PNE) is a strategy that aims to teach patients to reshape their mindset and perception of [[Pain Behaviours|pain]] despite these factors. It provides patients a better understanding of their condition and motivates them to become active participants in their treatment programs. | ||
Based on a large number of high-quality studies, it has been shown that teaching people with chronic pain more about the neuroscience of their pain produces immediate and long-term changes. PNE has been shown to have positive effects in reducing pain, disability, and psychosocial problems, improving patient's knowledge of pain mechanisms, facilitating movement and decreasing healthcare consumption.<ref>Zimney KJ, Louw A, Cox T, Puentedura EJ, Diener I. Pain neuroscience education: Which pain neuroscience education metaphor worked best?. South African Journal of Physiotherapy. 2019 Jan 1;75(1):1-7. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6739553/<nowiki/>(accessed 19.4.2022)</ref> | Based on a large number of high-quality studies, it has been shown that teaching people with chronic pain more about the neuroscience of their pain produces immediate and long-term changes. PNE has been shown to have positive effects in reducing pain, disability, and psychosocial problems, improving patient's knowledge of pain mechanisms, facilitating movement and decreasing healthcare consumption.<ref>Zimney KJ, Louw A, Cox T, Puentedura EJ, Diener I. Pain neuroscience education: Which pain neuroscience education metaphor worked best?. South African Journal of Physiotherapy. 2019 Jan 1;75(1):1-7. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6739553/<nowiki/>(accessed 19.4.2022)</ref> | ||
== Pain Neuroscience Education == | == Pain Neuroscience Education == | ||
With respect to PNE, [[Chronic Pain and the Brain|chronic pain]] is not viewed as a result of unhealthy or dysfunctional tissues. Rather, it is due to [[Neuroplasticity|brain plasticity]] leading to hyper-excitability of the central nervous system, known as central sensitization.<ref name=":1">Nijs J, Girbés EL, Lundberg M, Malfliet A, Sterling M. Exercise therapy for chronic musculoskeletal pain: Innovation by altering pain memories. Manual therapy. 2015; 20 (1): 216-220.</ref> The ultimate goal for Pain Neuroscience Education (PNE) is to increase pain tolerance with movement (e.g., be able to perform exercise with mild discomfort), reduce any fear associated with movement, and reduce central nervous system hypersensitivity. In practice, this often includes the use of educational pain analogies, re-education of patient misconceptions regarding disease pathogenesis, and guidance about lifestyle and movements modifications that can be introduced. | |||
There are two clinical indications for initiating Pain Neuroscience Education (PNE)<ref>Nijs, J., Paul van Wilgen, C., Van Oosterwijck, J., van Ittersum, M., Meeus, M.,How to explain central sensitization to patients with ‘unexplained’ chronic musculoskeletal pain: Practice guidelines, | There are two clinical indications for initiating Pain Neuroscience Education (PNE)<ref>Nijs, J., Paul van Wilgen, C., Van Oosterwijck, J., van Ittersum, M., Meeus, M.,How to explain central sensitization to patients with ‘unexplained’ chronic musculoskeletal pain: Practice guidelines, | ||
| Line 27: | Line 27: | ||
* the clinical picture is dominated by central sensitization | * the clinical picture is dominated by central sensitization | ||
* illness coping mechanisms or poor illness perception is present | * illness coping mechanisms or poor illness perception is present | ||
[[Image:Effects_of_central_sensatisation.png|300x200px|alt=|thumb|Effects of central sensitization]]Central sensitization is when there is amplification of pain in the central nervous system. It can result in hypersensitivity to stimuli, responsiveness to non-noxious stimuli, and increased pain response evoked by stimuli outside the area of injury, an expanded receptive field. <ref>[[Central Sensitisation]]</ref>This can be assessed during the subjective and objective portion of a patient's evaluation. A physical therapist can determine what a patient's perception of their own pain is and how they cope with their pain. | |||
PNE consists of educational sessions for patients describing in detail the neurobiology and neurophysiology of pain and [[Pain Facilitation and Inhibition|pain processing]] by the [[Introduction to Neuroanatomy|nervous system]].<ref name=":10">Louw A, Diener I, Butler DS, Puentedura EJ. The effect of neuroscience education on pain, disability, anxiety, and stress in chronic musculoskeletal pain. Archives of physical medicine and rehabilitation. 2011; 92(12):2041-2056.</ref> It is implemented prior to administering physical therapy interventions with a verbal explanation. This is subsequently reinforced throughout the course of treatment with handouts or brochures for the patient's reference and in discussions with their therapist. This is to ensure proper carryover of reconceptualization of pain during and after discharge from physical therapy.[[File:Upload_version_of_systemic_effects.jpg|alt=|thumb|426x426px|Pain behaviors caused by central sensitization]]Mosely (2007) describes pain in a reconceptualized manner: | |||
PNE consists of educational sessions for patients describing in detail the neurobiology and neurophysiology of pain and [[Pain Facilitation and Inhibition|pain processing]] by the [[Introduction to Neuroanatomy|nervous system]].<ref name=":10">Louw A, Diener I, Butler DS, Puentedura EJ. The effect of neuroscience education on pain, disability, anxiety, and stress in chronic musculoskeletal pain. Archives of physical medicine and rehabilitation. 2011; 92(12):2041-2056.</ref> This | |||
[[File:Upload_version_of_systemic_effects.jpg|alt=|thumb|426x426px|Pain | |||
* Pain does not provide a measure of the state of the tissues | * Pain does not provide a measure of the state of the tissues | ||
* Pain is modulated by many factors from somatic, psychological and social domains | * Pain is modulated by many factors from somatic, psychological and social domains | ||
* The relationship between pain and the state of tissues becomes less predictable as pain persists | * The relationship between pain and the state of tissues becomes less predictable as pain persists | ||
* Pain can be | * Pain can be conceptualized as the conscious correlate of the implicit perception that tissue is in danger<ref name=":0" /> | ||
== Application == | == Application == | ||
The application of PNE is most useful as part of a combination therapy for chronic pain that includes physiotherapy intervention (including [[Therapeutic Exercise|exercise therapy]]) and may or may not include [[Pain Medications|pharmacological treatment]]. Its application is best applied by trained and skilled clinicians with experience in managing patients with chronic pain conditions. Overall PNE serves as a method of | The application of PNE is most useful as part of a combination therapy for chronic pain that includes physiotherapy intervention (including [[Therapeutic Exercise|exercise therapy]]) and may or may not include [[Pain Medications|pharmacological treatment]]. Its application is best applied by trained and skilled clinicians with experience in managing patients with chronic pain conditions. Overall PNE serves as a method of reconceptualizing a patient's perception of their pain experience, providing an avenue for reducing pain, disability and improving [[Quality of Life|quality of life]]<ref name=":0">Project Physio PNE Available:https://www.project-physio.com/pain-neuroscience-education (accessed 19.4.2022)</ref>. | ||
* eg A patient may have believed that damaged tissues were the main cause for their pain, and by receiving education about pain neurophysiology the patient understands that pain may not correctly represent the health of the tissue, but may be due to extra-sensitive nerves. As a result, patients have been found to have a reduction in fear avoidance behaviours and are more able and willing to move.<ref name=":1" /> | * eg A patient may have believed that damaged tissues were the main cause for their pain, and by receiving education about pain neurophysiology the patient understands that pain may not correctly represent the health of the tissue, but may be due to extra-sensitive nerves. As a result, patients have been found to have a reduction in fear avoidance behaviours and are more able and willing to move.<ref name=":1" /> | ||
| Line 56: | Line 49: | ||
This is made possible by using simplified scientific language used with additional methods of presenting information that may include the use of:<br>'''• Simple pictures<br>• Examples<br>• Booklets<br>• Metaphors<br>• Drawings<br>• Workbook with reading/question-answer assignments<br>• Neurophysiology Pain Questionnaires''' | This is made possible by using simplified scientific language used with additional methods of presenting information that may include the use of:<br>'''• Simple pictures<br>• Examples<br>• Booklets<br>• Metaphors<br>• Drawings<br>• Workbook with reading/question-answer assignments<br>• Neurophysiology Pain Questionnaires''' | ||
Methods of PNE delivery vary but can typically involve around 4 hours of teaching that is provided to a group or individually, either in single or multiple sessions.<ref name=":4" /> | Methods of PNE delivery vary but can typically involve around 4 hours of teaching that is provided to a group or individually, either in single or multiple sessions.<ref name=":4">Clarke CL, Ryan CG, Martin DJ. Pain neurophysiology education for the management of individuals with chronic low back pain: A systematic review and meta-analysis. Manual therapy. 2011; 16(6):544-549.</ref> | ||
Figure 6. showing the content of PNE education sessions with patients<ref name=":10" /><br> | Figure 6. showing the content of PNE education sessions with patients<ref name=":10" /><br> | ||
Revision as of 03:50, 18 November 2023
This article is currently under review and may not be up to date. Please come back soon to see the finished work! (18/11/2023)
Original Editor - David Greaves, Lynette Fox, and Katie White as part of the Nottingham University Spinal Rehabilitation Project
Top Contributors - David Greaves, Lynette Fox, Becky Mead, Katie White, Kim Jackson, Maram Salem, Lucinda hampton, Uchechukwu Chukwuemeka, Vanessa Rhule, Rachael Lowe, Lauren Lopez, Evan Thomas and Rishika Babburu
Introduction[edit | edit source]
Chronic pain is defined as pain that lasts more than three months. It is a very common and prevalent problem that affects most age groups worldwide. Chronic pain is a multifactorial disorder that is influenced by biology, psychology, environmental, and social factors.[1] Pain Neuroscience Education (PNE) is a strategy that aims to teach patients to reshape their mindset and perception of pain despite these factors. It provides patients a better understanding of their condition and motivates them to become active participants in their treatment programs.
Based on a large number of high-quality studies, it has been shown that teaching people with chronic pain more about the neuroscience of their pain produces immediate and long-term changes. PNE has been shown to have positive effects in reducing pain, disability, and psychosocial problems, improving patient's knowledge of pain mechanisms, facilitating movement and decreasing healthcare consumption.[2]
Pain Neuroscience Education[edit | edit source]
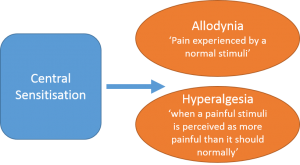
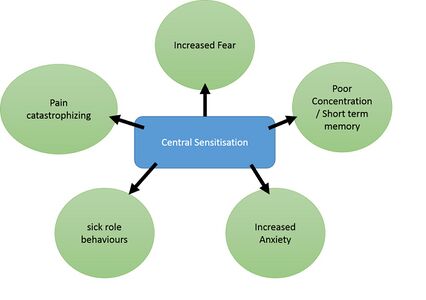
With respect to PNE, chronic pain is not viewed as a result of unhealthy or dysfunctional tissues. Rather, it is due to brain plasticity leading to hyper-excitability of the central nervous system, known as central sensitization.[3] The ultimate goal for Pain Neuroscience Education (PNE) is to increase pain tolerance with movement (e.g., be able to perform exercise with mild discomfort), reduce any fear associated with movement, and reduce central nervous system hypersensitivity. In practice, this often includes the use of educational pain analogies, re-education of patient misconceptions regarding disease pathogenesis, and guidance about lifestyle and movements modifications that can be introduced.
There are two clinical indications for initiating Pain Neuroscience Education (PNE)[4]:
- the clinical picture is dominated by central sensitization
- illness coping mechanisms or poor illness perception is present
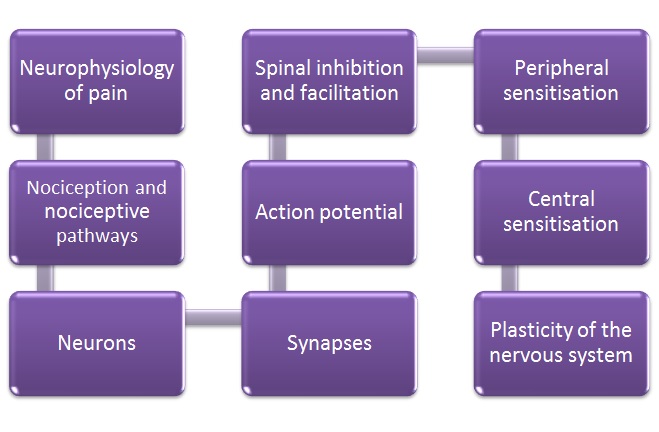
Central sensitization is when there is amplification of pain in the central nervous system. It can result in hypersensitivity to stimuli, responsiveness to non-noxious stimuli, and increased pain response evoked by stimuli outside the area of injury, an expanded receptive field. [5]This can be assessed during the subjective and objective portion of a patient's evaluation. A physical therapist can determine what a patient's perception of their own pain is and how they cope with their pain. PNE consists of educational sessions for patients describing in detail the neurobiology and neurophysiology of pain and pain processing by the nervous system.[6] It is implemented prior to administering physical therapy interventions with a verbal explanation. This is subsequently reinforced throughout the course of treatment with handouts or brochures for the patient's reference and in discussions with their therapist. This is to ensure proper carryover of reconceptualization of pain during and after discharge from physical therapy.
Mosely (2007) describes pain in a reconceptualized manner:
- Pain does not provide a measure of the state of the tissues
- Pain is modulated by many factors from somatic, psychological and social domains
- The relationship between pain and the state of tissues becomes less predictable as pain persists
- Pain can be conceptualized as the conscious correlate of the implicit perception that tissue is in danger[7]
Application[edit | edit source]
The application of PNE is most useful as part of a combination therapy for chronic pain that includes physiotherapy intervention (including exercise therapy) and may or may not include pharmacological treatment. Its application is best applied by trained and skilled clinicians with experience in managing patients with chronic pain conditions. Overall PNE serves as a method of reconceptualizing a patient's perception of their pain experience, providing an avenue for reducing pain, disability and improving quality of life[7].
- eg A patient may have believed that damaged tissues were the main cause for their pain, and by receiving education about pain neurophysiology the patient understands that pain may not correctly represent the health of the tissue, but may be due to extra-sensitive nerves. As a result, patients have been found to have a reduction in fear avoidance behaviours and are more able and willing to move.[3]
This is a good 4 minute video explaining PNE
What Does PNE Involve?[edit | edit source]
PNE first of all puts the complex process of describing the nerves and brain into a format that is easy to understand for everyone; no matter whether the target audience is of a particular age, educational level or ethnic group.[6]
This is made possible by using simplified scientific language used with additional methods of presenting information that may include the use of:
• Simple pictures
• Examples
• Booklets
• Metaphors
• Drawings
• Workbook with reading/question-answer assignments
• Neurophysiology Pain Questionnaires
Methods of PNE delivery vary but can typically involve around 4 hours of teaching that is provided to a group or individually, either in single or multiple sessions.[9]
Figure 6. showing the content of PNE education sessions with patients[6]
How is PNE Used in Clinical Practice?[edit | edit source]
A metaphor/story that can be found here: (http://www.instituteforchronicpain.org/treating-common-pain/what-is-pain-management/therapeutic-neuroscience-education) is used by Louw et al.[10] in clinical practice to teach patients about complex pain physiology including extra-sensitive nerves, inflammation, injury and how pain is created in the brain. It is such an example that helps patient to break away from a view of a particular tissue being the issue (e.g. generative disc) and helps the patient think towards the problem being related to pain and a sensitive nervous system.[10] Therefore, Instead of pain following spinal surgery being seen as the ‘problem has not resolved’ or ‘there is something still wrong with the disc’, PNE would explain pain is sensitive to act as a protector which is perfectly normal after surgery.
Indicators For the Use of PNE[edit | edit source]
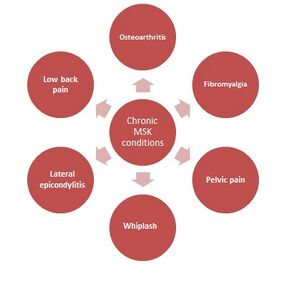
Chronic Musculoskeletal Conditions[11][edit | edit source]
These conditions are often characterised by brain plasticity that leads to hyperexcitability of the central nervous system (central sensitisation).
- PNE is recommended in
central sensitisation conditions like these,
as the patient may present with maladaptive
cognitions, behaviour, or coping
strategies in response to pain. - Typically they acquire a protective (movement-related) pain memory, which causes a barrier to adhere to therapeutic treatment such as exercise, decreasing the likelihood of a good outcome.
- Therefore these maladaptive behaviours, central sensitisation and previous failed treatments are all indicators for PNE
- Evidence showing benefits for pre op MSK patients.[10][12]
References[edit | edit source]
- ↑ Mills SEE, Nicolson KP, Smith BH. Chronic pain: a review of its epidemiology and associated factors in population-based studies. Br J Anaesth. 2019 Aug;123(2):e273-e283.
- ↑ Zimney KJ, Louw A, Cox T, Puentedura EJ, Diener I. Pain neuroscience education: Which pain neuroscience education metaphor worked best?. South African Journal of Physiotherapy. 2019 Jan 1;75(1):1-7. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6739553/(accessed 19.4.2022)
- ↑ 3.0 3.1 Nijs J, Girbés EL, Lundberg M, Malfliet A, Sterling M. Exercise therapy for chronic musculoskeletal pain: Innovation by altering pain memories. Manual therapy. 2015; 20 (1): 216-220.
- ↑ Nijs, J., Paul van Wilgen, C., Van Oosterwijck, J., van Ittersum, M., Meeus, M.,How to explain central sensitization to patients with ‘unexplained’ chronic musculoskeletal pain: Practice guidelines, Manual Therapy, Volume 16, Issue 5, 2011, Pages 413-418
- ↑ Central Sensitisation
- ↑ 6.0 6.1 6.2 Louw A, Diener I, Butler DS, Puentedura EJ. The effect of neuroscience education on pain, disability, anxiety, and stress in chronic musculoskeletal pain. Archives of physical medicine and rehabilitation. 2011; 92(12):2041-2056.
- ↑ 7.0 7.1 Project Physio PNE Available:https://www.project-physio.com/pain-neuroscience-education (accessed 19.4.2022)
- ↑ Pain Neuroscience Education PAINWeek Available:https://www.youtube.com/watch?v=6RGP_usIbBU (accessed 19.4.2022)
- ↑ Clarke CL, Ryan CG, Martin DJ. Pain neurophysiology education for the management of individuals with chronic low back pain: A systematic review and meta-analysis. Manual therapy. 2011; 16(6):544-549.
- ↑ 10.0 10.1 10.2 Louw A, Diener I, Landers MR, Puentedura EJ. Preoperative pain neuroscience education for lumbar radiculopathy: a multicenter randomized controlled trial with 1-year follow-up. Spine. 2014; 39(18):1449-1457.
- ↑ Moseley GL, Butler DS. Fifteen years of explaining pain: the past, present, and future. The Journal of Pain. 2015;16(9):807-813.
- ↑ Zimney K, Louw A, Puentedura EJ. Use of Therapeutic Neuroscience Education to address psychosocial factors associated with acute low back pain: a case report. Physiotherapy theory and practice. 2014; 30(3):202-209.
Keller T and Krames ES. (2009). “On the Shoulders of Giants”: A History of the Understandings of Pain, Leading to the Understandings of Neuromodulation. Neuromodulation. 12 (2), 77-84.