Osteoporotic Vertebral Fractures: Difference between revisions
No edit summary |
(Key research) |
||
| (23 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox">'''Original Editor '''- [[User:Mathieu Vanderroost|Mathieu Vanderroost]] | <div class="editorbox">'''Original Editor '''- [[User:Mathieu Vanderroost|Mathieu Vanderroost]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Definition / Description == | == Definition / Description == | ||
= | Osteoporotic (fragility) vertebral fractures (VFs) are fractures that result from mechanical forces that would not ordinarily result in a fracture. <ref name=":1">Yoo JH, Moon SH, Ha YC, Lee DY, Gong HS, Park SY, Yang KH. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4691591/ Osteoporotic Fracture: 2015 Position Statement of the Korean Society for Bone and Mineral Research.]J Bone Metab. 2015 Nov;22(4):175-81. 30. '''Level of Evidence: 2B.''' </ref> These types of fractures are [https://www.physio-pedia.com/Insufficiency_Fracture insufficiency fractures], caused by normal stresses on abnormal bone, often indicating [[Introduction to Frailty|frailty]]. | ||
== Classification of Vertebral Fractures == | |||
Classification of VFs has been described by '''<u>type of deformity</u>''' (wedge, biconcavity, or crush compression) and further by the <u>'''degree of deformity'''</u> (grades I, II). <ref name=":3">Eastell R, Cedel SL, Wahner HW, Riggs BL, Melton LJ III. [https://asbmr.onlinelibrary.wiley.com/doi/epdf/10.1002/jbmr.5650060302 Classification of vertebral fractures.] JBMR 1991; 6(3):207-15.</ref> <ref name=":2">Alexandru D, So W. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3523935/ Evaluation and Management of Vertebral Compression Fractures.] Perm J. 2012 Fall; 16(4): 46–51. </ref> | |||
[[File:Anterior-wedge-fracture-l1.jpg|thumb|X-Ray of an anterior wedge fracture. ]] | |||
* '''Wedge VFs''' are the most common, occuring in the midthoracic region with compression of the anterior segment of the vertebral body (VB) and the anterior longitudinal ligament (ALL), and reports of more than 50% of all VFs. <ref>Black DM, Arden NK, Palermo L, Pearson J, Cummings SR. [https://pubmed.ncbi.nlm.nih.gov/10320531/ Prevalent vertebral deformities predict hip fractures and new vertebral deformities but not wrist fractures.] Study of Osteoporotic Fractures Research Group. J Bone Miner Res. 1999 May;14(5):821–8. </ref> Wedge fractures do not involve the posterior half of the VB and do not involve the posterior osseous ligamentous complex. The former distinguishes a compression fracture from a burst fracture. | |||
* '''Biconcave compression VFs''' are the second-most common (approximately 17% of all VFs); here, only the middle portion of the vertebral body is collapsed, with no compromise of the anterior and posterior walls. <ref name=":2" /> | |||
* '''Crush compression VFs''' are the least common (13%), and are characterised by the collaplse of the entire anterior column, including anterior and posterior margins. <ref name=":2" /> | |||
* The remaining 20% of VFs may involve '''complex''' fractures of the spine. <ref name=":2" /> | |||
* Grade I refers to 3 SD < deformity < 4 SD and grade 2 deformity > 4 SD from the normal range for each vertebra. <ref name=":3" /> | |||
== Etiology == | |||
* The most common etiology of VFs is [[osteoporosis]], making these fractures the most common fragility fracture. <ref>Ettinger B, Black DM, Nevitt MC, Rundle AC, Cauley JA, Cummings SR, Genant HK. [https://pubmed.ncbi.nlm.nih.gov/1535172/ Contribution of vertebral deformities to chronic back pain and disability. The Study of Osteoporotic Fractures Research Group.] J Bone Miner Res. 1992 Apr;7(4):449-56.</ref><ref name="Griffith" /> | |||
* In contrast, vertebral compression fractures (VCFs) demonstrate a bimodal distribution with younger patients sustaining these injuries secondary to high energy mechanisms (fall from a height, MVA, etc.). | |||
* VFs occur secondary to an axial/compressive (and to a lesser extent, flexion) load with a resultant biomechanical failure of the bone resulting in a fracture. | |||
Watch this video analysing causes of VFs (including osteoporotic):{{#ev:youtube|https://www.youtube.com/watch?v=LILgFAEMAbg|width}}<ref>Spine live. Spinal compression fractures reasons. Available from: https://www.youtube.com/watch?v=LILgFAEMAbg [accessed 26/10/2023]</ref> | |||
== Epidemiology == | == Epidemiology == | ||
European population studies have shown that the annual incidence of VCFs is 10.7 per 1000 women and 5.7 per 1000 men. <ref>European Prospective Osteoporosis Study (EPOS) Group; Felsenberg D, Silman AJ, Lunt M, Armbrecht G, Ismail AA, Finn JD, Cockerill WC, Banzer D, Benevolenskaya LI, Bhalla A, Bruges Armas J, Cannata JB, Cooper C, Dequeker J, Eastell R, Felsch B, Gowin W, Havelka S, Hoszowski K, Jajic I, Janott J, Johnell O, Kanis JA, Kragl G, Lopes Vaz A, Lorenc R, Lyritis G, Masaryk P, Matthis C, Miazgowski T, Parisi G, Pols HA, Poor G, Raspe HH, Reid DM, Reisinger W, Schedit-Nave C, Stepan JJ, Todd CJ, Weber K, Woolf AD, Yershova OB, Reeve J, O'Neill TW. [https://pubmed.ncbi.nlm.nih.gov/11918229/ Incidence of vertebral fracture in europe: results from the European Prospective Osteoporosis Study (EPOS).] J Bone Miner Res. 2002 Apr;17(4):716-24. </ref> | |||
* VCFs are the most common fragility | * VCFs are the most common fragility fractures reported in the literature. <ref>Kutsal FY, Ergin Ergani GO. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8203169/ Vertebral compression fractures: Still an unpredictable aspect of osteoporosis.] Turk J Med Sci. 2021; 51(2): 393–399. | ||
* Approximately | |||
* | </ref> | ||
* Thoracolumbar junction (i.e., the segment from T12 to L2) location most often affected | * VCFs are common in Asian and Caucasian women, and less common in African-American women. <ref name=":2" /> | ||
* Approximately 1.5 million VCFs occur annually in the United States (US) alone in the general population. <ref>Barr JD, Barr MS, Lemley TJ, McCann RM. [https://pubmed.ncbi.nlm.nih.gov/10767803/ Percutaneous vertebroplasty for pain relief and spinal stabilization.] Spine (Phila Pa 1976). 2000 Apr 15;25(8):923-8.</ref> | |||
* | * Prevalence increases with age, and it is estimated that 40% to 50% of patients over age 80 years have sustained a VCF either acutely, or recognised incidentally during clinical workup for a separate condition.<ref>Black DM, Cummings SR, Karpf DB, Cauley JA, Thompson DE, Nevitt MC, Bauer DC, Genant HK, Haskell WL, Marcus R, Ott SM, Torner JC, Quandt SA, Reiss TF, Ensrud KE. [https://pubmed.ncbi.nlm.nih.gov/8950879/ Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures.] Fracture Intervention Trial Research Group. Lancet. 1996 Dec 7;348(9041):1535-41. </ref> | ||
In the elderly patients | * Thoracolumbar junction (i.e., the segment from T12 to L2) location most often affected and the second most common site is the L2 to L5 region. <ref name=":2" /> | ||
* 30% of VCFs | * Estimated annual cost of VCFs in the US is $746 million. <ref>Lad SP, Patil CG, Lad EM, Boakye M. [https://pubmed.ncbi.nlm.nih.gov/17877264/ Trends in pathological vertebral fractures in the United States: 1993 to 2004.] J Neurosurg Spine. 2007 Sep;7(3):305-10.</ref> | ||
In the elderly patients, | |||
* 30% of VCFs in severe cases of osteoporosis occur while the patient is in bed <ref name=":2" /><ref>Kim HJ, Park S, Park SH, Park J, Chang BS, Lee CK, Yeom JS. [https://pubmed.ncbi.nlm.nih.gov/29436202/ Prevalence of Frailty in Patients with Osteoporotic Vertebral Compression Fracture and Its Association with Numbers of Fractures.] Yonsei Med J. 2018;59(2):317.</ref> | |||
* As the population continues to age, the population at risk of sustaining low energy fragility fractures will continue to increase as well. | * As the population continues to age, the population at risk of sustaining low energy fragility fractures will continue to increase as well. | ||
* Largely unreported and are probably more common radiographically (present up to 14% of women older than 60 years in one study)<ref name=":0">Radiopedia. | * Largely unreported and are probably more common radiographically (present up to 14% of women older than 60 years in one study)<ref name=":0">Radiopedia. Spinal compression fracture. Available from:https://radiopaedia.org/articles/osteoporotic-spinal-compression-fracture [accessed 26/10/2023]</ref> | ||
* Currently, 10 million Americans are already diagnosed with osteoporosis, and another 34 million have [[osteopenia]]. | * Currently, 10 million Americans are already diagnosed with osteoporosis, and another 34 million have [[osteopenia]]. | ||
== Clinical Presentation == | == Clinical Presentation == | ||
[[File:Low Back Pain Guy.jpg|thumb]] | |||
VFs present with pain and loss of mobility.<ref name=":0" /> | |||
Symptoms of | Symptoms of VFs can include: | ||
* Back pain is common in elderly patients. | * '''Back pain''' is common in elderly patients. Decreases when lying on the back (reduced weight baring conditions). <ref name="p3">Buchbinder R, Johnston RV, Rischin KJ, Homik J, Jones CA, Golmohammadi K, Kallmes DF. [https://pubmed.ncbi.nlm.nih.gov/29618171/ Percutaneous vertebroplasty for osteoporotic vertebral compression fracture.] Cochrane Database Syst Rev. 2018 Apr 4;4(4):CD006349. '''Level of Evidence: 1A.''' </ref><ref name="p8">NOF. Osteoporosis and your spine. National Osteoporosis Foundation. http://nof.org/articles/18 (accessed 03/02/15. </ref> | ||
* | * Most patients with vertebral fractures do not seek medical attention and up to 70% of vertebral fractures may not result in notably severe symptoms.<ref name="Griffith">Griffith JF. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4559972/ Identifying osteoporotic vertebral fracture.] Quant Imaging Med Surg. 2015 Aug;5(4):592-602. </ref> | ||
* '''Loss of height'''. Height loss of the osteoporotic fractured vertebra may be mild (20-25%), moderate (25-40%) or severe (> 40%). It commonly affects the thoracolumbar region, though any vertebra may be disturbed. | |||
* The pain of acute fracture usually lasts 4 to 6 weeks with intense pain at the site of fracture. | * The pain of acute fracture usually lasts 4 to 6 weeks with intense pain at the site of fracture. | ||
* The pain resolves over a period of six to 12 weeks. | * The pain resolves over a period of six to 12 weeks. | ||
* Chronic pain may also occur in patients with multiple compression fractures, height loss and low bone density (also due to structural changes or osteoarthritis). | * '''Chronic pain''' may also occur in patients with multiple compression fractures, height loss and low bone density (also due to structural changes or osteoarthritis).<ref name=":2" /> | ||
* Radiographic VCF may not be symptomatic. The greater the deformity, the greater the likelihood of pain and disability. | * Radiographic VCF may not be symptomatic. The greater the deformity, the greater the likelihood of pain and disability. | ||
* As height is lost, patients experience discomfort from the rib cage pressing downward on the pelvis. | * As height is lost, patients experience discomfort from the rib cage pressing downward on the pelvis. | ||
* Patients develop an exaggerated thoracic kyphosis and/or an exaggerated lumbar lordosis<ref name="Griffith" />which may result in decreased exercise tolerance and reduced abdominal space giving rise to early satiety and weight loss. | * Patients develop an exaggerated thoracic kyphosis and/or an exaggerated lumbar lordosis<ref name="Griffith" /> - due to multiple adjacent VCFs - <ref name=":2" />which may result in decreased exercise tolerance and reduced abdominal space giving rise to early satiety and '''weight loss'''. | ||
* Sleep disorders may occur and decreased self esteem +/- depression. | * '''Sleep disorders''' may occur and decreased self esteem +/- depression. | ||
* Self care may become difficult. <ref name="El-Fiki">El-Fiki M. Vertebroplasty, Kyphoplasty, Lordoplasty, | * Self care may become difficult. <ref name="El-Fiki">El-Fiki M. [https://pubmed.ncbi.nlm.nih.gov/27072339/ Vertebroplasty, Kyphoplasty, Lordoplasty, Expandable devices and Current treatment of painful osteoporoticvertebral fractures.]World Neurosurg. 2016 Jul;91:628-32.</ref><ref name="Longo">Longo UG, Loppini M, Denaro L, Maffulli N, Denaro V. [https://pubmed.ncbi.nlm.nih.gov/22323677/ Conservative management of patients with an osteoporotic vertebral fracture: a review of the literature.] J Bone Joint Surg Br. 2012 Feb;94(2):152-7. </ref><ref name="Silverman">Silverman SL. [https://pubmed.ncbi.nlm.nih.gov/1627411/ The Clinical Consequences of Vertebral Compression Fracture.] Bone 13, S27-S31. 1992. (Level of Evidence: 3B)</ref> | ||
* Associated with an increased morbidity and increased mortality<ref name="Griffith" /><ref name="p9">Puisto V, Rissanen H, Heliövaara M, Impivaara O, Jalanko T, Kröger H, Knekt P, Aromaa A, Helenius I. Vertebral fracture and cause-specific mortality: a prospective population study of 3,210 men and 3,730 women with 30 years of follow-up. Eur Spine J 2011 20: | * Associated with an increased morbidity and '''increased mortality''' <ref name="Griffith" /><ref name="p9">Puisto V, Rissanen H, Heliövaara M, Impivaara O, Jalanko T, Kröger H, Knekt P, Aromaa A, Helenius I. [https://pubmed.ncbi.nlm.nih.gov/21611851/ Vertebral fracture and cause-specific mortality: a prospective population study of 3,210 men and 3,730 women with 30 years of follow-up.] Eur Spine J 2011 20:2181–86. </ref> | ||
== Risk | == Fracture Risk Assessment Tool == | ||
A Fracture Risk Assessment Tool (FRAX) has been developed with the aim to predict osteoporotic fractures in general. It is based on cohort data generated from European, North American, Australian and Asian men and women. Although it does not refer to vertebral fractures exclusively, the FRAX algorithm indicates the 10-year chance of a major osteoporotic fracture taking place. <ref>Centre for Metabolic Bone Diseases, University of Sheffield. UK. Welcome to FRAX. Available from: https://frax.shef.ac.uk/FRAX/ [accessed 17-11-2023]</ref> Clinicians may use of the FRAX tool in combination with indications for assessment of osteoporotic vertebral fractures. | |||
== Indications for Vertebral Fracture Assessment == | |||
A Vertebral Fracture Assessment (VFA) is indicated: <ref>Gregson CL, Armstrong DJ, Bowden J, Cooper C, Edwards J, Gittoes NJL, Harvey N, Kanis J, Leyland S, Low R, McCloskey E, Moss K, Parker J, Paskins Z, Poole K, Reid DM, Stone M, Thomson J, Vine N, Compston J. [https://pubmed.ncbi.nlm.nih.gov/35378630/ UK clinical guideline for the prevention and treatment of osteoporosis]. Arch Osteoporos. 2022 Apr 5;17(1):58. </ref> | |||
* In postmenopausal women, and men aged ≥ 50 years, | |||
* In the presence of a history of ≥ 4 cm height loss, or [[kyphosis]], | |||
* If there is a history of recent or current long-term oral glucocorticoid therapy, or other therapy that compromises the bone | |||
* In BMD T-scores ≤ − 2.5 at either the spine or hip | |||
* If an acute onset of [[Low Back Pain|back pain]] with risk factors for [[osteoporosis]] at an older age is reported. An updated Cochrane review assessing the [[Test Diagnostics|diagnostic accuracy]] of red flags for vertebral fracture in patients complaining for low back pain <ref>Han CS, Hancock MJ, Downie A, Jarvik JG, Koes BW, Machado GC, Verhagen AP, Williams CM, Chen Q, Maher CG. [https://pubmed.ncbi.nlm.nih.gov/37615643/ Red flags to screen for vertebral fracture in people presenting with low back pain.] Cochrane Database Syst Rev. 2023 Aug 24;8(8):CD014461.</ref> concluded that appropriate sets of vertebral fracture indicators of various aetiologies are still lacking, so this finding may be interpreted with caution. | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
[[X-Rays| | [[File:Compressionfracture.jpg|thumb|435x435px|[[X-Rays|compression fracture of 3rd lumbar vertebra]]]]Diagnosed on [[X-Rays|Xrays]] when there is a loss of height in the anterior, middle, or posterior dimension of the vertebral body that exceeds 20%. | ||
Diagnosed on Xrays when there is a loss of height in the anterior, middle, or posterior dimension of the vertebral body that exceeds 20%. | |||
Osteoporotic spine fractures can be graded based on vertebral height loss as: | Osteoporotic spine fractures can be graded based on vertebral height loss as: | ||
* | * '''Mild''': up to 20-25% | ||
* | * '''Moderate''': 25-40% | ||
* | * '''Severe''': >40% | ||
Chronicity of the fracture indicates its temporal relationship with symptoms and hence is an important determination. | Chronicity of the fracture indicates its temporal relationship with symptoms and hence is an important determination when deciding on conservative or surgical treatment. <ref>Garnon J, Doré B, Auloge P, Caudrelier J, Dalili D, Ramamurthy N, Koch G, Cazzato RL, Gangi A. [https://link.springer.com/article/10.1007/s00270-019-02265-y Efficacy of the vertebral body stenting system for the restoration of vertebral height in acute traumatic compression fractures in a non-osteoporotic population.] Cardiovasc Intervent Radiol. 2019;42(11):1579–87. </ref> | ||
On conventional imaging, acute fracture signs include cortical breaking or impaction of trabeculae; in the absence of these signs fractures are chronic. | On conventional imaging, acute fracture signs include cortical breaking or impaction of trabeculae; in the absence of these signs fractures are chronic. | ||
In uncertain cases, [[MRI Scans|MRI]] signs of oedema (acute) and presence of radiotracer uptake on bone scintigraphy (acute) help decide the age of the fracture. | In uncertain cases, [[MRI Scans|MRI]] signs of oedema (acute) and presence of radiotracer uptake on bone scintigraphy (acute) help decide the age of the fracture. | ||
== Outcome Measures == | == Outcome Measures == | ||
| Line 82: | Line 86: | ||
# Quality of Life questionnaire: this can be measured with the use of the Quality of Life Questionnaire of the European Foundation for Osteoporosis (QUALEFFO). An other possibility is to use the Assessment of Quality of Life (AQoL) questionnaire or the European Quality of Life–5 Dimensions (EQ–5D) scale. | # Quality of Life questionnaire: this can be measured with the use of the Quality of Life Questionnaire of the European Foundation for Osteoporosis (QUALEFFO). An other possibility is to use the Assessment of Quality of Life (AQoL) questionnaire or the European Quality of Life–5 Dimensions (EQ–5D) scale. | ||
# Physical functioning: measured by a modified 23-item version of the [[Roland‐Morris Disability Questionnaire|Roland–Morris]] Disability Questionnaire. | # Physical functioning: measured by a modified 23-item version of the [[Roland‐Morris Disability Questionnaire|Roland–Morris]] Disability Questionnaire. | ||
# Pain at night and at rest (VAS score)<ref name="Diamond">Diamond TH. | # Pain at night and at rest (VAS score) <ref name="Diamond">Diamond TH, Champion B, Clark WA. [https://pubmed.ncbi.nlm.nih.gov/12681451/ Management of acute osteoporotic vertebral fractures: a nonrandomized trial comparing percutaneous vertebroplasty with conservative therapy.] Am J Med. 2003 Mar;114(4):257-65.</ref> | ||
#Research suggests that the four-factor Mini-BESTest model can be effective in evaluating multiple dynamic balance aspects in older adults with femoral or vertebral fractures and may help therapists in making clinical decisions, considering factors that indicated a decline in function. <ref>Miyata K, Hasegawa S, Iwamoto H, Otani T, Kaizu Y, Shinohara T, Usuda S. [https://pubmed.ncbi.nlm.nih.gov/32623475/ Comparison of the structural validity of three Balance Evaluation Systems Test in older adults with femoral or vertebral fracture]. J Rehabil Med. 2020 Jul 30;52(7):jrm00079.</ref> | |||
== Examination == | == Examination == | ||
Clinical assessment of vertebral fractures is generally poor and reliance is made on imaging studies for diagnosis<ref name="Longo" / | Clinical assessment of vertebral fractures is generally poor and reliance is made on imaging studies for diagnosis. <ref name="Longo" /> | ||
Two tests that help the practitioner to predict more accurately which patients have an acute vertebral fracture: <ref name="James Langdon">Langdon J, Way A, Heaton S, Bernard J, Molloy S. [https://pubmed.ncbi.nlm.nih.gov/19995486/ Vertebral compression fractures--new clinical signs to aid diagnosis.] Ann R Coll Surg Engl. 2010 Mar;92(2):163-6.</ref> | |||
# '''Closed-fist percussion sign:''' <ref name="James Langdon" />This test has a sensitivity of 87,5% and a specificity of 90%, which is good. Stand behind the patiënt and the patiënt stand in front of a mirror allowing you to see the reaction of the patiënt. Firm closed-fist percussion is used to examine the entire length of the spine. The clinical sign is positive when the patiënt complains of a sharp, sudden pain. | |||
# '''The supine sign:''' <ref name="James Langdon" /> This test has a sensitivity of 81,25% and a specificity of 93,33%, which is also pretty good. The patiënt is asked to lie supine with only one pillow for the head. The clinical sign is positive when the patiënt is unable to lie supine due to severe pain. | |||
== Medical Management == | == Medical Management == | ||
VFs are usually considered stable and do not require surgical instrumentation.<ref>Donnally C, Varacallo M. Fracture, Compression. 2018. Available from:https://www.researchgate.net/publication/329717392_Fracture_Compression [accessed 26/10/2023)</ref> | |||
Conservative management of acute osteoporotic compression fractures may involve the following goals: reducing pain and improving functional status. This can be accomplished with the following:<ref name=":4">Ponzano M, Tibert N, Brien S, Funnell L, Gibbs JC, Keller H, Laprade J, Morin SN, Papaioannou A, Weston Z, Wideman TH, Giangregorio LM. [https://pubmed.ncbi.nlm.nih.gov/36799981/ International consensus on the non-pharmacological and non-surgical management of osteoporotic vertebral fractures.] Osteoporos Int. 2023 Jun;34(6):1065-74. </ref> | |||
* Acetaminophen, ibuprofen, opioids | |||
* Nutritional support | |||
* Bed rest (but not continuous or prolonged) | |||
* Modifications in daily activities | |||
* Pacing or graded activity | |||
* Physiotherapy e.g. exercises after 12 weeks post fracture | |||
* Rehabilitation programmes | |||
* Taping and bracing for compression fractures is often done for patient comfort and is unlikely to influence spinal stability. A small study did support the use of semirigid thoracolumbar orthosis for gait improvement.<ref>Jacobs E, Senden R, McCrum C, van Rhijn LW, Meijer K, Willems PC. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6469477/ Effect of a semirigid thoracolumbar orthosis on gait and sagittal alignment in patients with an osteoporotic vertebral compression fracture]. Clin Interv Aging. 2019 Apr 11;14:671-680.</ref> | |||
* Treatment of the underlying disease (osteoporosis) is the recommended approach. | |||
In 2023, an international consensus was reached on the non-pharmacological and non-surgical management of osteoporotic vertebral fractures. <ref name=":4" /> Multidisciplinary biopsychosocial recommendations were made on pain, nutrition, safe movement, and exercise for individuals with acute and chronic vertebral fractures.<ref name=":4" /> | |||
Vertebroplasty is usually an outpatient procedure that takes one to two hours where under guided imaging, a needle get inserted into the vertebral body and cement is injected. This cement hardens quickly and | For persistent pain and the failure of conservative treatments, surgical intervention may be indicated.<ref>Gutierrez-Gonzalez R, Royuela A, Zamarron A. [https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-023-07041-1 Vertebral compression fractures: pain relief, progression and new fracture rate comparing vertebral augmentation with brace]. BMC Musculoskel Dis. 2023; 24: 898. </ref> | ||
* Vertebroplasty is usually an outpatient procedure that takes one to two hours where under guided imaging, a needle get inserted into the vertebral body and medical-grade cement is injected. This cement hardens quickly and stabilises the fracture. <ref>Buchbinder R, Johnston RV, Rischin KJ, Homik J, Jones C, Golmohammadi K, Kallmes DF. [https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD006349.pub4/full Vertebroplasty for treating spinal fractures due to osteoporosis.] Cochrane Library of Systematic Reviews 2018; 11:1465-1858.</ref> | |||
* Kyphoplasty is a very similar procedure, but in this case, a balloon is used to expand the vertebral body before injecting the cement. <ref>Whitney E, Alastra AJ. [https://www.ncbi.nlm.nih.gov/books/NBK547673/ Vertebral Fracture.] Available from:https://www.ncbi.nlm.nih.gov/books/NBK547673/ [accessed 26/10/2023]</ref> | |||
{{#ev:youtube|https://www.youtube.com/watch?v=QjvKkYehpUI|width}}<ref>Lee Health. Fixing a Fractured Spine. Available from: https://www.youtube.com/watch?v=QjvKkYehpUI&feature=emb_logo [accessed 26/10/2023]</ref> | |||
== Physical Therapy Management == | == Physical Therapy Management == | ||
[[File:Exercise_older_person.jpg|right|frameless|400x400px]] | |||
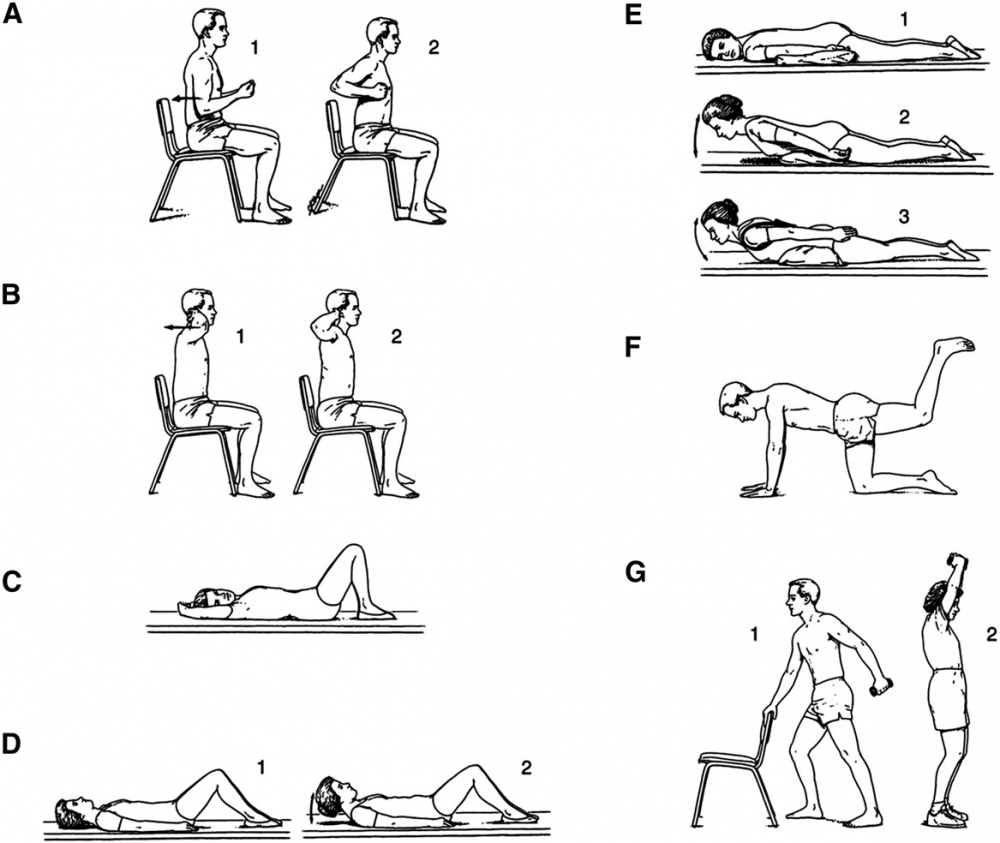
After a short period of bed rest, patients begin with a rehabilitation exercise programme. A "how-to" language is preferred rather than only suggesting activity restrictions. <ref name=":4" /> The goals of rehabilitation are the prevention of [[Falls in elderly|falls]], providing correct spine alignment (reduction of the [[Thoracic Hyperkyphosis]]), improving respiratory function in severe cases, and enhancing axial muscle strength. <ref name=":1" /> | |||
After a short period of bed rest patients | |||
Treatment approaches include: | |||
* Diaphragmatic breathing exercises <ref name=":4" />and pelvic floor exercises | |||
* Strengthening exercises, stabilisation exercise, [[Balance Boards|balance training]], stretching, relaxation techniques, taping.<ref name="Pratelli et al (2010)">Pratelli E, Cinotti I, Pasquetti P. [https://pubmed.ncbi.nlm.nih.gov/22461291/ Rehabilitation in osteoporotic vertebral fractures.] Clin Cases Miner Bone Metab. 2010 7(1): 45–47.</ref><ref name="Barker et al (2014)">Barker KL, Newman M, Stallard N, Leal J, Lowe CM, Javaid MK, Noufaily A, Hughes T, Smith D, Gandhi V, Cooper C, Lamb SE; PROVE trial group. [https://pubmed.ncbi.nlm.nih.gov/31720722/ Physiotherapy rehabilitation for osteoporotic vertebral fracture-a randomised controlled trial and economic evaluation (PROVE trial).] Osteoporos Int. 2020 Feb;31(2):277-89. </ref> | |||
* Exercises such as walking help to maintain or improve bone density in an osteoporotic population. | |||
Strengthening and | * Strengthening exercises, using weights or resistance bands help maintain or improve bone density at the location of the targeted muscle attachments. <ref>Hong AR, Kim SW. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6279907/ Effects of resistance exercise on bone health.] Endocrinol Metab. 2018 Dec 1;33(4):435-44.</ref> Maintaining bone health is extremely important, especially in the elderly as there typically is a decline in bone mass with age. | ||
* Strengthening and flexibility exercises improve overall physical function and postural control (important to reduce risk for falls).<ref name="burke">Burke TN, Franca FJR, Ferreira de Meneses SR, Pereira RMR, Marques AP. [https://pubmed.ncbi.nlm.nih.gov/22498664/ Postural control in elderly women with osteoporosis: comparison of balance, strengthening and stretching exercises. A randomized controlled trial.] Clinical Rehabilitation 2012; 26 (11): 1021-1031. </ref> | |||
* Combined balance and progressive strength training programme produced the best results in terms of maintaining leg strength, balance, bone mineral density and physical function compared to balance or strength training alone. <ref name="de kam">De Kam D, Smulders E, Weerdesteyn V, Smits-Engelsman BCM. [https://pubmed.ncbi.nlm.nih.gov/19421702/ Exercise interventions to reduce fall-related fractures and their risk factors in individuals with low bone density: a systematic review of randomized controlled trials.] Osteoporos Int. 2009;20:2111–25.</ref><ref name="karinkanta">Karinkanta S, Heinonen A, Sievänen H, Uusi-Rasi K, Pasanen M, Ojala K. [https://pubmed.ncbi.nlm.nih.gov/17103296/ A multi-component exercise regimen to prevent functional decline and bone fragility in home-dwelling elderly women: a randomized, controlled trial.] Osteoporos Int. 2007;18:453–462. </ref><ref name="hourigan">Hourigan SR, Nitz JC, Brauer SG, O'Neill S, Wong J, Richardson CA. [https://pubmed.ncbi.nlm.nih.gov/18188658/ Positive effects of exercise on falls and fracture risk in osteopenic women.] Osteoporos Int. 2008;19:1077–86.</ref> | |||
* Spinal extensor strengthening programme and a dynamic proprioceptive programme increase bone density and reduced the risk of VCFs.<ref name="sinaki 1">Sinaki M, Lynn SG. [https://pubmed.ncbi.nlm.nih.gov/11953540/ Reducing the risk of falls through proprioceptive dynamic posture training in osteoporotic women with kyphotic posturing: a randomized pilot study].Am J Phys Med Rehabil. 2002 Apr;81(4):241-6. </ref> | |||
* Back extensor exercises improve muscle strength, providing a better dynamic-static posture and reduction of the kyphotic deformity. Correction of the kyphosis also results in pain relief, increased mobility and an improvement in the quality of life.<ref name="itoi">Itoi E, Sinaki M.[https://pubmed.ncbi.nlm.nih.gov/7967758/ Effect of back-strengthening exercise on posture in healthy women 49 to 65 years of age].Mayo Clin Proc. 1994 Nov;69(11):1054-9. (Level of Evidence: 3B)</ref> | |||
Back extensor exercises improve muscle strength, providing a better dynamic-static posture and reduction of the kyphotic deformity. Correction of the kyphosis also results in pain relief, increased mobility and an improvement in the quality of life<ref name="itoi">Itoi E, Sinaki M.Effect of back-strengthening exercise on posture in healthy women 49 to 65 years of age.Mayo Clin Proc. 1994 Nov;69(11):1054-9. (Level of Evidence: 3B)</ref> | |||
[[Image:Oefeningen osteo.png|1000x1000px]] | [[Image:Oefeningen osteo.png|1000x1000px]] | ||
<br> | <br>Postural [[taping]] can help in postural alignment. Tape is applied to the skin to provide increased proprioceptive feedback about postural alignment, improve thoracic extension, reduce pain and facilitate postural muscle activity and balance. <ref name="bautmans">Bautmans I, Van Arken J, Van Mackelenberg M, Mets T. [https://pubmed.ncbi.nlm.nih.gov/20140408/ Rehabilitation using manual mobilization for thoraic kyphosis in elderly postmenopauzal patients with osteoporosis.] J Rehabil Med 2010, 42: 129-135. (Level of Evidence: 3B)</ref> For example;{{#ev:youtube|996cC3ovLEQ|300}}<ref>John Gibbons. Try this Kinesiology Taping technique for poor posture - its incredible. Available from: http://www.youtube.com/watch?v=996cC3ovLEQ[last accessed 21/4/2020]</ref> | ||
{{#ev:youtube|996cC3ovLEQ|300}}<ref>John Gibbons. Try this Kinesiology Taping technique for poor posture - its incredible. Available from: http://www.youtube.com/watch?v=996cC3ovLEQ[last accessed 21/4/2020]</ref> | |||
== Clinical Bottom Line == | == Clinical Bottom Line == | ||
* Osteoporotic vertebral fractures are fractures of one or more of the vertebrae due to osteoporosis.[[File:Strengthing exercise for old people .jpg|right|frameless|400x400px]]Osteoporosis causes the bones to be more fragile and more likely to fracture. Osteoporotic vertebral fractures classically occur during normal day-to-day activities such as bending, twisting, walking or lifting relatively light objects. | |||
Osteoporotic vertebral fractures are fractures of one or more of the vertebrae due to osteoporosis. Osteoporosis causes the bones to be more fragile and more likely to fracture. Osteoporotic vertebral fractures classically occur during normal day-to-day activities such as bending, twisting, walking or lifting relatively light objects. | * The pain of acute fracture usually lasts 4 to 6 weeks with intense pain at the site of fracture. Chronic pain may also occur in patients with multiple compression fractures, height loss and low bone density. Although this is probably due to structural changes or osteoarthritis. | ||
* Vertebral fractures don't only occur due to osteoporosis. Also a trauma or metastasis can cause a vertebral fracture. The diagnosis of osteoporosis can be confirmed by Dual Energy X-ray Absorptiometry (DXA). | |||
The pain of acute fracture usually lasts 4 to 6 weeks with intense pain at the site of fracture. Chronic pain may also occur in patients with multiple compression fractures, height loss and low bone density. Although this is probably due to structural changes or osteoarthritis. | * Often used outcome measures to evaluate the progression of a patient are: Visual analogue scale for overall pain and pain during day and night (VAS), a Quality of Life questionnaire and a Physical functioning questionaire ( modified 23-item version of the Roland–Morris Disability Questionnaire). | ||
* Conservative treatment (bed rest, analgesic medication, physiotherapy and bracing) still is the method of choice as medical treatment. Vertebral fractures can also be treated surgically using vertebroplasty and kyphoplasty. | |||
Vertebral fractures don't only occur due to osteoporosis. Also a trauma or metastasis can cause a vertebral fracture. The diagnosis of osteoporosis can be confirmed by Dual Energy X-ray Absorptiometry (DXA). | * As physical therapy management there are a number of treatment approaches, including strengthening exercise, stabilisation exercise, balance training, stretching, relaxation techniques, manual therapy and taping. | ||
Often used outcome measures to evaluate the progression of a patient are: Visual analogue scale for overall pain and pain during day and night (VAS), a Quality of Life questionnaire and a Physical functioning questionaire ( modified 23-item version of the Roland–Morris Disability Questionnaire). | |||
Conservative treatment (bed rest, analgesic medication, physiotherapy and bracing) still is the method of choice as medical treatment. Vertebral fractures can also be treated surgically using vertebroplasty and kyphoplasty. | |||
As physical therapy management there are a number of treatment approaches, including strengthening exercise, stabilisation exercise, balance training, stretching, relaxation techniques, manual therapy and taping. | |||
== Key Research == | == Key Research == | ||
The following articles are key evidence pieces for physical therapy interventions: | The following articles are key evidence pieces for physical therapy interventions: | ||
* Exercise interventions to reduce fall-related fractures and their risk factors in individuals with low bone density: a systematic review of randomized controlled trials<ref name="p4">Liu JT et al. Balloon kyphoplasty versus vertebroplasty for treatment of osteoporotic vertebral compression fracture: a prospective, comparative, and randomized clinical study. Osteoporos Int. 2010 Feb;21(2):359-64. '''Level of Evidence: 1B.''' </ref> | * International consensus on the non-pharmacological and non-surgical management of osteoporotic vertebral fractures. <ref name=":4" /> | ||
* Exercise interventions to reduce fall-related fractures and their risk factors in individuals with low bone density: a systematic review of randomized controlled trials <ref name="p4">Liu JT et al. Balloon kyphoplasty versus vertebroplasty for treatment of osteoporotic vertebral compression fracture: a prospective, comparative, and randomized clinical study. Osteoporos Int. 2010 Feb;21(2):359-64. '''Level of Evidence: 1B.''' </ref> | |||
* A multi-component exercise regimen to prevent functional decline and bone fragility in home-dwelling elderly women: a randomized, controlled trial <ref name="p5">Gauthier A, Kanis JA, Jiang Y, Martin M, Compston JE, Borgström F, Cooper C, McCloskey EV. Epidemiological burden of postmenopausal osteoporosis in the UK from 2010 to 2021: estimations from a disease model. Arch Osteoporos 2011 6:179–188. </ref> | * A multi-component exercise regimen to prevent functional decline and bone fragility in home-dwelling elderly women: a randomized, controlled trial <ref name="p5">Gauthier A, Kanis JA, Jiang Y, Martin M, Compston JE, Borgström F, Cooper C, McCloskey EV. Epidemiological burden of postmenopausal osteoporosis in the UK from 2010 to 2021: estimations from a disease model. Arch Osteoporos 2011 6:179–188. </ref> | ||
* Positive effects of exercise on falls and fracture risk in osteopenic women<ref name="p6">Kim DH, Vaccaro AR. Contemporary Concepts in Spine Care: Osteoporotic compression fractures of the spine; current options and considerations for treatment. The Spine Journal. 2006 6 479–487. </ref> | * Positive effects of exercise on falls and fracture risk in osteopenic women <ref name="p6">Kim DH, Vaccaro AR. Contemporary Concepts in Spine Care: Osteoporotic compression fractures of the spine; current options and considerations for treatment. The Spine Journal. 2006 6 479–487. </ref> | ||
* Reducing the risk of falls through proprioceptive dynamic posture training in osteoporotic women with kyphotic posturing: a randomized pilot study | * Reducing the risk of falls through proprioceptive dynamic posture training in osteoporotic women with kyphotic posturing: a randomized pilot study | ||
* Identifying osteoporotic vertebral fracture<ref name="p7">NICE. Alendronate, etidronate, risedronate, raloxifene and strontium ranelate for the primary prevention of osteoporotic fragility fractures in postmenopausal women (amended): NICE technology appraisal guidance 160. Manchester: National Institute for Health and Care Excellence, 2011. </ref> | * Identifying osteoporotic vertebral fracture <ref name="p7">NICE. Alendronate, etidronate, risedronate, raloxifene and strontium ranelate for the primary prevention of osteoporotic fragility fractures in postmenopausal women (amended): NICE technology appraisal guidance 160. Manchester: National Institute for Health and Care Excellence, 2011. </ref> | ||
* Position Statement of the Korean Society for Bone and Mineral Research<ref name="p7" /> | * Position Statement of the Korean Society for Bone and Mineral Research <ref name="p7" /> | ||
== Resources == | == Resources == | ||
Latest revision as of 19:40, 11 February 2024
Top Contributors - Mathieu Vanderroost, Angeliki Chorti, Lucinda hampton, Jasper Vermeersch, Jon Room, Kim Jackson, Jelle Van Hemelryck, Khloud Shreif, Laura Ritchie, Vidya Acharya, Lauren Lopez, Kai A. Sigel, WikiSysop, Claire Knott, 127.0.0.1, Admin and Rachael Lowe
Definition / Description[edit | edit source]
Osteoporotic (fragility) vertebral fractures (VFs) are fractures that result from mechanical forces that would not ordinarily result in a fracture. [1] These types of fractures are insufficiency fractures, caused by normal stresses on abnormal bone, often indicating frailty.
Classification of Vertebral Fractures[edit | edit source]
Classification of VFs has been described by type of deformity (wedge, biconcavity, or crush compression) and further by the degree of deformity (grades I, II). [2] [3]
- Wedge VFs are the most common, occuring in the midthoracic region with compression of the anterior segment of the vertebral body (VB) and the anterior longitudinal ligament (ALL), and reports of more than 50% of all VFs. [4] Wedge fractures do not involve the posterior half of the VB and do not involve the posterior osseous ligamentous complex. The former distinguishes a compression fracture from a burst fracture.
- Biconcave compression VFs are the second-most common (approximately 17% of all VFs); here, only the middle portion of the vertebral body is collapsed, with no compromise of the anterior and posterior walls. [3]
- Crush compression VFs are the least common (13%), and are characterised by the collaplse of the entire anterior column, including anterior and posterior margins. [3]
- The remaining 20% of VFs may involve complex fractures of the spine. [3]
- Grade I refers to 3 SD < deformity < 4 SD and grade 2 deformity > 4 SD from the normal range for each vertebra. [2]
Etiology[edit | edit source]
- The most common etiology of VFs is osteoporosis, making these fractures the most common fragility fracture. [5][6]
- In contrast, vertebral compression fractures (VCFs) demonstrate a bimodal distribution with younger patients sustaining these injuries secondary to high energy mechanisms (fall from a height, MVA, etc.).
- VFs occur secondary to an axial/compressive (and to a lesser extent, flexion) load with a resultant biomechanical failure of the bone resulting in a fracture.
Watch this video analysing causes of VFs (including osteoporotic):
Epidemiology[edit | edit source]
European population studies have shown that the annual incidence of VCFs is 10.7 per 1000 women and 5.7 per 1000 men. [8]
- VCFs are the most common fragility fractures reported in the literature. [9]
- VCFs are common in Asian and Caucasian women, and less common in African-American women. [3]
- Approximately 1.5 million VCFs occur annually in the United States (US) alone in the general population. [10]
- Prevalence increases with age, and it is estimated that 40% to 50% of patients over age 80 years have sustained a VCF either acutely, or recognised incidentally during clinical workup for a separate condition.[11]
- Thoracolumbar junction (i.e., the segment from T12 to L2) location most often affected and the second most common site is the L2 to L5 region. [3]
- Estimated annual cost of VCFs in the US is $746 million. [12]
In the elderly patients,
- 30% of VCFs in severe cases of osteoporosis occur while the patient is in bed [3][13]
- As the population continues to age, the population at risk of sustaining low energy fragility fractures will continue to increase as well.
- Largely unreported and are probably more common radiographically (present up to 14% of women older than 60 years in one study)[14]
- Currently, 10 million Americans are already diagnosed with osteoporosis, and another 34 million have osteopenia.
Clinical Presentation[edit | edit source]
VFs present with pain and loss of mobility.[14]
Symptoms of VFs can include:
- Back pain is common in elderly patients. Decreases when lying on the back (reduced weight baring conditions). [15][16]
- Most patients with vertebral fractures do not seek medical attention and up to 70% of vertebral fractures may not result in notably severe symptoms.[6]
- Loss of height. Height loss of the osteoporotic fractured vertebra may be mild (20-25%), moderate (25-40%) or severe (> 40%). It commonly affects the thoracolumbar region, though any vertebra may be disturbed.
- The pain of acute fracture usually lasts 4 to 6 weeks with intense pain at the site of fracture.
- The pain resolves over a period of six to 12 weeks.
- Chronic pain may also occur in patients with multiple compression fractures, height loss and low bone density (also due to structural changes or osteoarthritis).[3]
- Radiographic VCF may not be symptomatic. The greater the deformity, the greater the likelihood of pain and disability.
- As height is lost, patients experience discomfort from the rib cage pressing downward on the pelvis.
- Patients develop an exaggerated thoracic kyphosis and/or an exaggerated lumbar lordosis[6] - due to multiple adjacent VCFs - [3]which may result in decreased exercise tolerance and reduced abdominal space giving rise to early satiety and weight loss.
- Sleep disorders may occur and decreased self esteem +/- depression.
- Self care may become difficult. [17][18][19]
- Associated with an increased morbidity and increased mortality [6][20]
Fracture Risk Assessment Tool[edit | edit source]
A Fracture Risk Assessment Tool (FRAX) has been developed with the aim to predict osteoporotic fractures in general. It is based on cohort data generated from European, North American, Australian and Asian men and women. Although it does not refer to vertebral fractures exclusively, the FRAX algorithm indicates the 10-year chance of a major osteoporotic fracture taking place. [21] Clinicians may use of the FRAX tool in combination with indications for assessment of osteoporotic vertebral fractures.
Indications for Vertebral Fracture Assessment[edit | edit source]
A Vertebral Fracture Assessment (VFA) is indicated: [22]
- In postmenopausal women, and men aged ≥ 50 years,
- In the presence of a history of ≥ 4 cm height loss, or kyphosis,
- If there is a history of recent or current long-term oral glucocorticoid therapy, or other therapy that compromises the bone
- In BMD T-scores ≤ − 2.5 at either the spine or hip
- If an acute onset of back pain with risk factors for osteoporosis at an older age is reported. An updated Cochrane review assessing the diagnostic accuracy of red flags for vertebral fracture in patients complaining for low back pain [23] concluded that appropriate sets of vertebral fracture indicators of various aetiologies are still lacking, so this finding may be interpreted with caution.
Diagnostic Procedures[edit | edit source]
Diagnosed on Xrays when there is a loss of height in the anterior, middle, or posterior dimension of the vertebral body that exceeds 20%.
Osteoporotic spine fractures can be graded based on vertebral height loss as:
- Mild: up to 20-25%
- Moderate: 25-40%
- Severe: >40%
Chronicity of the fracture indicates its temporal relationship with symptoms and hence is an important determination when deciding on conservative or surgical treatment. [24]
On conventional imaging, acute fracture signs include cortical breaking or impaction of trabeculae; in the absence of these signs fractures are chronic.
In uncertain cases, MRI signs of oedema (acute) and presence of radiotracer uptake on bone scintigraphy (acute) help decide the age of the fracture.
Outcome Measures[edit | edit source]
- Visual analogue scale for overall pain (VAS).
- Quality of Life questionnaire: this can be measured with the use of the Quality of Life Questionnaire of the European Foundation for Osteoporosis (QUALEFFO). An other possibility is to use the Assessment of Quality of Life (AQoL) questionnaire or the European Quality of Life–5 Dimensions (EQ–5D) scale.
- Physical functioning: measured by a modified 23-item version of the Roland–Morris Disability Questionnaire.
- Pain at night and at rest (VAS score) [25]
- Research suggests that the four-factor Mini-BESTest model can be effective in evaluating multiple dynamic balance aspects in older adults with femoral or vertebral fractures and may help therapists in making clinical decisions, considering factors that indicated a decline in function. [26]
Examination[edit | edit source]
Clinical assessment of vertebral fractures is generally poor and reliance is made on imaging studies for diagnosis. [18]
Two tests that help the practitioner to predict more accurately which patients have an acute vertebral fracture: [27]
- Closed-fist percussion sign: [27]This test has a sensitivity of 87,5% and a specificity of 90%, which is good. Stand behind the patiënt and the patiënt stand in front of a mirror allowing you to see the reaction of the patiënt. Firm closed-fist percussion is used to examine the entire length of the spine. The clinical sign is positive when the patiënt complains of a sharp, sudden pain.
- The supine sign: [27] This test has a sensitivity of 81,25% and a specificity of 93,33%, which is also pretty good. The patiënt is asked to lie supine with only one pillow for the head. The clinical sign is positive when the patiënt is unable to lie supine due to severe pain.
Medical Management[edit | edit source]
VFs are usually considered stable and do not require surgical instrumentation.[28]
Conservative management of acute osteoporotic compression fractures may involve the following goals: reducing pain and improving functional status. This can be accomplished with the following:[29]
- Acetaminophen, ibuprofen, opioids
- Nutritional support
- Bed rest (but not continuous or prolonged)
- Modifications in daily activities
- Pacing or graded activity
- Physiotherapy e.g. exercises after 12 weeks post fracture
- Rehabilitation programmes
- Taping and bracing for compression fractures is often done for patient comfort and is unlikely to influence spinal stability. A small study did support the use of semirigid thoracolumbar orthosis for gait improvement.[30]
- Treatment of the underlying disease (osteoporosis) is the recommended approach.
In 2023, an international consensus was reached on the non-pharmacological and non-surgical management of osteoporotic vertebral fractures. [29] Multidisciplinary biopsychosocial recommendations were made on pain, nutrition, safe movement, and exercise for individuals with acute and chronic vertebral fractures.[29]
For persistent pain and the failure of conservative treatments, surgical intervention may be indicated.[31]
- Vertebroplasty is usually an outpatient procedure that takes one to two hours where under guided imaging, a needle get inserted into the vertebral body and medical-grade cement is injected. This cement hardens quickly and stabilises the fracture. [32]
- Kyphoplasty is a very similar procedure, but in this case, a balloon is used to expand the vertebral body before injecting the cement. [33]
Physical Therapy Management[edit | edit source]
After a short period of bed rest, patients begin with a rehabilitation exercise programme. A "how-to" language is preferred rather than only suggesting activity restrictions. [29] The goals of rehabilitation are the prevention of falls, providing correct spine alignment (reduction of the Thoracic Hyperkyphosis), improving respiratory function in severe cases, and enhancing axial muscle strength. [1]
Treatment approaches include:
- Diaphragmatic breathing exercises [29]and pelvic floor exercises
- Strengthening exercises, stabilisation exercise, balance training, stretching, relaxation techniques, taping.[35][36]
- Exercises such as walking help to maintain or improve bone density in an osteoporotic population.
- Strengthening exercises, using weights or resistance bands help maintain or improve bone density at the location of the targeted muscle attachments. [37] Maintaining bone health is extremely important, especially in the elderly as there typically is a decline in bone mass with age.
- Strengthening and flexibility exercises improve overall physical function and postural control (important to reduce risk for falls).[38]
- Combined balance and progressive strength training programme produced the best results in terms of maintaining leg strength, balance, bone mineral density and physical function compared to balance or strength training alone. [39][40][41]
- Spinal extensor strengthening programme and a dynamic proprioceptive programme increase bone density and reduced the risk of VCFs.[42]
- Back extensor exercises improve muscle strength, providing a better dynamic-static posture and reduction of the kyphotic deformity. Correction of the kyphosis also results in pain relief, increased mobility and an improvement in the quality of life.[43]
Postural taping can help in postural alignment. Tape is applied to the skin to provide increased proprioceptive feedback about postural alignment, improve thoracic extension, reduce pain and facilitate postural muscle activity and balance. [44] For example;
Clinical Bottom Line[edit | edit source]
- Osteoporotic vertebral fractures are fractures of one or more of the vertebrae due to osteoporosis.Osteoporosis causes the bones to be more fragile and more likely to fracture. Osteoporotic vertebral fractures classically occur during normal day-to-day activities such as bending, twisting, walking or lifting relatively light objects.
- The pain of acute fracture usually lasts 4 to 6 weeks with intense pain at the site of fracture. Chronic pain may also occur in patients with multiple compression fractures, height loss and low bone density. Although this is probably due to structural changes or osteoarthritis.
- Vertebral fractures don't only occur due to osteoporosis. Also a trauma or metastasis can cause a vertebral fracture. The diagnosis of osteoporosis can be confirmed by Dual Energy X-ray Absorptiometry (DXA).
- Often used outcome measures to evaluate the progression of a patient are: Visual analogue scale for overall pain and pain during day and night (VAS), a Quality of Life questionnaire and a Physical functioning questionaire ( modified 23-item version of the Roland–Morris Disability Questionnaire).
- Conservative treatment (bed rest, analgesic medication, physiotherapy and bracing) still is the method of choice as medical treatment. Vertebral fractures can also be treated surgically using vertebroplasty and kyphoplasty.
- As physical therapy management there are a number of treatment approaches, including strengthening exercise, stabilisation exercise, balance training, stretching, relaxation techniques, manual therapy and taping.
Key Research[edit | edit source]
The following articles are key evidence pieces for physical therapy interventions:
- International consensus on the non-pharmacological and non-surgical management of osteoporotic vertebral fractures. [29]
- Exercise interventions to reduce fall-related fractures and their risk factors in individuals with low bone density: a systematic review of randomized controlled trials [46]
- A multi-component exercise regimen to prevent functional decline and bone fragility in home-dwelling elderly women: a randomized, controlled trial [47]
- Positive effects of exercise on falls and fracture risk in osteopenic women [48]
- Reducing the risk of falls through proprioceptive dynamic posture training in osteoporotic women with kyphotic posturing: a randomized pilot study
- Identifying osteoporotic vertebral fracture [49]
- Position Statement of the Korean Society for Bone and Mineral Research [49]
Resources[edit | edit source]
www.nhs.uk/conditions/Osteoporosis/Pages/Introduction.aspx
www.nos.org.uk/about-osteoporosis
References[edit | edit source]
- ↑ 1.0 1.1 Yoo JH, Moon SH, Ha YC, Lee DY, Gong HS, Park SY, Yang KH. Osteoporotic Fracture: 2015 Position Statement of the Korean Society for Bone and Mineral Research.J Bone Metab. 2015 Nov;22(4):175-81. 30. Level of Evidence: 2B.
- ↑ 2.0 2.1 Eastell R, Cedel SL, Wahner HW, Riggs BL, Melton LJ III. Classification of vertebral fractures. JBMR 1991; 6(3):207-15.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 Alexandru D, So W. Evaluation and Management of Vertebral Compression Fractures. Perm J. 2012 Fall; 16(4): 46–51.
- ↑ Black DM, Arden NK, Palermo L, Pearson J, Cummings SR. Prevalent vertebral deformities predict hip fractures and new vertebral deformities but not wrist fractures. Study of Osteoporotic Fractures Research Group. J Bone Miner Res. 1999 May;14(5):821–8.
- ↑ Ettinger B, Black DM, Nevitt MC, Rundle AC, Cauley JA, Cummings SR, Genant HK. Contribution of vertebral deformities to chronic back pain and disability. The Study of Osteoporotic Fractures Research Group. J Bone Miner Res. 1992 Apr;7(4):449-56.
- ↑ 6.0 6.1 6.2 6.3 Griffith JF. Identifying osteoporotic vertebral fracture. Quant Imaging Med Surg. 2015 Aug;5(4):592-602.
- ↑ Spine live. Spinal compression fractures reasons. Available from: https://www.youtube.com/watch?v=LILgFAEMAbg [accessed 26/10/2023]
- ↑ European Prospective Osteoporosis Study (EPOS) Group; Felsenberg D, Silman AJ, Lunt M, Armbrecht G, Ismail AA, Finn JD, Cockerill WC, Banzer D, Benevolenskaya LI, Bhalla A, Bruges Armas J, Cannata JB, Cooper C, Dequeker J, Eastell R, Felsch B, Gowin W, Havelka S, Hoszowski K, Jajic I, Janott J, Johnell O, Kanis JA, Kragl G, Lopes Vaz A, Lorenc R, Lyritis G, Masaryk P, Matthis C, Miazgowski T, Parisi G, Pols HA, Poor G, Raspe HH, Reid DM, Reisinger W, Schedit-Nave C, Stepan JJ, Todd CJ, Weber K, Woolf AD, Yershova OB, Reeve J, O'Neill TW. Incidence of vertebral fracture in europe: results from the European Prospective Osteoporosis Study (EPOS). J Bone Miner Res. 2002 Apr;17(4):716-24.
- ↑ Kutsal FY, Ergin Ergani GO. Vertebral compression fractures: Still an unpredictable aspect of osteoporosis. Turk J Med Sci. 2021; 51(2): 393–399.
- ↑ Barr JD, Barr MS, Lemley TJ, McCann RM. Percutaneous vertebroplasty for pain relief and spinal stabilization. Spine (Phila Pa 1976). 2000 Apr 15;25(8):923-8.
- ↑ Black DM, Cummings SR, Karpf DB, Cauley JA, Thompson DE, Nevitt MC, Bauer DC, Genant HK, Haskell WL, Marcus R, Ott SM, Torner JC, Quandt SA, Reiss TF, Ensrud KE. Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet. 1996 Dec 7;348(9041):1535-41.
- ↑ Lad SP, Patil CG, Lad EM, Boakye M. Trends in pathological vertebral fractures in the United States: 1993 to 2004. J Neurosurg Spine. 2007 Sep;7(3):305-10.
- ↑ Kim HJ, Park S, Park SH, Park J, Chang BS, Lee CK, Yeom JS. Prevalence of Frailty in Patients with Osteoporotic Vertebral Compression Fracture and Its Association with Numbers of Fractures. Yonsei Med J. 2018;59(2):317.
- ↑ 14.0 14.1 Radiopedia. Spinal compression fracture. Available from:https://radiopaedia.org/articles/osteoporotic-spinal-compression-fracture [accessed 26/10/2023]
- ↑ Buchbinder R, Johnston RV, Rischin KJ, Homik J, Jones CA, Golmohammadi K, Kallmes DF. Percutaneous vertebroplasty for osteoporotic vertebral compression fracture. Cochrane Database Syst Rev. 2018 Apr 4;4(4):CD006349. Level of Evidence: 1A.
- ↑ NOF. Osteoporosis and your spine. National Osteoporosis Foundation. http://nof.org/articles/18 (accessed 03/02/15.
- ↑ El-Fiki M. Vertebroplasty, Kyphoplasty, Lordoplasty, Expandable devices and Current treatment of painful osteoporoticvertebral fractures.World Neurosurg. 2016 Jul;91:628-32.
- ↑ 18.0 18.1 Longo UG, Loppini M, Denaro L, Maffulli N, Denaro V. Conservative management of patients with an osteoporotic vertebral fracture: a review of the literature. J Bone Joint Surg Br. 2012 Feb;94(2):152-7.
- ↑ Silverman SL. The Clinical Consequences of Vertebral Compression Fracture. Bone 13, S27-S31. 1992. (Level of Evidence: 3B)
- ↑ Puisto V, Rissanen H, Heliövaara M, Impivaara O, Jalanko T, Kröger H, Knekt P, Aromaa A, Helenius I. Vertebral fracture and cause-specific mortality: a prospective population study of 3,210 men and 3,730 women with 30 years of follow-up. Eur Spine J 2011 20:2181–86.
- ↑ Centre for Metabolic Bone Diseases, University of Sheffield. UK. Welcome to FRAX. Available from: https://frax.shef.ac.uk/FRAX/ [accessed 17-11-2023]
- ↑ Gregson CL, Armstrong DJ, Bowden J, Cooper C, Edwards J, Gittoes NJL, Harvey N, Kanis J, Leyland S, Low R, McCloskey E, Moss K, Parker J, Paskins Z, Poole K, Reid DM, Stone M, Thomson J, Vine N, Compston J. UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos. 2022 Apr 5;17(1):58.
- ↑ Han CS, Hancock MJ, Downie A, Jarvik JG, Koes BW, Machado GC, Verhagen AP, Williams CM, Chen Q, Maher CG. Red flags to screen for vertebral fracture in people presenting with low back pain. Cochrane Database Syst Rev. 2023 Aug 24;8(8):CD014461.
- ↑ Garnon J, Doré B, Auloge P, Caudrelier J, Dalili D, Ramamurthy N, Koch G, Cazzato RL, Gangi A. Efficacy of the vertebral body stenting system for the restoration of vertebral height in acute traumatic compression fractures in a non-osteoporotic population. Cardiovasc Intervent Radiol. 2019;42(11):1579–87.
- ↑ Diamond TH, Champion B, Clark WA. Management of acute osteoporotic vertebral fractures: a nonrandomized trial comparing percutaneous vertebroplasty with conservative therapy. Am J Med. 2003 Mar;114(4):257-65.
- ↑ Miyata K, Hasegawa S, Iwamoto H, Otani T, Kaizu Y, Shinohara T, Usuda S. Comparison of the structural validity of three Balance Evaluation Systems Test in older adults with femoral or vertebral fracture. J Rehabil Med. 2020 Jul 30;52(7):jrm00079.
- ↑ 27.0 27.1 27.2 Langdon J, Way A, Heaton S, Bernard J, Molloy S. Vertebral compression fractures--new clinical signs to aid diagnosis. Ann R Coll Surg Engl. 2010 Mar;92(2):163-6.
- ↑ Donnally C, Varacallo M. Fracture, Compression. 2018. Available from:https://www.researchgate.net/publication/329717392_Fracture_Compression [accessed 26/10/2023)
- ↑ 29.0 29.1 29.2 29.3 29.4 29.5 Ponzano M, Tibert N, Brien S, Funnell L, Gibbs JC, Keller H, Laprade J, Morin SN, Papaioannou A, Weston Z, Wideman TH, Giangregorio LM. International consensus on the non-pharmacological and non-surgical management of osteoporotic vertebral fractures. Osteoporos Int. 2023 Jun;34(6):1065-74.
- ↑ Jacobs E, Senden R, McCrum C, van Rhijn LW, Meijer K, Willems PC. Effect of a semirigid thoracolumbar orthosis on gait and sagittal alignment in patients with an osteoporotic vertebral compression fracture. Clin Interv Aging. 2019 Apr 11;14:671-680.
- ↑ Gutierrez-Gonzalez R, Royuela A, Zamarron A. Vertebral compression fractures: pain relief, progression and new fracture rate comparing vertebral augmentation with brace. BMC Musculoskel Dis. 2023; 24: 898.
- ↑ Buchbinder R, Johnston RV, Rischin KJ, Homik J, Jones C, Golmohammadi K, Kallmes DF. Vertebroplasty for treating spinal fractures due to osteoporosis. Cochrane Library of Systematic Reviews 2018; 11:1465-1858.
- ↑ Whitney E, Alastra AJ. Vertebral Fracture. Available from:https://www.ncbi.nlm.nih.gov/books/NBK547673/ [accessed 26/10/2023]
- ↑ Lee Health. Fixing a Fractured Spine. Available from: https://www.youtube.com/watch?v=QjvKkYehpUI&feature=emb_logo [accessed 26/10/2023]
- ↑ Pratelli E, Cinotti I, Pasquetti P. Rehabilitation in osteoporotic vertebral fractures. Clin Cases Miner Bone Metab. 2010 7(1): 45–47.
- ↑ Barker KL, Newman M, Stallard N, Leal J, Lowe CM, Javaid MK, Noufaily A, Hughes T, Smith D, Gandhi V, Cooper C, Lamb SE; PROVE trial group. Physiotherapy rehabilitation for osteoporotic vertebral fracture-a randomised controlled trial and economic evaluation (PROVE trial). Osteoporos Int. 2020 Feb;31(2):277-89.
- ↑ Hong AR, Kim SW. Effects of resistance exercise on bone health. Endocrinol Metab. 2018 Dec 1;33(4):435-44.
- ↑ Burke TN, Franca FJR, Ferreira de Meneses SR, Pereira RMR, Marques AP. Postural control in elderly women with osteoporosis: comparison of balance, strengthening and stretching exercises. A randomized controlled trial. Clinical Rehabilitation 2012; 26 (11): 1021-1031.
- ↑ De Kam D, Smulders E, Weerdesteyn V, Smits-Engelsman BCM. Exercise interventions to reduce fall-related fractures and their risk factors in individuals with low bone density: a systematic review of randomized controlled trials. Osteoporos Int. 2009;20:2111–25.
- ↑ Karinkanta S, Heinonen A, Sievänen H, Uusi-Rasi K, Pasanen M, Ojala K. A multi-component exercise regimen to prevent functional decline and bone fragility in home-dwelling elderly women: a randomized, controlled trial. Osteoporos Int. 2007;18:453–462.
- ↑ Hourigan SR, Nitz JC, Brauer SG, O'Neill S, Wong J, Richardson CA. Positive effects of exercise on falls and fracture risk in osteopenic women. Osteoporos Int. 2008;19:1077–86.
- ↑ Sinaki M, Lynn SG. Reducing the risk of falls through proprioceptive dynamic posture training in osteoporotic women with kyphotic posturing: a randomized pilot study.Am J Phys Med Rehabil. 2002 Apr;81(4):241-6.
- ↑ Itoi E, Sinaki M.Effect of back-strengthening exercise on posture in healthy women 49 to 65 years of age.Mayo Clin Proc. 1994 Nov;69(11):1054-9. (Level of Evidence: 3B)
- ↑ Bautmans I, Van Arken J, Van Mackelenberg M, Mets T. Rehabilitation using manual mobilization for thoraic kyphosis in elderly postmenopauzal patients with osteoporosis. J Rehabil Med 2010, 42: 129-135. (Level of Evidence: 3B)
- ↑ John Gibbons. Try this Kinesiology Taping technique for poor posture - its incredible. Available from: http://www.youtube.com/watch?v=996cC3ovLEQ[last accessed 21/4/2020]
- ↑ Liu JT et al. Balloon kyphoplasty versus vertebroplasty for treatment of osteoporotic vertebral compression fracture: a prospective, comparative, and randomized clinical study. Osteoporos Int. 2010 Feb;21(2):359-64. Level of Evidence: 1B.
- ↑ Gauthier A, Kanis JA, Jiang Y, Martin M, Compston JE, Borgström F, Cooper C, McCloskey EV. Epidemiological burden of postmenopausal osteoporosis in the UK from 2010 to 2021: estimations from a disease model. Arch Osteoporos 2011 6:179–188.
- ↑ Kim DH, Vaccaro AR. Contemporary Concepts in Spine Care: Osteoporotic compression fractures of the spine; current options and considerations for treatment. The Spine Journal. 2006 6 479–487.
- ↑ 49.0 49.1 NICE. Alendronate, etidronate, risedronate, raloxifene and strontium ranelate for the primary prevention of osteoporotic fragility fractures in postmenopausal women (amended): NICE technology appraisal guidance 160. Manchester: National Institute for Health and Care Excellence, 2011.