Numeric Pain Rating Scale: Difference between revisions
Tomer Yona (talk | contribs) No edit summary |
Tomer Yona (talk | contribs) No edit summary |
||
| Line 67: | Line 67: | ||
For construct validity, the NRS was shown to be highly correlated to the VAS in patients with rheumatic and other chronic pain conditions (pain>6 months): cor-relations range from 0.86 to 0.95.<ref name="8">Ferraz MB, Quaresma MR, Aquino LR, Atra E, Tugwell P, Goldsmith CH. Reliability of pain scales in the assessment of literate and illiterate patients with rheumatoid arthritis. J Rheumatol 1990;17:1022–4.</ref> | For construct validity, the NRS was shown to be highly correlated to the VAS in patients with rheumatic and other chronic pain conditions (pain>6 months): cor-relations range from 0.86 to 0.95.<ref name="8">Ferraz MB, Quaresma MR, Aquino LR, Atra E, Tugwell P, Goldsmith CH. Reliability of pain scales in the assessment of literate and illiterate patients with rheumatoid arthritis. J Rheumatol 1990;17:1022–4.</ref> | ||
===== Minimal clinically important difference (MCID) ===== | ===== Minimal clinically important difference (MCID) ===== | ||
In clinical trials of pregabalin (Medication- known as Lyrica in big parts of the world) for diabetic neuropathy, postherpetic neuralgia, chronic low back pain, fibromyalgia, and OA, analyses of the relationships between changes in pain NRS scores and patient reports of overall improvement, measured using a standard 7-point patient global impression of change, demonstrated a reduction of 2 points, or 30%, on the pain NRS scores to be clinically important <ref>Farrar JT, Young JP Jr, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 2001;94:149–58.</ref>. Similar results were found in low back pain patients when changes in pain NRS scores were compared to patient improvements in pain after physical therapy, using a 15-point Global Rating of Change scale <ref>Childs JD, Piva SR, Fritz JM. Responsiveness of the numeric pain rating scale in patients with low back pain. Spine 2005;30:1331–4</ref> | In clinical trials of pregabalin (Medication- known as Lyrica in big parts of the world) for diabetic neuropathy, postherpetic neuralgia, chronic low back pain, fibromyalgia, and OA, analyses of the relationships between changes in pain NRS scores and patient reports of overall improvement, measured using a standard 7-point patient global impression of change, demonstrated a reduction of 2 points, or 30%, on the pain NRS scores to be clinically important <ref>Farrar JT, Young JP Jr, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 2001;94:149–58.</ref>. Similar results were found in low back pain patients when changes in pain NRS scores were compared to patient improvements in pain after physical therapy, using a 15-point Global Rating of Change scale <ref>Childs JD, Piva SR, Fritz JM. Responsiveness of the numeric pain rating scale in patients with low back pain. Spine 2005;30:1331–4</ref>. In another study<ref name="mich">Michener LA, Snyder AR, Leggin BG. Responsiveness of the numeric pain rating scale in patients with shoulder pain and the effect of surgical status. Journal of sport rehabilitation. 2011 Feb 1;20(1):115.</ref> the MCID was found to be 2 points in patients with shoulder pain. | ||
== References == | == References == | ||
Revision as of 19:21, 12 March 2016
Original Editor - Venus Pagare
Top Contributors - Venus Pagare, Tomer Yona, Kim Jackson, Evan Thomas, Lucinda hampton, Vanessa Rhule, Claire Knott, Lauren Lopez, Melissa Coetsee, 127.0.0.1 and WikiSysop
Purpose[edit | edit source]
The NRS for pain is a unidimensional measure of pain intensity in adults Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title, including those with chronic pain due to rheumatic diseases Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Content[edit | edit source]
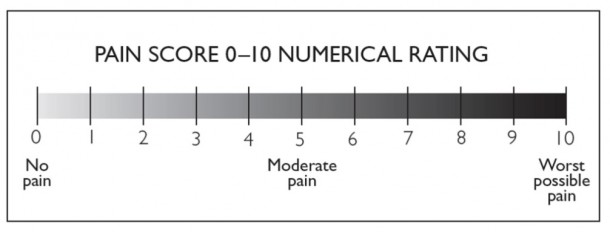
The NRS is a segmented numeric version of the visual analog scale (VAS) in which a respondent selects a whole number (0–10 integers) that best reflects the intensity of their pain Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. The common format is a horizontal bar or line. Similar to the pain VAS, the NRS is anchored by terms describing pain severity extremes. [1]
Number of Items[edit | edit source]
Although various iterations exist, the most commonly used is the 11-item NRS.[2]
Response Options/Scale[edit | edit source]
An 11-point numeric scale (NRS 11) with 0 representing one pain extreme (e.g., “no pain”) and 10 representing the other pain extreme (e.g., “pain as bad as you can imagine” and “worst pain imaginable”)Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Recall period for items[edit | edit source]
Varies, but most commonly respondents are asked to report pain intensity “in the last 24 hours” or average pain intensity. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Obtaining the Scale[edit | edit source]
Available from the web site: http://www.partnersagainstpain.com/printouts/A7012AS2.pdf.
Administration[edit | edit source]
The NRS can be adminis-tered verbally (therefore also by telephone) or graphically for self-completionCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. The respondent is asked to indicate the numeric value on the segmented scale that best describes their pain intensity. [1]
Scoring and Interpretation[edit | edit source]
The number that the respondent indicates on the scale to rate their pain intensity is recorded. Scores range from 0–10. Higher scores indicate greater pain intensity.[1]
Merits and Demerits[edit | edit source]
- The pain NRS takes <1 minute to complete.
- The pain NRS is easy to administer and score.Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title Cite error: Invalid<ref>tag; name cannot be a simple integer. Use a descriptive title - Minimal language translation difficulties supports the use of the NRS across cultures and languagesCite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - Valid and reliable scale to measure pain intensity [1]
- Strengths of this measure over the pain VAS are the ability to be administered both verbally (therefore by telephone) and in writing, as well as its simplicity of scoring.[1]
- However, pain NRS evaluates only 1 component of the pain experience, pain intensity, and therefore does not capture the complexity and idiosyncratic nature of the pain experience or improvements due to symptom fluctuations.
Psychometric Information[edit | edit source]
Development[edit | edit source]
To improve discrimination for detecting relatively small changes, an NRS comprised of numbers along a scale was used in a population of 100 patients with a variety of rheumatic diseases. Variations in pain descriptors used as anchors for end points on the pain NRS have been reported in the literature. However, the methodology used to develop these various anchor terms is unknown.[3] [4]
Acceptability[edit | edit source]
Chronic pain patients prefer the NRS over other measures of pain intensity, including the pain VAS, due to comprehensibility and ease of completion[5]. However, focus groups of patients with chronic back pain and symptomatic hip and knee osteoarthritis (OA) have found that the pain NRS is inadequate in capturing the complexity and idiosyncratic nature of the pain expe-rience or improvements due to symptom fluctuations.[6] [7]
Reliability.[edit | edit source]
High test–retest reliability has been observed in both literate and illiterate patients with rheumatoid arthritis (r = 0.96 and 0.95, respectively) before and after medical consultation. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Validity[edit | edit source]
For construct validity, the NRS was shown to be highly correlated to the VAS in patients with rheumatic and other chronic pain conditions (pain>6 months): cor-relations range from 0.86 to 0.95.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Minimal clinically important difference (MCID)[edit | edit source]
In clinical trials of pregabalin (Medication- known as Lyrica in big parts of the world) for diabetic neuropathy, postherpetic neuralgia, chronic low back pain, fibromyalgia, and OA, analyses of the relationships between changes in pain NRS scores and patient reports of overall improvement, measured using a standard 7-point patient global impression of change, demonstrated a reduction of 2 points, or 30%, on the pain NRS scores to be clinically important [8]. Similar results were found in low back pain patients when changes in pain NRS scores were compared to patient improvements in pain after physical therapy, using a 15-point Global Rating of Change scale [9]. In another study[10] the MCID was found to be 2 points in patients with shoulder pain.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 HAWKER GA. Measures of Adult Pain. Arthritis Care &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Research 2011; 63,S240–S252
- ↑ Williamson A. Pain: a review of three commonly used pain rating scales. ISSUES IN CLINICAL NURSING 2005; 14: 798–804
- ↑ Downie WW, Leatham PA, Rhind VM, Wright V, Branco JA, Anderson JA. Studies with pain rating scales. Ann Rheum Dis 1978;37:378–81.
- ↑ Jensen MP, Karoly P, Braver S. The measurement of clinical pain intensity: a comparison of six methods. Pain 1986;27:117–26.
- ↑ De C Williams AC, Davies HT, Chadury Y. Simple pain rating scales hide complex idiosyncratic meanings. Pain 2000;85:457–63
- ↑ Hawker GA, Davis AM, French MR, Cibere J, Jordan JM, March L, et al. Development and preliminary psychometric testing of a new OA pain measure: an OARSI/OMERACT initiative. Osteoarthritis CartilagefckLR2008;16:409–14
- ↑ Hush JM, Refshauge KM, Sullivan G, De Souza L, McAuley JH. Do numerical rating scales and the Roland-Morris Disability Question-naire capture changes that are meaningful to patients with persistent back pain? Clin Rehabil 2010;24:648–57.
- ↑ Farrar JT, Young JP Jr, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 2001;94:149–58.
- ↑ Childs JD, Piva SR, Fritz JM. Responsiveness of the numeric pain rating scale in patients with low back pain. Spine 2005;30:1331–4
- ↑ Michener LA, Snyder AR, Leggin BG. Responsiveness of the numeric pain rating scale in patients with shoulder pain and the effect of surgical status. Journal of sport rehabilitation. 2011 Feb 1;20(1):115.