Noble's test: Difference between revisions
No edit summary |
No edit summary |
||
| Line 10: | Line 10: | ||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
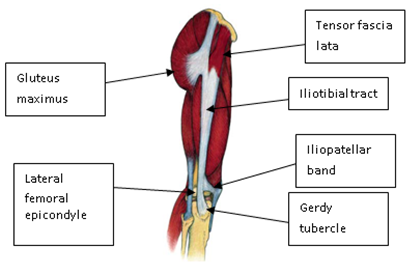
Relevant anatomy related to the test is knowledge of the iliotibial band. It starts as the iliotibial tract, which is a thickening of the fascia lata, originating from the iliac crest. The iliotibial tract continues downward, laterally from the femur. At the greater trochanter, fibres of the tensor fascia lata muscle and gluteus maximus muscle inserts in the iliotibial tract. When approaching the [[Knee|knee]] joint, the iliotibial tract passes the lateral epicondyle of the femur and splits into two structures: the iliopatellar band, and a distal extension inserting at the Gerdy tubercle (Figure 1).<ref name="Dubin 2005"/> | Relevant anatomy related to the test is knowledge of the iliotibial band. It starts as the iliotibial tract, which is a thickening of the fascia lata, originating from the iliac crest. The iliotibial tract continues downward, laterally from the femur. At the greater trochanter, fibres of the tensor fascia lata muscle and gluteus maximus muscle inserts in the iliotibial tract. When approaching the [[Knee|knee]] joint, the iliotibial tract passes the lateral epicondyle of the femur and splits into two structures: the iliopatellar band, and a distal extension inserting at the Gerdy tubercle (Figure 1).<ref name="Dubin 2005"/> | ||
During walking and running, the Iliotibial band is subjected to frictional and compressive forces over the greater trochanter and lateral epicondyle. Repetitive strain, improper footwear, lower extremity mal-alignments and muscle imbalance results into increased friction.<ref>SieunNarine-McKay J. ''Evaluation of outcomes in assessment of iliotibial band syndrome rehabilitation programs'' (Doctoral dissertation, University of British Columbia).https://open.library.ubc.ca/cIRcle/collections/ubctheses/24/items/1.0306928 (accessed on 21/07/2018)</ref> | |||
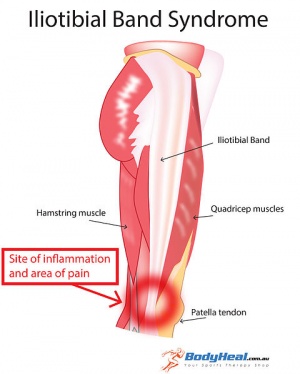
Iliotibial band (ITB) friction syndrome is an overuse injury common in runners, cyclists, weightlifters, skiers, and soccer players. It is characterized by pain over the lateral femoral epicondyle caused by excessive friction between the ITB and the lateral femoral epicondyle. | |||
[[File:Iliotibial Band Syndrome.jpg|center|thumb|Iliotibial band]] | [[File:Iliotibial Band Syndrome.jpg|center|thumb|Iliotibial band]] | ||
Revision as of 06:22, 21 July 2018
Original Editors - Merlin Roggeman
Top Contributors - Evan Thomas, Vidya Acharya, Merlin Roggeman, Admin, Kim Jackson, Chelsea Mclene, Kai A. Sigel, WikiSysop, Rachael Lowe, Oyemi Sillo, Wanda van Niekerk, 127.0.0.1 and Demol Yves
Definition/Description[edit | edit source]
The Noble’s test (also known as Noble's Compression test) is a provocative test of the iliotibial band, developed by Clive Noble. It is commonly used as an indication for iliotibial band syndrome; however, no evidence-based research has been done yet to control the validity of this test. Other tests that could be used are the modified Ober’s test and the Renne Creak test. [1][2][3]
Clinically Relevant Anatomy[edit | edit source]
Relevant anatomy related to the test is knowledge of the iliotibial band. It starts as the iliotibial tract, which is a thickening of the fascia lata, originating from the iliac crest. The iliotibial tract continues downward, laterally from the femur. At the greater trochanter, fibres of the tensor fascia lata muscle and gluteus maximus muscle inserts in the iliotibial tract. When approaching the knee joint, the iliotibial tract passes the lateral epicondyle of the femur and splits into two structures: the iliopatellar band, and a distal extension inserting at the Gerdy tubercle (Figure 1).[4]
During walking and running, the Iliotibial band is subjected to frictional and compressive forces over the greater trochanter and lateral epicondyle. Repetitive strain, improper footwear, lower extremity mal-alignments and muscle imbalance results into increased friction.[5]
Iliotibial band (ITB) friction syndrome is an overuse injury common in runners, cyclists, weightlifters, skiers, and soccer players. It is characterized by pain over the lateral femoral epicondyle caused by excessive friction between the ITB and the lateral femoral epicondyle.
Purpose[edit | edit source]
The purpose of this test is to detect pain, abnormalities, tightness of the iliotibial tract, which can be indicative for the iliotibial band syndrome. It helps to differentiate iliotibial band syndrome from other common causes of lateral knee pain.[2][4]
Technique[edit | edit source]
Put the patient in a supine position. Next, bring the affected knee up to a 90-degree knee flexion and apply pressure with your thumb to the lateral femoral epicondyle. The leg is then extended slowly. When it is extended to approximately 30 degrees, the iliotibial band translates anteriorly over the lateral femoral epicondyle under the examiner's thumb.
If the patient indicates pain at this 30-degree angle, which is similar to when the patient is active, the test is considered positive and it suggests the presence of iliotibial band syndrome.
Evidence[edit | edit source]
Reliability & Validity: Unknown[7]
Clinical Bottom Line[edit | edit source]
This test is indicative of iliotibial band syndrome, but again it must be stated that there have been no studies to indicate the validity of this test.[2][4]
References[edit | edit source]
- ↑ Kasunich NJ. Changes in low back pain in a long distance runner after stretching the iliotibial band. Journal of Chiropractic Medicine 2003; number 1, volume 2; 37-40. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2646955/pdf/main.pdf (accessed 20/05/2011) LEVEL OF EVIDENCE: B
- ↑ 2.0 2.1 2.2 Noble CA. The Treatment of Iliotibial Band Friction Syndrome. Brit. J. Sports Med. 1979; 13; 51-54. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1859686/pdf/brjsmed00261-0005.pdf (accessed 20/05/2011) LEVEL OF EVIDENCE: A2
- ↑ Rosenthal MD. Clinical Testing for Extra-Articular Lateral Knee Pain. A Modification and Combination of Traditional Tests. North American Journal of Sports Physical Therapy 2008; volume 3, number 2; 107-109. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2953323/pdf/najspt-03-107.pdf (accessed 20/05/2011) LEVEL OF EVIDENCE: B
- ↑ 4.0 4.1 4.2 4.3 Dubin J. Evidence Based Treatment for Iliotibial Band Friction Syndrome: Review of Literature. BioMechanics, August 2005. http://dubinchiro.com/iliotibial_band.pdf (accessed 22/05/2011) LEVEL OF EVIDENCE: A1
- ↑ SieunNarine-McKay J. Evaluation of outcomes in assessment of iliotibial band syndrome rehabilitation programs (Doctoral dissertation, University of British Columbia).https://open.library.ubc.ca/cIRcle/collections/ubctheses/24/items/1.0306928 (accessed on 21/07/2018)
- ↑ Physiotutors. Noble Compression / Noble's Test | Iliotibial Band Friction Syndrome ITBS. Available from: https://www.youtube.com/watch?v=PmUGl7ryQOo
- ↑ Knee Orthopaedic Test - A Strategic Approach to Assessing the Knee; University of Western States, College of Chiropractic, Clinic Protocol; Renne; Page No.34; Adopted 12/12. (accessed on 21.07.18 from Knee_Orthopedic_Tests.pdf)