Nine-Hole Peg Test: Difference between revisions
No edit summary |
Chloe Waller (talk | contribs) (Added picture) |
||
| (22 intermediate revisions by 10 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | | ||
'''Original Editor '''- | <div class="editorbox"> | ||
'''Original Editor '''- [[User:Sinead Greenan|Sinead Greenan]] | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Objective | == Objective == | ||
The | The Nine-Hole Peg Test (9HPT) is used to measure finger [[Dexterity Tests|dexterity]] in patients with various [[Neurological Disorders|neurological]] diagnoses<ref>Stroke Engine. Nine Hole Peg Test. Available from: <nowiki>http://strokengine.ca/en/assessments/nine-hole-peg-test-nhpt/</nowiki> (Accessed 11/08/2022)</ref>. | ||
== Intended Population | == Intended Population == | ||
Patients with Stroke, Brain Injury, Parkinson's | Patients with [[Stroke]], [[Traumatic Brain Injury|Brain Injury]], [[Parkinson's]], [[Multiple Sclerosis (MS)|Multiple Sclerosis]] or other neurological conditions<ref name=":0">Shirley Ryan Ability Lab. Nine Hole Peg Test. Available from: <nowiki>https://www.sralab.org/rehabilitation-measures/nine-hole-peg-test</nowiki> (Accessed 11/08/2022)</ref>. | ||
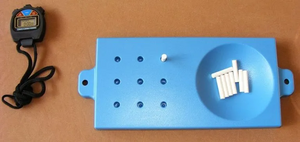
[[File:9-hole-pin-test.webp|thumb|Example of the equipment]] | |||
== Method of Use == | == Method of Use == | ||
<u> | <u>Equipment Required:</u> | ||
* | *Board (wood or plastic): with 9 holes (10 mm diameter, 15 mm depth), placed apart by 32 mm<ref name=":1">Mathiowetz, V., Kashman, N., et al. "Grip and pinch strength: normative data for adults." Arch Phys Med Rehabil 1985 66(2): 69-74</ref><ref>Sommerfeld, D. K., Eek, E. U., et al. "Spasticity after stroke: its occurrence and association with motor impairments and activity limitations." Stroke 2004 35(1): 134-139</ref> or 50 mm<ref name=":2">Heller, A., Wade, D. T., et al. "Arm function after stroke: measurement and recovery over the first three months." Journal of Neurology, Neurosurgery and Psychiatry 1987 50(6): 714-719</ref>. | ||
*A container for the pegs: square box (100 x 100 x 10 mm) apart from the board or a shallow round dish at the end of the board<ref name=":3">Grice, K. O., Vogel, K. A., et al. "Adult norms for a commercially available Nine Hole Peg Test for finger dexterity." The American journal of occupational therapy 2003 57(5): 570-573</ref>. | |||
* | *9 pegs (7 mm diameter, 32 mm length)<ref name=":1" />. | ||
*A stopwatch. | |||
* | |||
* | |||
<u>Description:</u><ref name=":0" /> | |||
*Instruct the patient to take the pegs from a container, one by one, and place them into the holes on the board, as quickly as possible, using only the hand being evaluated. | |||
*Then, instruct the patient to remove the pegs from the holes, one by one, and replace them back into the container. | |||
*The evaluator should start the stopwatch as soon as the patient touches the first peg. | |||
*The evaluator should stop the stopwatch once the last peg is in the container. | |||
<u>Scoring:</u> | |||
*The number of seconds it takes for the patient to complete the test. | |||
*Alternative scoring - the number of pegs placed in 50 or 100 seconds can be recorded. In this case, results are expressed as the number of pegs placed per second. | |||
<u>Example:</u>{{#ev:youtube|kkyfI5OvfJo}} | |||
== Evidence == | == Evidence == | ||
| Line 40: | Line 43: | ||
=== Reliability === | === Reliability === | ||
<u>Test-retest Reliability:</u> | <u>Test-retest Reliability:</u> | ||
<u></u>''Stroke:''<br>(Chen et al, 2009, Acute and Chronic Stroke) <ref>Chen, H. M., Chen, C. C., et al. "Test-retest reproducibility and smallest real difference of 5 hand function tests in patients with stroke." Neurorehabil Neural Repair 2009 23(5): 435-440</ref> | |||
*Excellent test-retest reliability for entire group (ICC = 0.85) | |||
*Adequate test-retest reliability for individuals with hand spasticity (ICC = 0.64). Excellent test-retest reliability for individuals without hand spasticity (ICC = 0.86) | |||
''Parkinson's | ''Parkinson's:'' | ||
(Earhart et al, 2011) <ref>Earhart, G. M., Cavanaugh, J. T., et al. "The 9-hole PEG test of upper extremity function: average values, test-retest reliability, and factors contributing to performance in people with Parkinson disease." J Neurol Phys Ther 2011 35(4): 157-163</ref> | (Earhart et al, 2011) <ref>Earhart, G. M., Cavanaugh, J. T., et al. "The 9-hole PEG test of upper extremity function: average values, test-retest reliability, and factors contributing to performance in people with Parkinson disease." J Neurol Phys Ther 2011 35(4): 157-163</ref> | ||
*Excellent test retest reliability (ICC = 0.88 for dominant hand and ICC = 0.91 for nondominant hand) | *Excellent test retest reliability (ICC = 0.88 for dominant hand and ICC = 0.91 for nondominant hand) | ||
(Wang et al 2011; n = 305; mean age = 32 (26); age range = 3 - 85 years) <ref>Wang, Y. C., Magasi, S. R., et al. "Assessing dexterity function: a comparison of two alternatives for the NIH Toolbox." Journal of Hand Therapy 2011 24(4): 313-320; quiz 321</ref> | ''Healthy Adults:'' | ||
(Wang et al 2011; n = 305; mean age = 32 (26); age range = 3 - 85 years) <ref name=":4">Wang, Y. C., Magasi, S. R., et al. "Assessing dexterity function: a comparison of two alternatives for the NIH Toolbox." Journal of Hand Therapy 2011 24(4): 313-320; quiz 321</ref> | |||
*Excellent test retest reliability (ICC = 0.95 for right hand, ICC = 0.92 for left hand) | *Excellent test retest reliability (ICC = 0.95 for right hand, ICC = 0.92 for left hand) | ||
<br> | |||
<u>Interrater/Intrarater Reliability:</u><br> | |||
<u> | <u></u>''Healthy Adults:'' | ||
< | (Grice et al, 2003) <ref name=":3" /> | ||
( | *Excellent interrater reliability for the right hand (r = 0.984) and the left hand (r = 0.993) | ||
''Stroke:'' | ''Stroke:'' | ||
*Adequate to excellent intrarater reliability (r = 0.68 to 0.99) | (Heller et al, 1987; n = 56; mean age = 72 (9.9) years; assessed < 3 months post-stroke, Acute Stroke) <ref name=":2" /> | ||
*Adequate to excellent intrarater reliability (r = 0.68 to 0.99) | |||
*Excellent interrater reliability (r = 0.75 to 0.99) | *Excellent interrater reliability (r = 0.75 to 0.99) | ||
''Cerebral Palsy:'' | |||
(Mendoza-Sánchez et al, 2022)<ref>Mendoza-Sánchez S, Molina-Rueda F, Florencio LL, Carratalá-Tejada M, Cuesta-Gómez A. [https://pubmed.ncbi.nlm.nih.gov/35212827/ Reliability and agreement of the Nine Hole Peg Test in patients with unilateral spastic cerebral palsy]. Eur J Pediatr. 2022 Jun;181(6):2283-2290.</ref> | |||
* Excellent intra-rater inter-session reliability in patients with spastic unilateral CP | |||
=== Validity === | === Validity === | ||
<u>Criterion Validity:</u> | <u>Criterion Validity:</u> | ||
<u></u>''Stroke:''<br>(Sunderland et al, 1989; n = 38; mean age = 67, Acute Stroke) <ref>Sunderland, A., Tinson, D., et al. "Arm function after stroke. An evaluation of grip strength as a measure of recovery and a prognostic indicator." British Medical Journal 1989 52(11): 1267</ref> | <u></u>''Stroke:''<br>(Sunderland et al, 1989; n = 38; mean age = 67, Acute Stroke) <ref>Sunderland, A., Tinson, D., et al. "Arm function after stroke. An evaluation of grip strength as a measure of recovery and a prognostic indicator." British Medical Journal 1989 52(11): 1267</ref> | ||
*Poor concurrent validity with Frenchay Arm Test: 27% of cases incorrectly classified | *Poor concurrent validity with Frenchay Arm Test: 27% of cases incorrectly classified | ||
*Poor predictive validity: NHPT administered at 1 month did not predict functional outcomes at 6 months post stroke | *Poor predictive validity: NHPT administered at 1 month did not predict functional outcomes at 6 months post stroke | ||
*Adequate correlation with the Purdue Pegboard test (p = -0.74 to -0.75) | ''Healthy Adults:''<br>(Wang et al, 2011) <ref name=":4" /> | ||
*Adequate correlation with the Purdue Pegboard test (p = -0.74 to -0.75) | |||
*Excellent correlation with the Bruininks-Oseretsky Test of Motor Proficiency (p = -0.87 to -0.89) | *Excellent correlation with the Bruininks-Oseretsky Test of Motor Proficiency (p = -0.87 to -0.89) | ||
''Stroke:''<br>(Parker et al, 1986; 2 weeks, 3 & 6 months post onset, Acute Stroke) <ref>Parker, V. M., Wade, D. T., et al. "Loss of arm function after stroke: measurement, frequency, and recovery." Int Rehabil Med 1986 8(2): 69-73</ref><br> | ''Myotonic Dystrophy'': | ||
(Cutelle et al, 2018)<ref>Cutellè C, Rastelli E, Gibellini M, Greco G, Frezza E, Botta A, Terracciano C, Massa R. [https://pubmed.ncbi.nlm.nih.gov/30270126/ Validation of the Nine Hole Peg Test as a measure of dexterity in myotonic dystrophy type 1.] Neuromuscul Disord. 2018 Nov;28(11):947-951.</ref> | |||
* Found to be a reliable, valid and sensitive test of dexterity in Myotonic Dystrophy Type 1. | |||
<u>Construct Validity:</u> | |||
''Stroke:''<br>(Parker et al, 1986; 2 weeks, 3 & 6 months post onset, Acute Stroke) <ref>Parker, V. M., Wade, D. T., et al. "Loss of arm function after stroke: measurement, frequency, and recovery." Int Rehabil Med 1986 8(2): 69-73</ref><br> | |||
*Excellent convergent validity with Motricity Index (r = 0.82) | *Excellent convergent validity with Motricity Index (r = 0.82) | ||
''Healthy children:'' | |||
(Smith, Hong and Presson, 2000)<ref>Smith YA, Hong E, Presson C. [https://pubmed.ncbi.nlm.nih.gov/10883762/ Normative and validation studies of the Nine-hole Peg Test with children.] Percept Mot Skills. 2000 Jun;90(3 Pt 1):823-43</ref> | |||
* Adequate concurrent validity for screening fine motor dexterity of school-age children. | |||
=== Responsiveness === | === Responsiveness === | ||
''Stroke:'' | |||
(Beebe and Lang, 2009, Acute Stroke) <ref>Beebe, J. A. and Lang, C. E. "Relationships and responsiveness of six upper extremity function tests during the first six months of recovery after stroke." J Neurol Phys Ther 2009 33(2): 96-103</ref> | |||
== | {| width="200" border="1" cellpadding="1" cellspacing="1" | ||
|- | |||
| colspan="3" | Responsiveness: | |||
|- | |||
| | |||
| 1–3 months | |||
| 1–6 months | |||
|- | |||
| Grip | |||
| 0.50 | |||
| 0.65 | |||
|- | |||
| Pinch | |||
| 0.52 | |||
| 0.56 | |||
|- | |||
| ARAT | |||
| 0.55 | |||
| 0.63 | |||
|- | |||
| 9HPT | |||
| 0.52 | |||
| 0.66 | |||
|- | |||
| SIS-Hand | |||
| 1.02 | |||
| 0.86 | |||
|} | |||
Responsiveness was calculated using the single population effect size method. Values closer to 1.00 = more responsive to change. Low responsiveness < 0.20; moderate responsiveness < 0.50, and high responsiveness < 0.80 | |||
== References == | == References == | ||
<references /> | |||
[[Category:Outcome_Measures]] | |||
[[Category:Neurological - Outcome Measures]] | |||
[[Category:Stroke]] | |||
[[Category:Stroke - Outcome Measures]] | |||
[[Category:Acquired Brain Injuries]] | |||
[[Category:Parkinson's]] | |||
[[Category:Occupational Health]] | |||
[[Category:Head]] | |||
[[Category:Head - Outcome Measures]] | |||
Latest revision as of 15:55, 21 August 2022
Original Editor - Sinead Greenan
Top Contributors - Sinead Greenan, Kim Jackson, Scott Buxton, Evan Thomas, Oyemi Sillo, Chloe Waller, Admin, Naomi O'Reilly, WikiSysop and Amrita Patro
Objective[edit | edit source]
The Nine-Hole Peg Test (9HPT) is used to measure finger dexterity in patients with various neurological diagnoses[1].
Intended Population[edit | edit source]
Patients with Stroke, Brain Injury, Parkinson's, Multiple Sclerosis or other neurological conditions[2].
Method of Use[edit | edit source]
Equipment Required:
- Board (wood or plastic): with 9 holes (10 mm diameter, 15 mm depth), placed apart by 32 mm[3][4] or 50 mm[5].
- A container for the pegs: square box (100 x 100 x 10 mm) apart from the board or a shallow round dish at the end of the board[6].
- 9 pegs (7 mm diameter, 32 mm length)[3].
- A stopwatch.
Description:[2]
- Instruct the patient to take the pegs from a container, one by one, and place them into the holes on the board, as quickly as possible, using only the hand being evaluated.
- Then, instruct the patient to remove the pegs from the holes, one by one, and replace them back into the container.
- The evaluator should start the stopwatch as soon as the patient touches the first peg.
- The evaluator should stop the stopwatch once the last peg is in the container.
Scoring:
- The number of seconds it takes for the patient to complete the test.
- Alternative scoring - the number of pegs placed in 50 or 100 seconds can be recorded. In this case, results are expressed as the number of pegs placed per second.
Example:
Evidence[edit | edit source]
Reliability[edit | edit source]
Test-retest Reliability:
Stroke:
(Chen et al, 2009, Acute and Chronic Stroke) [7]
- Excellent test-retest reliability for entire group (ICC = 0.85)
- Adequate test-retest reliability for individuals with hand spasticity (ICC = 0.64). Excellent test-retest reliability for individuals without hand spasticity (ICC = 0.86)
Parkinson's:
(Earhart et al, 2011) [8]
- Excellent test retest reliability (ICC = 0.88 for dominant hand and ICC = 0.91 for nondominant hand)
Healthy Adults:
(Wang et al 2011; n = 305; mean age = 32 (26); age range = 3 - 85 years) [9]
- Excellent test retest reliability (ICC = 0.95 for right hand, ICC = 0.92 for left hand)
Interrater/Intrarater Reliability:
Healthy Adults:
(Grice et al, 2003) [6]
- Excellent interrater reliability for the right hand (r = 0.984) and the left hand (r = 0.993)
Stroke:
(Heller et al, 1987; n = 56; mean age = 72 (9.9) years; assessed < 3 months post-stroke, Acute Stroke) [5]
- Adequate to excellent intrarater reliability (r = 0.68 to 0.99)
- Excellent interrater reliability (r = 0.75 to 0.99)
Cerebral Palsy:
(Mendoza-Sánchez et al, 2022)[10]
- Excellent intra-rater inter-session reliability in patients with spastic unilateral CP
Validity[edit | edit source]
Criterion Validity:
Stroke:
(Sunderland et al, 1989; n = 38; mean age = 67, Acute Stroke) [11]
- Poor concurrent validity with Frenchay Arm Test: 27% of cases incorrectly classified
- Poor predictive validity: NHPT administered at 1 month did not predict functional outcomes at 6 months post stroke
Healthy Adults:
(Wang et al, 2011) [9]
- Adequate correlation with the Purdue Pegboard test (p = -0.74 to -0.75)
- Excellent correlation with the Bruininks-Oseretsky Test of Motor Proficiency (p = -0.87 to -0.89)
Myotonic Dystrophy:
(Cutelle et al, 2018)[12]
- Found to be a reliable, valid and sensitive test of dexterity in Myotonic Dystrophy Type 1.
Construct Validity:
Stroke:
(Parker et al, 1986; 2 weeks, 3 & 6 months post onset, Acute Stroke) [13]
- Excellent convergent validity with Motricity Index (r = 0.82)
Healthy children:
(Smith, Hong and Presson, 2000)[14]
- Adequate concurrent validity for screening fine motor dexterity of school-age children.
Responsiveness[edit | edit source]
Stroke:
(Beebe and Lang, 2009, Acute Stroke) [15]
| Responsiveness: | ||
| 1–3 months | 1–6 months | |
| Grip | 0.50 | 0.65 |
| Pinch | 0.52 | 0.56 |
| ARAT | 0.55 | 0.63 |
| 9HPT | 0.52 | 0.66 |
| SIS-Hand | 1.02 | 0.86 |
Responsiveness was calculated using the single population effect size method. Values closer to 1.00 = more responsive to change. Low responsiveness < 0.20; moderate responsiveness < 0.50, and high responsiveness < 0.80
References[edit | edit source]
- ↑ Stroke Engine. Nine Hole Peg Test. Available from: http://strokengine.ca/en/assessments/nine-hole-peg-test-nhpt/ (Accessed 11/08/2022)
- ↑ 2.0 2.1 Shirley Ryan Ability Lab. Nine Hole Peg Test. Available from: https://www.sralab.org/rehabilitation-measures/nine-hole-peg-test (Accessed 11/08/2022)
- ↑ 3.0 3.1 Mathiowetz, V., Kashman, N., et al. "Grip and pinch strength: normative data for adults." Arch Phys Med Rehabil 1985 66(2): 69-74
- ↑ Sommerfeld, D. K., Eek, E. U., et al. "Spasticity after stroke: its occurrence and association with motor impairments and activity limitations." Stroke 2004 35(1): 134-139
- ↑ 5.0 5.1 Heller, A., Wade, D. T., et al. "Arm function after stroke: measurement and recovery over the first three months." Journal of Neurology, Neurosurgery and Psychiatry 1987 50(6): 714-719
- ↑ 6.0 6.1 Grice, K. O., Vogel, K. A., et al. "Adult norms for a commercially available Nine Hole Peg Test for finger dexterity." The American journal of occupational therapy 2003 57(5): 570-573
- ↑ Chen, H. M., Chen, C. C., et al. "Test-retest reproducibility and smallest real difference of 5 hand function tests in patients with stroke." Neurorehabil Neural Repair 2009 23(5): 435-440
- ↑ Earhart, G. M., Cavanaugh, J. T., et al. "The 9-hole PEG test of upper extremity function: average values, test-retest reliability, and factors contributing to performance in people with Parkinson disease." J Neurol Phys Ther 2011 35(4): 157-163
- ↑ 9.0 9.1 Wang, Y. C., Magasi, S. R., et al. "Assessing dexterity function: a comparison of two alternatives for the NIH Toolbox." Journal of Hand Therapy 2011 24(4): 313-320; quiz 321
- ↑ Mendoza-Sánchez S, Molina-Rueda F, Florencio LL, Carratalá-Tejada M, Cuesta-Gómez A. Reliability and agreement of the Nine Hole Peg Test in patients with unilateral spastic cerebral palsy. Eur J Pediatr. 2022 Jun;181(6):2283-2290.
- ↑ Sunderland, A., Tinson, D., et al. "Arm function after stroke. An evaluation of grip strength as a measure of recovery and a prognostic indicator." British Medical Journal 1989 52(11): 1267
- ↑ Cutellè C, Rastelli E, Gibellini M, Greco G, Frezza E, Botta A, Terracciano C, Massa R. Validation of the Nine Hole Peg Test as a measure of dexterity in myotonic dystrophy type 1. Neuromuscul Disord. 2018 Nov;28(11):947-951.
- ↑ Parker, V. M., Wade, D. T., et al. "Loss of arm function after stroke: measurement, frequency, and recovery." Int Rehabil Med 1986 8(2): 69-73
- ↑ Smith YA, Hong E, Presson C. Normative and validation studies of the Nine-hole Peg Test with children. Percept Mot Skills. 2000 Jun;90(3 Pt 1):823-43
- ↑ Beebe, J. A. and Lang, C. E. "Relationships and responsiveness of six upper extremity function tests during the first six months of recovery after stroke." J Neurol Phys Ther 2009 33(2): 96-103