Navicular Drop Test
Original Editor - Evan Thomas
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Purpose
[edit | edit source]
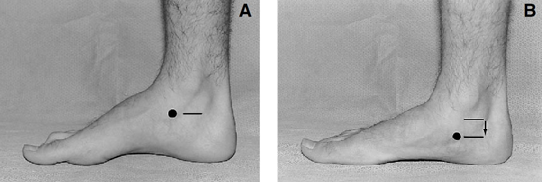
The Navicular Drop Test (NDT) was first described by Brody in 1982 as a means of quantifying the amount of foot pronation in runners (Brody). It’s intended to represent the sagittal plane displacement of the navicular tuberosity from a neutral position to a relaxed position in standing (Vinicombe) (Fig. 1).
Clinical Relevance[edit | edit source]
Excessive navicular drop has been reported in patients with a history of ACL tears (Beckett, Loudon) and is thought to predispose individuals to shin splints (Delacerda) and medial tibial stress syndrome (Moen). It may also help identify individuals who would benefit from prefabricated orthotics and modified activity in those with patellofemoral pain syndrome (Glynn textbook). Headlee et al also found a positive NDT as being indicative of plantar intrinsic muscle fatigue (Headlee).
It has also been suggested that the measurement of navicular position may provide more useful information about the function of the foot in normal walking than frontal plane rear-foot measurements in cases where the navicular undergoes greater displacement than the calcaneus (Headlee). Therefore, the NDT may also be of benefit assessing patients with overuse symptoms of the lower extremity (Vinicombe).
Technique
[edit | edit source]
Position the patient in standing so there is full weight-bearing through the lower extremity and ensure the foot is in the subtalar joint neutral position (“talar head congruent”). Mark the location of the navicular tuberosity and measure its distance from the supporting surface (floor or step). Ask the patient to relax and then measure the amount of sagittal plane excursion of the navicular with a ruler (Fig. 1) (Menz). Alternatively, the test can also be performed in reverse, i.e. measuring from relaxed position up to talar neutral. Many clinicians also choose to perform this test by marking the start and end position of the navicular on an index card placed along the inside of the foot and then measure the change with a ruler.
Figure 1. Measurement of navicular drop. The height of the navicular tuberosity is measured in neutral (A) and relaxed (B) stance positions, and the amount of excursion is measured. Image from Menz 1998.
Evidence[edit | edit source]
Table 1. NDT Values
| Normal | Abnormal/Excessive |
|---|---|
| 6-8mm (Shrader) | ≥10-15mm (Brody, Mueller) |
Table 2. Measurement of navicular height in standing
| Study | Population | Inter-rater reliability (ICC) | Intra-rater reliability (ICC) |
|---|---|---|---|
| Sell et al 1994 | --- | 0.87-0.96 | 0.92-0.95 |
| Shultz et al 2006 | Healthy | 0.56-0.67 | 0.91-0.97 |
| Deng et al 2010 | Healthy | 0.83-0.95 | 0.83-0.95 |
Table 3. Performance of the NDT
| Study | Population | Inter-rater reliability (ICC) | Intra-rater reliability (ICC) |
|---|---|---|---|
| Mueller et al 1993 | Healthy | 0.78-0.83 | --- |
| Sell et al 1994 | --- | 0.73 | 0.83 |
| Shrader et al 2005 | Rheumatoid Arthritis | 0.85-0.97 | 0.90-0.98 |
As with any clinical test, the results should interpreted with caution and informed clinical decisions should be made in light of the error associated with each technique (Vinicombe). The NDT is only one component of an overall lower extremity evaluation and should be used in conjunction with other techniques (Sell).
It should also be noted that despite its relatively widespread use, it lacks normative data from a large cohort of healthy individuals (Cornwall & McPoil 2011) and that other versions of the also test exist, such as one involving a single leg stance relaxed position and the sit-to-stand navicular drop test (SSNDT). And as expected, the classic NDT has been compared to its variants. For example, Deng et al found no correlation between NDT and the sit-to-stand version (SSNDT), suggesting the static measures of navicular height change may not predict dynamic navicular motion during the gait cycle (Deng).
Recent Related Research (from Pubmed)[edit | edit source]
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
Brody TM. Techniques in the evaluation and treatment of the injured runner. Orthop Clin North Am 1982;13:541-58.