Myofascial Pain: Difference between revisions
No edit summary |
No edit summary |
||
| Line 74: | Line 74: | ||
== Diagnosis == | == Diagnosis == | ||
Palpation is the gold standard in identifying the presence of taut bands in muscle. This involves the training and accurate skills of practitioners to identify these taut bands.<br>Palpation of taut bands needs a precise knowledge of muscle anatomy, direction of specific muscle fibres and muscle function.<br>The palpation on muscle must meet several essential criteria and confirmatory observations to identify the presence of trigger points. | Palpation is the gold standard in identifying the presence of taut bands in muscle. This involves the training and accurate skills of practitioners to identify these taut bands.<br>Palpation of taut bands needs a precise knowledge of muscle anatomy, direction of specific muscle fibres and muscle function.<br>The palpation on muscle must meet several essential criteria and confirmatory observations to identify the presence of trigger points. | ||
Confirmatory observations:<br>Visual or tactile local twitch response<br>Referred pain sensation on compression of the taut band<br>SEA confirmed by electromyography | <br><u>Essential criteria:</u><br>Taut band palpable (where muscle is accessible)<br>Exquisite spot of tenderness in a taut band<br>Patient recognition of current pain complaint by pressure of examiner<br>Painful limit to full stretch ROM | ||
<u>Confirmatory observations:</u><br>Visual or tactile local twitch response<br>Referred pain sensation on compression of the taut band<br>SEA confirmed by electromyography | |||
<br> | |||
The interrater and intrarater reliabily of palpation has been a subject of scientific research over the past years. There has been improvement in the methodological quality in recent studies but the main problem rests the lack of rater blinding. It is a problem hard to solve because the reliability of palpation depends on a high rater expertise level. | The interrater and intrarater reliabily of palpation has been a subject of scientific research over the past years. There has been improvement in the methodological quality in recent studies but the main problem rests the lack of rater blinding. It is a problem hard to solve because the reliability of palpation depends on a high rater expertise level. | ||
Revision as of 01:32, 2 February 2015
- Please do not edit unless you are involved in this project, but please come back in the near future to check out new information!!
- If you would like to get involved in this project and earn accreditation for your contributions, please get in touch!
Tips for writing this page:
- Some tips for writing this page.....
Original Editor - Add a link to your Physiopedia profile here.
Top Contributors - German Garcia, Jo Etherton, Kim Jackson, Oyemi Sillo, Vidya Acharya, Alex Benham, Evan Thomas, Vanessa Rhule, WikiSysop, Candace Goh, Lauren Lopez, Lucinda hampton, Sai Kripa and 127.0.0.1
Definition[edit | edit source]
The myofascial pain syndrome is a common clinical problem of muscle pain involving sensory, motor and autonomic symptoms caused by myofascial trigger points.
A myofascial trigger point is defined as a hyperirritable spot, usually within a taut band of skeletal muscle wich is painful on compression and can give rise to characteristic referred pain, motor dysfunction and autonomic phenomena.
Classification and Clinical Presentation[edit | edit source]
Myofascial trigger points are classified into active and latent trigger points. An active trigger point is one with spontaneous pain or pain in response to movement that can trigger local or referred pain. A latent trigger point is a sensitive spot with pain or discomfort only elicited in response to compression. The myofascial trigger points (active or latent) follow common clinical characteristics such as:
- Pain on compression. This may elicit local pain and/or referred pain that is similar to a patient's usual clinical complaint or may aggravate the existing pain.
- Local twitch response. Snapping palpation (compression across the muscle fibers rapidly) may elicit a local twitch response, which is a quick contraction of the muscle fibers in or around the taut band.
- Muscle tightness. Restricted range of stretch, and increased sensitivity to stretch, of muscle fibers in a taut band may cause tightness of the involved muscle.
- Local myasthenia. The muscle with a trigger point may be weak, but usually no atrophy can be noticed.
- Patients with trigger points may have associated localized autonomic phenomena, including vasoconstriction, pilomotor response and hypersecretion.
Spontaneous electrical activity (SEA) has also been recorded in myofascial trigger point sites. The site of this electrical activity is called "active locus". SEA consists of continuous, noise-like action potentials that can range from 5 to 50 µV, with intermittent large amplitude spikes up to 600 µV. This abnormal endplate potential is caused by an excessive release of acetylcholine at the motor endplate. The magnitude of SEA is related to the pain intensity in patients with myofascial trigger points.
Etiology[edit | edit source]
Several possible mechanisms can lead to the development of trigger points, including :
- Prolonged muscle contractures.
- Low-level muscle contractions.
- Postural stress.
- Direct trauma.
- Eccentric contractions in unconditioned or unaccustomed muscle
- Maximal or submaximal concentric contractions.
Initially the taut band formation can reflect a muscle contracture. Prolonged contractures are likely to lead to the formation of latent trigger points, which can eventually evolve into active trigger points.
Myofascial pain can also be caused by low-level muscle contractions which involves a selective overload of the earliest recruited and last derecruited motor units ("Henneman's size principle"). Smaller motor units are recruited before and derecruited after larger ones; as a result, the smaller type I fibers are continuously activated during prolonged motor tasks, wich in turn it can result in metabolically overloaded motor units with a subsequent activation of autogenic destructive processes and muscle pain, this is also known as the Cinderella hypothesis.
Pathophysiology[edit | edit source]
The initial change in muscle that is associated with myofascial pain seems to be the development of the taut band, wich is in term a motor abnormality. Several mechanisms have been hypothesied to explain this motor abnormality, the most accepted one is the "Integrated Hypothesis" first developed by Simmons and later expanded by Gerwin.
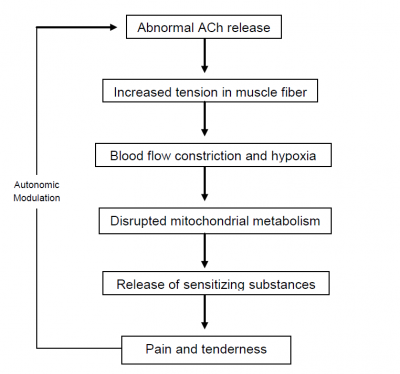
Simmons' integrated hypothesis is a six-link chain that starts with the abnormal release of acetylcholine. This triggers an increase in muscle fiber tension (formation of taut band). The taut band is thought to constrict blood flow that leads to local hypoxia. The reduced oxygen disrupts mitochondrial energy metabolism reducing ATP and leads to tissue distress and the release of sensitizing substances. These sensitizing substances lead to pain by activation of nociceptors and also lead to autonomic modulation that then potentiates the first step: abnormal acetylcholine release.
Gerwin expanded this hypothesis by adding more specific details. He stated that sympathetic nervous system activity augments acetylcholine release and that local hypoperfusion caused by the muscle contraction (taut band) resulted in muscle ischemia or hypoxia leading to an acidification of the pH.
The prolonged ischemia also leads to muscle injury resulting in the release of potassium, bradykinins, cytokines, ATP, and substance P which might stimulate nociceptors in the muscle. The end result is the tenderness and pain observed in myofascial trigger points.
Depolarization of nociceptive neurons causes the release of calcitonin gene-related peptide (CGRP).
CGRP inhibits acetylcholine esterase, increases the sensitivity of acetylcholine receptors and release of acetylcholine resulting in SEA.
In recent studies Shah et al. confirmed the presence of these substances using microdyalisis techniques at trigger point sites. Elevations of substance P, protons (H+), CGRP, bradykinin, serotonin, norepinephrine, TNF, interleukines, and cytokines were found in active trigger points compared to normal muscle or even latent trigger points. The pH of the active trigger point region was decreased as low as pH 4 (normal pH value is 7,4) causing muscle pain and tenderness as well as a decrease in acetylcholine esterase activity resulting in sustained muscle contractions.
Perpetuating Factors[edit | edit source]
In some cases there may be perpetuating factors that have a feed forward effect on myofascial pain. These factors may chronify the pain and tenderness. Perpetuating factors may also have an important role in wide spreading the referred pain by central sensitisation mechanisms.
There are mechanical perpetuating factors such as:
Scoliosis
Leg length discrepancies
Joint hypermobility
Muscle overuse
There are as well systemic or metabolic perpetuating factors such as:
Hypothyroidism
Iron insufficiency
Vitamin D insufficiency
Vitamin B12 insufficiency
Psychosocial perpetuating factors:
Stress
Anxiety
And other possible perpetuating factors:
Infectious diseases
Parasitic diseases (e.g. Lyme disease)
Polymyalgia rheumatica
Use of statin-class drugs
In some cases, managing and correcting an identified perpetuating factor may lead to a complete resolution of pain and may be the sole therapeutic approach needed to relief the patient’s symptoms.
Diagnosis[edit | edit source]
Palpation is the gold standard in identifying the presence of taut bands in muscle. This involves the training and accurate skills of practitioners to identify these taut bands.
Palpation of taut bands needs a precise knowledge of muscle anatomy, direction of specific muscle fibres and muscle function.
The palpation on muscle must meet several essential criteria and confirmatory observations to identify the presence of trigger points.
Essential criteria:
Taut band palpable (where muscle is accessible)
Exquisite spot of tenderness in a taut band
Patient recognition of current pain complaint by pressure of examiner
Painful limit to full stretch ROM
Confirmatory observations:
Visual or tactile local twitch response
Referred pain sensation on compression of the taut band
SEA confirmed by electromyography
The interrater and intrarater reliabily of palpation has been a subject of scientific research over the past years. There has been improvement in the methodological quality in recent studies but the main problem rests the lack of rater blinding. It is a problem hard to solve because the reliability of palpation depends on a high rater expertise level.
Recent research has shown interesting results using magnetic resonance elastography. The technique involves the introduction of cyclic
waves into the muscle, and then using phase contrast imaging to identify tissue
distortions. The speed of the waves is determined from the images. Shear waves
travel more rapidly in stiffer tissues. The taut band can then be distinguished
from the surrounding normal muscle.
Another recent technique used to confirm the extension of myofascial trigger point sites is sonoelastography combined with Doppler imaging.
It uses a clinical ultrasound imaging system with a 12-5 MHz linear array, associated to an external vibration source (hand held vibrating massager) working at cycles of approximately 92Hz.
Doppler imaging is used to identify surrounding blood flows.
Ballyns et al. showed in their study that sonoelastography can be a useful tool to classify myofascial trigger points by area. Larger areas correspond to active trigger points and smaller ones to latent trigger points.
To note that this technique needed preliminary manual rater palpation of trigger points.
Differential Diagnosis[edit | edit source]
Management[edit | edit source]
References[edit | edit source]
References will automatically be added here, see adding references tutorial.