Myocardial Infarction
Original Editors - Jessica King & Melissa Tuemler from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Jessica King, Melissa Tuemler, Lucinda hampton, Vidya Acharya, Kim Jackson, Admin, Elaine Lonnemann, WikiSysop, Wendy Walker, Evan Thomas, Venus Pagare and Karen Wilson
Definition/Description[edit | edit source]
Myocardial infarction (MI) or “heart attack,” is caused by decreased or complete cessation of blood flow to a portion of the myocardium.
Myocardial infarction
- May be “silent” and go undetected, or it could be a catastrophic event leading to hemodynamic deterioration and sudden death.
- Mainly due to underlying coronary artery disease. When the coronary artery is occluded, the myocardium is deprived of oxygen. Prolonged deprivation of oxygen supply to the myocardium can lead to myocardial cell death and necrosis.
- May be associated with ECG changes and elevated biochemical markers such as cardiac troponins
Patients can present with chest discomfort or pressure that can radiate to the neck, jaw, shoulder, or arm.[1]
Etiology[edit | edit source]
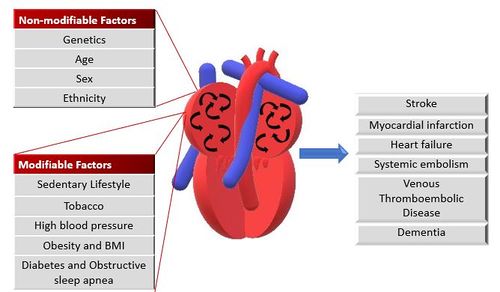
Myocardial infarction is closely associated with coronary artery disease, and the risk factors for MI are similarly associated with the below:
- Smoking
- Abnormal lipid profile/blood apolipoprotein (raised ApoB/ApoA1)
- Hypertension
- Diabetes mellitus
- Abdominal obesity (waist/hip ratio) (greater than 0.90 for males and greater than 0.85 for females)
- Psychosocial factors such as depression, loss of the locus of control, global stress, financial stress, and life events including marital separation, job loss, and family conflicts
- Lack of daily consumption of fruits or vegetables
- Lack of physical activity
Some non-modifiable risk factors for myocardial infarction include:
- Advanced age
- Male gender (males tend to have myocardial infarction earlier in life)
- Genetics (there is an increased risk of MI if a first-degree relative has a history of cardiovascular events before the age of 50). The role of genetic loci that increase the risk for MI is under active investigation[1]
Epidemiology[edit | edit source]
- The most common cause of death and disability in the western world and worldwide is coronary artery disease[1].
- There are 32.4 million myocardial infarctions and strokes worldwide every year.
- Patients with previous myocardial infarction (MI) are the highest risk group for further coronary events.
- Survivors of MI are at increased risk of recurrent infarctions and have an annual death rate of 5% - six times that in people of the same age who do not have coronary heart disease.[2]
- Myocardial Infarctions are the leading cause of death in the industrialized nations of the world. In the United States, there are about 450,000 deaths due to MIs each year. Now 95% of patients hospitalized with an MI will survive due to improvements in emergency response time, and treatment techniques. The risk of having an MI increases with age, but 50% of MIs in the United States occur in people under the age of 65 years old.[3]
Characteristics/Clinical Presentation[edit | edit source]
Myocardial ischemia can present as
- Chest pain, upper extremity pain, mandibular, or epigastric discomfort that occurs during exertion or at rest and is usually not affected by positional changes or active movement of the region. Chest pain (usually retrosternal), sometimes described as the sensation of pressure or heaviness.
- Pain radiating to the left shoulder, neck, or arms (with no obvious precipitating factors), and it may be intermittent or persistent.
- Dyspnea or fatigue.
- Pain lasting more than 20 minutes
- Additional symptoms, such as sweating, nausea, abdominal pain, dyspnea, and syncope, may also be present.
- Atypical with subtle findings such as palpitations
- Dramatic manifestations, such as cardiac arrest. [1]
- Silent ie with no symptoms.
Signs and symptoms vary based on gender.
- The most common symptom experienced by both genders is chest pain or discomfort.
- Women typically experience other symptoms such as SOA, nausea and vomiting, and neck or jaw pain[4].
Medications[edit | edit source]
Following an MI, patients will most likely be prescribed some form of medication for the rest of their lives.
|
Anticoagulants (Warfarin) |
Blood thinner. Decreases clotting ability of the blood, but do not dissolve existing clots. |
| Antiplatelet agents (Aspirin) |
Keeps blood clots from forming by preventing blood platelets from sticking together. |
| ACE inhibitors (Benazepril, Captopril, Enalapril) |
Expands blood vessels and decreases resistance by lowering levels of angiotensin II. Allows blood to flow more easily and makes the heart's work easier or more efficient. |
| Angiotension II Receptor Blockers (Candesartan) |
Prevent angiotension II from having any effects on the heart and blood vessels. This keeps blood pressure from rising. |
| Beta Blockers (Acebutolol) |
Decreases the heart rate and cardiac output, which lowers blood pressure and makes the heart beat more slowly and with less force. |
| Calcium Channel Blockers (Amlodipine) |
Interrupts the movement of calcium into the cells of the heart and blood vessels. May decrease the heart's pumping strength and relax blood vessels. |
| Diuretics (Amiloride) |
Causes the body to rid itself of excess fluids and sodium through urination. Helps to relieve the heart's workload. Also decreases the buildup of fluid in the lungs and other parts of the body, such as the ankles and legs. Different diuretics remove fluid at varied rates and through different methods. |
| Vasodilators (Nitrates) |
Relaxes blood vessels and increases the supply of blood and oxygen to the heart while reducing its workload. Can come in pills to be swallowed, chewable tablets and as a topical application (cream). |
| Digitalis Preparations (Lanoxin) |
Increases the force of the heart's contractions, which can be beneficial in heart failure and for irregular heartbeats. |
| Statins |
Various medications can lower blood cholesterol levels. They may be prescribed individually or in combination with other drugs. They work in the body in different ways. Some affect the liver, some work in the intestines and some interrupt the formation of cholesterol from circulating in the blood. |
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
The three components in the evaluation of the MI are clinical features, ECG findings, and cardiac biomarkers.
ECG
The resting 12 lead ECG is the first-line diagnostic tool for the diagnosis of acute coronary syndrome (ACS). It should be obtained within 10 minutes of the patient’s arrival in the emergency department. Acute MI is often associated with dynamic changes in the ECG waveform. Serial ECG monitoring can provide important clues to the diagnosis if the initial EKG is non-diagnostic at initial presentation.
Biomarker Detection of MI
Cardiac troponins (I and T) are components of the contractile apparatus of myocardial cells and expressed almost exclusively in the heart.
Systemic Involvement
Cardiovascular:
Damage to the heart can lead to some serious effects on the cardiovascular system including decreased peripheral blood flow, dangerous heart arrhythmias, congestive heart failure, and an increased risk for another MI.
Pulmonary:
The pulmonary system is also affected by an MI because there is a decreased level of oxygen saturation due to the damaged heart. Often times during an MI fluid can accumulate in the lungs which could result in damage or infection.
Endocrine:
Many times during an MI the insulin levels spike in individuals, even if they do not have diabetes. Treatment to control the increase in insulin is often required.
Integumentary:
Often times these individuals need to undergo emergency heart surgery, and the incisions need to be monitored for infection.
Medical Management (current best evidence)[edit | edit source]
| Tests | Surgeries | Implanted Medical Devices |
|---|---|---|
| Thrombolysis |
Angioplasty | Left Ventricular Assist Device |
| Artificial Heart Valve Surgery | Pacemaker | |
| Atherectomy | Implantable Cardioverter Defibrillator | |
| Bypass Surgery | ||
| Cardiomyoplasty | ||
| Heart Transplant | ||
| Radiofrequency Ablation | ||
| Stent Placement | ||
| Transmyocardial Revascularization |
Tests/Procedures
- Thrombolysis: procedure typically administered within 3-4 hours of an MI. A clot-dissolving agent is injected into a coronary atery to restore normal blood flow.
Surgeries
- Angioplasty: This procedure greatly increases blood flow through a blocked artery. A balloon is threaded into the blocked artery and is inflated to expand the blocked area so blood flow can be restored. A stent is also commonly placed into the blocked artery during this procedure to ensure that a blockage does not happen again.
- Artificial Heart Valve Surgery: procedure replaces unhealthy or deceased heart valves with new, healthy ones.
- Atherectomy: a catheter is threaded through a blocked artery. The catheter has a rotating sharp end that is used to cut away at plaque formation in the wall of an artery.
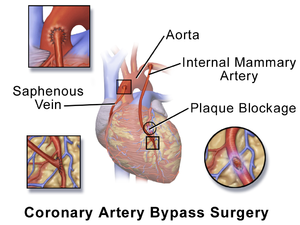
- Bypass Surgery: one of the most common treatment strategies for managing blocked arteries. New passageways are created by using grafts from veins or arteries from other areas of the body to pass the blocked site so blood can flow freely.
- Cardiomyoplasty: currently an experimental treatment where skeletal muscles are wrapped around the patient body over a weak heart. This will improve the heart's pumping motion when stimulated by a pacemaker type of device.
- Heart transplant: removal of a diseased heart that is replaced by a human heart from a donor.
- Radiofrequency Ablation: A catheter with an electrode at its tip is guided through the veins to the heart muscle with real-time, moving X-rays displayed on a video screen. The catheter is placed at the exact site inside the heart where cells give off the electrical signals that stimulate the abnormal heart rhythm. Then a mild, painless radiofrequency energy is transmitted to the pathway that carefully destroys selected heart muscle cells in a very small area (about 1/5 of an inch).
- Stent placement: a wire mesh used to hold open an artery during angioplasty and is then permanently placed in the artery.
- Transmyocardial Revascularization: used to relieve very severe chest pain or angina in patients who are not candidates for a bypass.
Implanted Medical Devices
- Left Ventricular Assist Device: battery-operated, mechanical pump device that is surgically implanted into the heart and is used to maintain the pumping ability of a heart that can't effectively work on its own. This device is typically implanted in patients who are on the waiting list for a heart transplant or suffering from end-stage heart failure.
- Pacemaker: device implanted into heart tissue that sends electrical impulses to help maintain a regular heartbeat. This device is typically used when the hearts "natural pacemaker" becomes defective and causes the heart to beat at an irregular beat.
- Implantable Cardioverter Defibrillator: a device that is implanted into the heart that can send an electrical shock, detect heart rhythm, and at times pace the hearts rhythm.[7]
Physical Therapy Management (Current Best Evidence)[edit | edit source]
Cardiac Rehab may be beneficial to patients of all ages who have had a heart attack, CAD, angina, or CHF. Other individuals who may gain benefits from this include post-surgical CABG, percutaneous intervention (PCI), or coronary angioplasty patients. A medical examination is completed at the initial consultation to determine the needs and limitations of the patient. After the results of the exam are interpreted, the team creates a rehab program and sets goals for treatment. Treatment typically consists of a physical activity program in a group setting where vital signs can consistently be monitored. As the program progresses, the patient is taught how to monitor their own vitals and progresses to more challenging aerobic activities.
Although early mobilization using a cycle ergometer didn't increase physical activity as compared to standard physiotherapy sessions, a randomized controlled trial found Cycle Ergometer Use in the post-operative period following cardiac surgery to be a safe choice for patient rehabilitation[8].
Along with physical activity, patient education is also a very important part of cardiac rehab. Patients may work with a dietician or be given advice on how to stop smoking if necessary.
According to the American Heart Association, the benefits of cardiac rehab include:
- Regular physical activity helps your heart and the rest of your body get stronger and work better. Physical activity improves your energy level and lifts your spirits. It also reduces your chances of future heart problems, including heart attack.
- Counseling and education can help you quit smoking, eat right, lose weight, and lower your blood pressure and cholesterol levels. Counseling may also help you learn to manage stress and to feel better about your health.
- You have the advice and close supervision of healthcare professionals to help you improve your health and lower your risk of future problems. These professionals can also communicate with your primary care doctor or cardiologist. [9]
Prevention - Dietary Modification [edit | edit source]
There are alternative/holistic options that can be employed to prevent an MI or additional MIs, which focus around diet and exercise. Regular aerobic exercise can help decrease an individual’s risk for an MI, and promote better overall health and wellness. Meditation and Yoga are two other options that can help cardiac patients recover after an MI and reduce stress that could lead to another MI in the future.
Nutrition is an important factor in reducing an individual’s risk for an MI. A diet low in fatty acids and cholesterol is important to limit the plaque buildup within arteries.
Differential Diagnosis[edit | edit source]
There are many differential diagnoses for patients experiencing an MI, and because there are many distractions an MI can often be missed. All patients that present with symptoms concurrent with an MI should be treated as a medical emergency.
Possible Differential Diagnoses of a MI include:
| Acute Coronary Syndrome | Dissection, Aortic |
Myopericarditis |
| Angina Pectoris |
Dyspepsia |
Pancreatitis |
| Anxiety |
Endocarditis |
Pericarditis and Cardiac Tamponade |
| Anxiety Disorders |
Esophageal reflux |
Pericarditis, Acute |
| Aortic Dissection |
Esophageal Spasm |
Pleurodynia |
| Aortic Regurgitation |
Esophagitis |
Pneumonia |
| Aortic Stenosis |
Gastritis, Acute |
Pneumothorax |
| Asthma |
Gastroenteritis |
Pneumothorax, Iatrogenic, Spontaneous and Pneumomediastinum |
| Biliary tract disease |
Gastroesophageal Reflux Disease |
Pulmonary Embolism |
| Cholecystitis |
Heart arrhythmias |
Pulmonary Hypertension, Primary |
| Cholecystitis and Biliary Colic |
Heart rupture |
Radicular pain |
| Cholelithiasis |
Herpes Zoster |
Shock, Cardiogenic |
| Chronic Obstructive Pulmonary Disease and Emphysema |
Hypotension |
Stroke Imaging |
| Compartment Syndrome, Abdominal |
Mitral Regurgitation |
Tachycardia myopathy |
| Contusions |
Mitral Valve Prolapse |
Unstable Angina |
| Depression |
Myocarditis |
Ventricular Septal Defect |
Case Reports/ Case Studies[edit | edit source]
Chernyavskiy A, Marchenko A, Lomivorotov V, Doronin D, Alsov S, Nesmachnyy A. Left Ventricular Assist Device Implantation. Texas Heart Institute Journal. (2012, Oct), cited February 15, 2013; 39(5): 627-629. Available from: Academic Search Premier.
Marcuccilli L, Casida J. Overcoming alterations in body image imposed by the left ventricular assist device: a case report. Progress In Transplantation (Aliso Viejo, Calif.). (2012, June), cited February 15, 2013; 22(2): 212-216. Available from: MEDLINE.
Narasimhan S, Krim N, Silverman G, Monrad E. Simultaneous Very Late Stent Thrombosis in Multiple Coronary Arteries. Texas Heart Institute Journal. (2012, Oct), cited February 15, 2013; 39(5): 630-634. Available from: Academic Search Premier.
Resources[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Ojha N, Dhamoon AS. Myocardial Infarction. InStatPearls [Internet] 2019 Dec 4. StatPearls Publishing. Available from:https://www.ncbi.nlm.nih.gov/books/NBK537076/ (last accessed 27.8.2020)
- ↑ WHO Prevention MI Available from:https://www.who.int/cardiovascular_diseases/priorities/secondary_prevention/country/en/index1.html (last accessed 27.8.2020)
- ↑ Cleveland Clinic. Acute Myocardial Infarction. http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/cardiology/acute-myocardial-infarction/#s0015 (12 Feb 2013)
- ↑ American Heart Association. Warning signs of a Heart Attack. http://www.heart.org/HEARTORG/Conditions/HeartAttack/WarningSignsofaHeartAttack/Warning-Signs-of-a-Heart-Attack_UCM_002039_Article.jsp (accessed 10 Feb 2013).
- ↑ American Heart Association. Cardiac Medications. http://www.heart.org/HEARTORG/Conditions/HeartAttack/PreventionTreatmentofHeartAttack/Cardiac-Medications_UCM_303937_Article.jsp (accessed 11 Feb 2013).
- ↑ Patient.co.uk. Myocardial Infarction (Heart Attack). http://www.patient.co.uk/health/myocardial-infarction-heart-attack (Accessed on 12 Feb 2013)
- ↑ American Heart Association. Cardiac Procedures and Surgeries. http://www.heart.org/HEARTORG/Conditions/HeartAttack/PreventionTreatmentofHeartAttack/Cardiac-Procedures-and-Surgeries_UCM_303939_Article.jsp (accessed 11 Feb 2013).
- ↑ Gama Lordello GG, Gonçalves Gama GG, Lago Rosier G, Viana PA, Correia LC, Fonteles Ritt LE. Effects of cycle ergometer use in early mobilization following cardiac surgery: a randomized controlled trial. Clinical Rehabilitation. 2020 Jan 29:0269215520901763.
- ↑ American Heart Association.What is Cardiac Rehab? http://www.heart.org/HEARTORG/Conditions/More/CardiacRehab/What-is-Cardiac-Rehabilitation_UCM_307049_Article.jsp (accessed 11 Feb 2013).
- ↑ Medscape. Myocardial Infarction Differential Diagnosis. http://emedicine.medscape.com/article/155919-differential (accessed 14 Feb 2013).