Myocardial Infarction: Difference between revisions
No edit summary |
No edit summary |
||
| (29 intermediate revisions by 3 users not shown) | |||
| Line 3: | Line 3: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
< | == Introduction == | ||
[[File:Cardiac MRI flow.gif|right|frameless|282x282px]] | |||
Myocardial infarction (MI) (colloquially known as a heart attack) results from interruption of myocardial blood flow and resultant ischaemia and is a leading cause of death worldwide<ref name=":2">Radiopedia [https://radiopaedia.org/articles/myocardial-infarction?lang=gb MI] Available from:https://radiopaedia.org/articles/myocardial-infarction?lang=gb (last accessed 20.2.2021)</ref>. | |||
MI is mainly due to underlying [[Coronary Artery Disease (CAD)|coronary artery disease]]. When the [[Coronary Artery|coronary artery]] is occluded, the myocardium is deprived of oxygen. Prolonged deprivation of oxygen supply to the myocardium can lead to myocardial cell death and necrosis. | |||
Image 1:Cardiac MRI flow. | |||
== Etiology == | |||
Risk factors | |||
* Male > Female | |||
* Age | |||
** >45 years for males | |||
** >55 years for females | |||
= | * Cardiovascular risk factors: smoking, [[hypertension]], low density lipoprotein (LDL) cholesterol, hyperlipidaemia, [[diabetes]], [[obesity]], [[Physical Inactivity|physical inactivity,]] air pollution | ||
* Positive family history: a history of first-degree male relative (i.e. brother, father, son) with MI <55 years of age or first-degree female relative (i.e. mother, sister, daughter) with MI <65 years of age<ref name=":2" /> | |||
Myocardial Infarctions are the leading cause of death in the industrialized nations of the world. In the United States, there are about 450,000 deaths due to MIs each year. Now 95% of patients hospitalized with an MI will survive due to improvements in emergency response time, and treatment techniques. The risk of having an MI increases with age, but 50% of MIs in the United States occur in people under the age of 65 years old.<ref name="Cleveland Clinic">Cleveland Clinic. Acute Myocardial Infarction. http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/cardiology/acute-myocardial-infarction/#s0015 (12 Feb 2013)</ref | == Epidemiology == | ||
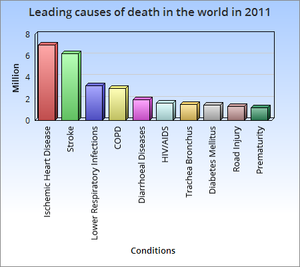
*[[File:Causes of death worldwide 2011.png|right|frameless]]The most common cause of death and disability in the western world and worldwide is coronary artery disease<ref name=":0">Ojha N, Dhamoon AS. [https://www.ncbi.nlm.nih.gov/books/NBK537076/ Myocardial Infarction.] InStatPearls [Internet] 2019 Dec 4. StatPearls Publishing. Available from:https://www.ncbi.nlm.nih.gov/books/NBK537076/ (last accessed 27.8.2020)</ref>. | |||
* There are 32.4 million myocardial infarctions and strokes worldwide every year. | |||
* Patients with previous myocardial infarction (MI) are the highest risk group for further coronary events. | |||
* Survivors of MI are at increased risk of recurrent infarctions and have an annual death rate of 5% - six times that in people of the same age who do not have coronary heart disease.<ref name=":1">WHO Prevention MI Available from:https://www.who.int/cardiovascular_diseases/priorities/secondary_prevention/country/en/index1.html (last accessed 27.8.2020)</ref> | |||
* Myocardial Infarctions are the leading cause of death in the industrialized nations of the world. In the United States, there are about 450,000 deaths due to MIs each year. Now 95% of patients hospitalized with an MI will survive due to improvements in emergency response time, and treatment techniques. The risk of having an MI increases with age, but 50% of MIs in the United States occur in people under the age of 65 years old.<ref name="Cleveland Clinic">Cleveland Clinic. Acute Myocardial Infarction. http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/cardiology/acute-myocardial-infarction/#s0015 (12 Feb 2013)</ref> | |||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
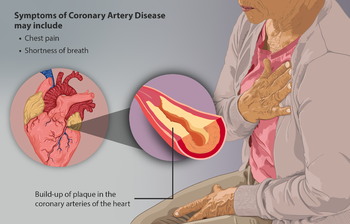
[[File:Coronary Artery Disease.png|right|frameless|350x350px]] | |||
Myocardial ischemia can present as | |||
* Chest pain/tightness, which may radiate down the left arm or into the jaw<ref name=":2" /> | |||
* Dramatic manifestations, such as cardiac arrest. <ref name=":0" /> | |||
* Silent" ischaemia can occur in those with poor visceral sensation (diabetics, post-cardiothoracic surgery) and may manifest with other symptoms of myocardial compromise, e.g. breathlessness<ref name=":2" /> | |||
Signs and symptoms vary based on gender. | |||
* The most common symptom experienced by both genders is chest pain or discomfort. | |||
* Women typically experience other symptoms such as SOA, nausea and vomiting, and neck or jaw pain<ref name="American Heart">American Heart Association. Warning signs of a Heart Attack. http://www.heart.org/HEARTORG/Conditions/HeartAttack/WarningSignsofaHeartAttack/Warning-Signs-of-a-Heart-Attack_UCM_002039_Article.jsp (accessed 10 Feb 2013).</ref>. | |||
{{#ev:youtube|Es-Cr9uRXgQ}} | |||
== Evaluation/Laboratory markers == | |||
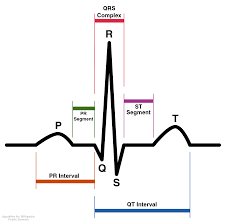
[[File:Normal ecg one wavelength.png|right|frameless|226x226px]]The mainstay of diagnosis revolves around: Cardiac biomarkers; ECG findings; and clinical features. | |||
* Cardiac biomarkers: Troponin is a protein of key importance in the functioning of skeletal and cardiac muscle. It forms part of the contractile mechanism. Cardiac troponin is the preferred biochemical standard for diagnosis of MI because it is the most sensitive and cardiospecific marker. AMI should be diagnosed in the presence of an increasing and/or decreasing pattern of cardiac troponin concentrations, with at least 1 value above the 99th percentile of a healthy reference population if there are symptoms suggestive of myocardial ischemia, or [[Electrocardiogram|ECG]]: changes indicative of ischemia, or imaging evidence of new loss of viable myocardium or new wall-motion abnormality.<ref>Katus HA, Giannitsis E, Jaffe AS. [https://academic.oup.com/clinchem/article/58/1/39/5620685 Interpreting changes in troponin—clinical judgment is essential]. Clinical chemistry. 2012 Jan 1;58(1):39-43.Available from:https://academic.oup.com/clinchem/article/58/1/39/5620685 (accessed 20.2.2021)</ref> | |||
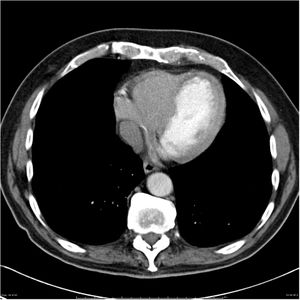
Image 5: Normal ECG wavelength [[File:Subacute-left-anterior-descending-myocardial-infarct.jpg|right|frameless]]Imaging is used to assess myocardial perfusion, myocardial viability, myocardial thickness, thickening and motion, and the effect of myocyte loss on the kinetics of para-magnetic or radio-opaque contrast agents indicating myocardial fibrosis or scars. | |||
* Some [[Medical Imaging|imaging]] modalities that can be used are echocardiography, radionuclide imaging, and cardiac magnetic resonance imaging (cardiac MRI). | |||
* Image R: Subacute-left-anterior-descending-myocardial-infarct | |||
== Pathology == | |||
Coronary artery disease with rupture of an [[Atherosclerosis|atherosclerotic]] plaque resulting in occlusion (local thrombosis/dissection) is the major cause of myocardial infarctions. Other causes include: | |||
* Ischaemic imbalance (i.e. myocardial oxygen supply/demand imbalance) | |||
* In critically-ill patients or in the setting of major (non-cardiac) [[Surgery and General Anaesthetic|surgery]] | |||
* Vasospasm | |||
* Iatrogenic, e.g. during revascularisation procedures<ref name=":2" /> | |||
== Treatment == | |||
[[File:Exercise older person.jpg|thumb]] | |||
The diagnosis and management of patients with MI is best done with an interprofessional team. In most hospitals, there are cardiology teams that are dedicated to the management of these patients. | |||
For patients who present with chest pain, the key to the management of MI is time to treatment. | |||
* A cardiology consult should be made immediately to ensure that the patient gets treated within the time frame recommendations. | |||
* As MI can be associated with several serious complications, these patients are best managed in an ICU setting. | |||
Long term management | |||
There is no cure for ischemic heart disease, and all treatments are symptom-oriented. | |||
* The key to improving outcomes is to prevent coronary artery disease. | |||
* The primary care provider, physiotherapist and nurse practitioner should educate the patient on the benefits of a healthy [[Gut Brain Axis (GBA)|diet]], the importance of controlling blood pressure and diabetes, exercising regularly, discontinuing smoking, maintaining healthy body weight, and remaining compliant with medications. | |||
* The pharmacist should educate the patient on types of medication used to treat ischemic heart disease, their benefits, and potential adverse effects. | |||
== | == Prognosis == | ||
[[File:Emergency-and-accident-sign1774530171.jpg|right|frameless]] | |||
Acute MI carries a mortality rate of 5-30%; the majority of deaths occur prior to arrival to the hospital. | |||
* Within the first year after an MI, there is an additional mortality rate of 5% to 12%. | |||
* Overall prognosis depends on the extent of heart muscle damage and ejection fraction. Patients with preserved left ventricular function tend to have good outcomes. | |||
Factors that worsen prognosis include: | |||
* Diabetes | |||
* Advanced age | |||
* Delayed reperfusion | |||
* Low ejection fraction | |||
* Presence of congestive heart failure | |||
* Elevations in C-reactive protein and B-type natriuretic peptide (BNP) levels | |||
* Depression<ref name=":0" /> | |||
== | == Physical Therapy Management == | ||
[[File:Treadmill walk.jpg|right|frameless]] | |||
[[Cardiac Rehabilitation|Cardiac Rehab]] is beneficial to patients of all ages who have had a heart attack, CAD, angina, or CHF. Other individuals who may gain benefits from this include post-surgical CABG, percutaneous intervention (PCI), or coronary angioplasty patients. | |||
== Indications for Cardiac Rehab == | |||
* | * A medical examination is completed at the initial consultation to determine the needs and limitations of the patient. | ||
* | * The results of the exam are interpreted, the team creates a rehab program and sets goals for treatment. | ||
* Treatment typically consists of a physical activity program in a group setting where vital signs can consistently be monitored. As the program progresses, the patient is taught how to monitor their own vitals and progresses to more challenging aerobic activities. | |||
* Cycle Ergometer Use in the post-operative period following cardiac surgery is a safe choice for patient rehabilitation<ref>Gama Lordello GG, Gonçalves Gama GG, Lago Rosier G, Viana PA, Correia LC, Fonteles Ritt LE. [https://pubmed.ncbi.nlm.nih.gov/31994405/ Effects of cycle ergometer use in early mobilization following cardiac surgery: a randomized controlled trial.] Clinical Rehabilitation. 2020 Jan 29:0269215520901763.</ref>. | |||
* Along with physical activity, patient education is also a very important part of cardiac rehab. Patients may work with a dietician or be given advice on how to stop smoking if necessary. | |||
According to the ''American Heart Association'', the benefits of cardiac rehab include: | |||
*Regular physical activity helps your heart and the rest of your body get stronger and work better. Physical activity improves your energy level and lifts your spirits. It also reduces your chances of future heart problems, including heart attack. | |||
*Counseling and education can help you quit smoking, eat right, lose weight, and lower your blood pressure and cholesterol levels. Counseling may also help you learn to manage stress and to feel better about your health. | |||
*You have the advice and close supervision of healthcare professionals to help you improve your health and lower your risk of future problems. These professionals can also communicate with your primary care doctor or cardiologist. <ref name="American 4">American Heart Association.What is Cardiac Rehab? http://www.heart.org/HEARTORG/Conditions/More/CardiacRehab/What-is-Cardiac-Rehabilitation_UCM_307049_Article.jsp (accessed 11 Feb 2013).</ref> | |||
== Prevention == | |||
Evidence based interventions for secondary prevention include the use of aspirin, beta-blockers, angiotensin converting enzyme inhibitors; lipid lowering drugs and other anti- hypertensives, as well as modifying lifestyle related risk behaviours. | |||
'''Physical exercise''' | |||
Although the role of exercise alone in reducing cardiovascular outcomes is not clear, systematic reviews of RCTs have found that cardiac rehabilitation which includes physical exercise improves coronary risk factors and reduces the risk of major cardiac events in people after MI.<ref name=":1" /> | |||
'''Dietary Modification '''[[File:Nutritous Food.jpg|right|frameless|216x216px]]RCTs have found that advising people with MI to eat more fish, fruit and vegetables, bread, pasta, potatoes, olive oil and margarine may result in a substantial survival advantage<ref name=":1" />. | |||
'''Stopping smoking''' | |||
Following an MI, patients will most likely be prescribed some form of medication for the rest of their lives. | Apart from these pharmacological measures for secondary prevention, evidence is available that lifestyle measures such as stopping smoking, encouraging a healthy diet and exercise can also significantly contribute to reduction in cardiovascular mortality in people with established CVD. Evidence from epidemiological studies indicates that people with coronary heart disease who stop smoking rapidly reduce their risk of recurrent coronary events or death. In the case of stroke survivors, observational studies have shown that the excess risk of stroke among former smokers largely disappeared 2-4 years after smoking cessation<ref name=":1" />. | ||
== Medications == | |||
Following an MI, patients will most likely be prescribed some form of medication for the rest of their lives<ref name="American Heart 3">American Heart Association. Cardiac Medications. http://www.heart.org/HEARTORG/Conditions/HeartAttack/PreventionTreatmentofHeartAttack/Cardiac-Medications_UCM_303937_Article.jsp (accessed 11 Feb 2013).</ref>. | |||
{| cellspacing="1" cellpadding="1" border="1" style="width: 743px; height: 543px;" | {| cellspacing="1" cellpadding="1" border="1" style="width: 743px; height: 543px;" | ||
|- | |- | ||
| Vasodilators (Nitrates)<br> | | Vasodilators (Nitrates)<br> | ||
| Line 85: | Line 123: | ||
| Various medications can lower blood cholesterol levels. They may be prescribed individually or in combination with other drugs. They work in the body in different ways. Some affect the liver, some work in the intestines and some interrupt the formation of cholesterol from circulating in the blood.<br> | | Various medications can lower blood cholesterol levels. They may be prescribed individually or in combination with other drugs. They work in the body in different ways. Some affect the liver, some work in the intestines and some interrupt the formation of cholesterol from circulating in the blood.<br> | ||
|} | |} | ||
== Resources == | == Resources == | ||
| Line 334: | Line 133: | ||
*[http://www.webmd.com/heart-disease/understanding-heart-attack-basics WebMD] | *[http://www.webmd.com/heart-disease/understanding-heart-attack-basics WebMD] | ||
== References == | == References == | ||
| Line 347: | Line 144: | ||
[[Category:Cardiovascular Disease - Conditions]] | [[Category:Cardiovascular Disease - Conditions]] | ||
[[Category:Cardiovascular Disease - Conditions]] | [[Category:Cardiovascular Disease - Conditions]] | ||
[[Category:Conditions]] | |||
Latest revision as of 08:06, 20 February 2021
Original Editors - Jessica King & Melissa Tuemler from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Jessica King, Melissa Tuemler, Lucinda hampton, Vidya Acharya, Kim Jackson, Admin, Elaine Lonnemann, WikiSysop, Wendy Walker, Evan Thomas, Venus Pagare and Karen Wilson
Introduction[edit | edit source]
Myocardial infarction (MI) (colloquially known as a heart attack) results from interruption of myocardial blood flow and resultant ischaemia and is a leading cause of death worldwide[1].
MI is mainly due to underlying coronary artery disease. When the coronary artery is occluded, the myocardium is deprived of oxygen. Prolonged deprivation of oxygen supply to the myocardium can lead to myocardial cell death and necrosis.
Image 1:Cardiac MRI flow.
Etiology[edit | edit source]
Risk factors
- Male > Female
- Age
- >45 years for males
- >55 years for females
- Cardiovascular risk factors: smoking, hypertension, low density lipoprotein (LDL) cholesterol, hyperlipidaemia, diabetes, obesity, physical inactivity, air pollution
- Positive family history: a history of first-degree male relative (i.e. brother, father, son) with MI <55 years of age or first-degree female relative (i.e. mother, sister, daughter) with MI <65 years of age[1]
Epidemiology[edit | edit source]
- The most common cause of death and disability in the western world and worldwide is coronary artery disease[2].
- There are 32.4 million myocardial infarctions and strokes worldwide every year.
- Patients with previous myocardial infarction (MI) are the highest risk group for further coronary events.
- Survivors of MI are at increased risk of recurrent infarctions and have an annual death rate of 5% - six times that in people of the same age who do not have coronary heart disease.[3]
- Myocardial Infarctions are the leading cause of death in the industrialized nations of the world. In the United States, there are about 450,000 deaths due to MIs each year. Now 95% of patients hospitalized with an MI will survive due to improvements in emergency response time, and treatment techniques. The risk of having an MI increases with age, but 50% of MIs in the United States occur in people under the age of 65 years old.[4]
Characteristics/Clinical Presentation[edit | edit source]
Myocardial ischemia can present as
- Chest pain/tightness, which may radiate down the left arm or into the jaw[1]
- Dramatic manifestations, such as cardiac arrest. [2]
- Silent" ischaemia can occur in those with poor visceral sensation (diabetics, post-cardiothoracic surgery) and may manifest with other symptoms of myocardial compromise, e.g. breathlessness[1]
Signs and symptoms vary based on gender.
- The most common symptom experienced by both genders is chest pain or discomfort.
- Women typically experience other symptoms such as SOA, nausea and vomiting, and neck or jaw pain[5].
Evaluation/Laboratory markers[edit | edit source]
The mainstay of diagnosis revolves around: Cardiac biomarkers; ECG findings; and clinical features.
- Cardiac biomarkers: Troponin is a protein of key importance in the functioning of skeletal and cardiac muscle. It forms part of the contractile mechanism. Cardiac troponin is the preferred biochemical standard for diagnosis of MI because it is the most sensitive and cardiospecific marker. AMI should be diagnosed in the presence of an increasing and/or decreasing pattern of cardiac troponin concentrations, with at least 1 value above the 99th percentile of a healthy reference population if there are symptoms suggestive of myocardial ischemia, or ECG: changes indicative of ischemia, or imaging evidence of new loss of viable myocardium or new wall-motion abnormality.[6]
Image 5: Normal ECG wavelength
Imaging is used to assess myocardial perfusion, myocardial viability, myocardial thickness, thickening and motion, and the effect of myocyte loss on the kinetics of para-magnetic or radio-opaque contrast agents indicating myocardial fibrosis or scars.
- Some imaging modalities that can be used are echocardiography, radionuclide imaging, and cardiac magnetic resonance imaging (cardiac MRI).
- Image R: Subacute-left-anterior-descending-myocardial-infarct
Pathology[edit | edit source]
Coronary artery disease with rupture of an atherosclerotic plaque resulting in occlusion (local thrombosis/dissection) is the major cause of myocardial infarctions. Other causes include:
- Ischaemic imbalance (i.e. myocardial oxygen supply/demand imbalance)
- In critically-ill patients or in the setting of major (non-cardiac) surgery
- Vasospasm
- Iatrogenic, e.g. during revascularisation procedures[1]
Treatment[edit | edit source]
The diagnosis and management of patients with MI is best done with an interprofessional team. In most hospitals, there are cardiology teams that are dedicated to the management of these patients.
For patients who present with chest pain, the key to the management of MI is time to treatment.
- A cardiology consult should be made immediately to ensure that the patient gets treated within the time frame recommendations.
- As MI can be associated with several serious complications, these patients are best managed in an ICU setting.
Long term management
There is no cure for ischemic heart disease, and all treatments are symptom-oriented.
- The key to improving outcomes is to prevent coronary artery disease.
- The primary care provider, physiotherapist and nurse practitioner should educate the patient on the benefits of a healthy diet, the importance of controlling blood pressure and diabetes, exercising regularly, discontinuing smoking, maintaining healthy body weight, and remaining compliant with medications.
- The pharmacist should educate the patient on types of medication used to treat ischemic heart disease, their benefits, and potential adverse effects.
Prognosis[edit | edit source]
Acute MI carries a mortality rate of 5-30%; the majority of deaths occur prior to arrival to the hospital.
- Within the first year after an MI, there is an additional mortality rate of 5% to 12%.
- Overall prognosis depends on the extent of heart muscle damage and ejection fraction. Patients with preserved left ventricular function tend to have good outcomes.
Factors that worsen prognosis include:
- Diabetes
- Advanced age
- Delayed reperfusion
- Low ejection fraction
- Presence of congestive heart failure
- Elevations in C-reactive protein and B-type natriuretic peptide (BNP) levels
- Depression[2]
Physical Therapy Management[edit | edit source]
Cardiac Rehab is beneficial to patients of all ages who have had a heart attack, CAD, angina, or CHF. Other individuals who may gain benefits from this include post-surgical CABG, percutaneous intervention (PCI), or coronary angioplasty patients.
Indications for Cardiac Rehab[edit | edit source]
- A medical examination is completed at the initial consultation to determine the needs and limitations of the patient.
- The results of the exam are interpreted, the team creates a rehab program and sets goals for treatment.
- Treatment typically consists of a physical activity program in a group setting where vital signs can consistently be monitored. As the program progresses, the patient is taught how to monitor their own vitals and progresses to more challenging aerobic activities.
- Cycle Ergometer Use in the post-operative period following cardiac surgery is a safe choice for patient rehabilitation[7].
- Along with physical activity, patient education is also a very important part of cardiac rehab. Patients may work with a dietician or be given advice on how to stop smoking if necessary.
According to the American Heart Association, the benefits of cardiac rehab include:
- Regular physical activity helps your heart and the rest of your body get stronger and work better. Physical activity improves your energy level and lifts your spirits. It also reduces your chances of future heart problems, including heart attack.
- Counseling and education can help you quit smoking, eat right, lose weight, and lower your blood pressure and cholesterol levels. Counseling may also help you learn to manage stress and to feel better about your health.
- You have the advice and close supervision of healthcare professionals to help you improve your health and lower your risk of future problems. These professionals can also communicate with your primary care doctor or cardiologist. [8]
Prevention[edit | edit source]
Evidence based interventions for secondary prevention include the use of aspirin, beta-blockers, angiotensin converting enzyme inhibitors; lipid lowering drugs and other anti- hypertensives, as well as modifying lifestyle related risk behaviours.
Physical exercise
Although the role of exercise alone in reducing cardiovascular outcomes is not clear, systematic reviews of RCTs have found that cardiac rehabilitation which includes physical exercise improves coronary risk factors and reduces the risk of major cardiac events in people after MI.[3]
Dietary Modification
RCTs have found that advising people with MI to eat more fish, fruit and vegetables, bread, pasta, potatoes, olive oil and margarine may result in a substantial survival advantage[3].
Stopping smoking
Apart from these pharmacological measures for secondary prevention, evidence is available that lifestyle measures such as stopping smoking, encouraging a healthy diet and exercise can also significantly contribute to reduction in cardiovascular mortality in people with established CVD. Evidence from epidemiological studies indicates that people with coronary heart disease who stop smoking rapidly reduce their risk of recurrent coronary events or death. In the case of stroke survivors, observational studies have shown that the excess risk of stroke among former smokers largely disappeared 2-4 years after smoking cessation[3].
Medications[edit | edit source]
Following an MI, patients will most likely be prescribed some form of medication for the rest of their lives[9].
| Vasodilators (Nitrates) |
Relaxes blood vessels and increases the supply of blood and oxygen to the heart while reducing its workload. Can come in pills to be swallowed, chewable tablets and as a topical application (cream). |
| Digitalis Preparations (Lanoxin) |
Increases the force of the heart's contractions, which can be beneficial in heart failure and for irregular heartbeats. |
| Statins |
Various medications can lower blood cholesterol levels. They may be prescribed individually or in combination with other drugs. They work in the body in different ways. Some affect the liver, some work in the intestines and some interrupt the formation of cholesterol from circulating in the blood. |
Resources[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Radiopedia MI Available from:https://radiopaedia.org/articles/myocardial-infarction?lang=gb (last accessed 20.2.2021)
- ↑ 2.0 2.1 2.2 Ojha N, Dhamoon AS. Myocardial Infarction. InStatPearls [Internet] 2019 Dec 4. StatPearls Publishing. Available from:https://www.ncbi.nlm.nih.gov/books/NBK537076/ (last accessed 27.8.2020)
- ↑ 3.0 3.1 3.2 3.3 WHO Prevention MI Available from:https://www.who.int/cardiovascular_diseases/priorities/secondary_prevention/country/en/index1.html (last accessed 27.8.2020)
- ↑ Cleveland Clinic. Acute Myocardial Infarction. http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/cardiology/acute-myocardial-infarction/#s0015 (12 Feb 2013)
- ↑ American Heart Association. Warning signs of a Heart Attack. http://www.heart.org/HEARTORG/Conditions/HeartAttack/WarningSignsofaHeartAttack/Warning-Signs-of-a-Heart-Attack_UCM_002039_Article.jsp (accessed 10 Feb 2013).
- ↑ Katus HA, Giannitsis E, Jaffe AS. Interpreting changes in troponin—clinical judgment is essential. Clinical chemistry. 2012 Jan 1;58(1):39-43.Available from:https://academic.oup.com/clinchem/article/58/1/39/5620685 (accessed 20.2.2021)
- ↑ Gama Lordello GG, Gonçalves Gama GG, Lago Rosier G, Viana PA, Correia LC, Fonteles Ritt LE. Effects of cycle ergometer use in early mobilization following cardiac surgery: a randomized controlled trial. Clinical Rehabilitation. 2020 Jan 29:0269215520901763.
- ↑ American Heart Association.What is Cardiac Rehab? http://www.heart.org/HEARTORG/Conditions/More/CardiacRehab/What-is-Cardiac-Rehabilitation_UCM_307049_Article.jsp (accessed 11 Feb 2013).
- ↑ American Heart Association. Cardiac Medications. http://www.heart.org/HEARTORG/Conditions/HeartAttack/PreventionTreatmentofHeartAttack/Cardiac-Medications_UCM_303937_Article.jsp (accessed 11 Feb 2013).