Musculoskeletal Injury Risk Screening: Difference between revisions
(added references and formatting to section on consequences of sports injury) |
Kim Jackson (talk | contribs) No edit summary |
||
| (46 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Wanda van Niekerk|Wanda van Niekerk]] based on the course by [https://members.physio-pedia.com/course_tutor/lee-herrington/ Lee Herrington]<br> | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | |||
<div class="editorbox"> | |||
'''Original Editor '''- [[User: | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | |||
</div> | |||
== Introduction == | == Introduction == | ||
[[File:Injury screen.jpeg|right|frameless]] | |||
Screening is a valuable process for athletes and is commonly practised in several elite sports. One of the common elements of a periodic medical assessment of athletes, is the musculoskeletal screening or examination. For many years, physiotherapists have screened athletes with the aim of identifying the athletes at risk for [[Sport Injury Classification|injury]], so that they can then implement injury prevention programmes for these athletes. More recently, the focus has, however, shifted from using screening to predict injuries to rather using screening to identify possible predispositions to injury. | |||
== Reasons for the Periodic Medical Assessment of Athletes == | == Reasons for the Periodic Medical Assessment of Athletes == | ||
The main reason for the periodic medical assessment of athletes is to safeguard sports participation, but there are many | The main reason for the periodic medical assessment of athletes is to safeguard sports participation, but there are many other additional benefits, including:<ref>Targett S, Clarsen B. Periodic medical assessment of athletes. In: Brukner P, Clarsen B, Cook J, Cools A, Crossley K, Hutchinson M, McCroy P, Bahr R, Khan K. Brukner and Khan's Clinical Sports Medicine: Injuries, Volume 1, 5e. Sydney: McGraw Hill Education. 2017</ref><ref>Nabhan D, Taylor D, Lewis M, Bahr R. Protecting the world’s finest athletes: periodic health evaluation practices of the top performing National Olympic Committees from the 2016 Rio or 2018 PyeongChang Olympic Games. British Journal of Sports Medicine. 2021 Sep 1;55(17):961-7.</ref> | ||
* Identification of medical conditions that contraindicate sports participation | * Identification of medical conditions that contraindicate sports participation | ||
| Line 18: | Line 13: | ||
* Athlete education | * Athlete education | ||
* Baseline testing | * Baseline testing | ||
* | * Developing rapport with the athlete | ||
* Specific | * Specific screening | ||
** Cardiac screening | ** Cardiac screening | ||
** Screening for unknown illnesses | ** Screening for unknown illnesses | ||
** Screening for risk factors for future injury | ** Screening for risk factors for future injury | ||
Read more: [[Screening in Sport|Screening in sport]] and [[Pre-participation Screening]] | |||
== Why Screen for Injury Risk? == | == Why Screen for Injury Risk? == | ||
Injury rates in sports are increasing despite the increased professionalism of sports science and sports medicine support teams. Although participation in sport is encouraged as part of a healthy lifestyle, the sport-related injury burden is high.<ref>Emery CA, Pasanen K. [https://delfamdoc.org/wp-content/uploads/2019/11/current-trends-sports-injury-prevention.pdf Current trends in sport injury prevention.] Best Practice & Research Clinical Rheumatology. 2019 Feb 1;33(1):3-15.</ref> | Injury rates in sports are increasing despite the increased professionalism of sports science and the use of sports medicine support teams. Although participation in sport is encouraged as part of a healthy lifestyle, the sport-related injury burden is high.<ref>Emery CA, Pasanen K. [https://delfamdoc.org/wp-content/uploads/2019/11/current-trends-sports-injury-prevention.pdf Current trends in sport injury prevention.] Best Practice & Research Clinical Rheumatology. 2019 Feb 1;33(1):3-15.</ref> | ||
=== Consequences of Injuries in Sport === | === Consequences of Injuries in Sport === | ||
* Financial implications for the club | * Financial implications for the club<ref name=":4">Eliakim E, Morgulev E, Lidor R, Meckel Y. Estimation of injury costs: financial damage of English Premier League teams’ underachievement due to injuries. BMJ Open Sport & Exercise Medicine. 2020 May 1;6(1):e000675.</ref> | ||
** The cost of player injuries on sports leagues and organisations mainly fall into two categories: the direct medical costs and the opportunity cost of time loss injuries and shortened careers. This has led to professional teams offering players contracts contingent upon medical evaluations | ** The cost of player injuries on sports leagues and organisations mainly fall into two categories: the direct medical costs and the opportunity cost of time loss injuries and shortened careers. This has led to professional teams offering players contracts contingent upon medical evaluations - players with high injury risk may then be offered short-term contracts.<ref>Walia B, Boudreaux CJ. The cost of players’ injuries to professional sports leagues and other sports organizations. Managerial Finance. 2020 Jul 31.</ref> | ||
* Team performance | * Team performance<ref name=":4" /> | ||
** A significant relationship | ** A significant relationship between injury rates and time-loss with performance in elite team sports is reported.<ref>Hägglund M, Waldén M, Magnusson H, Kristenson K, Bengtsson H, Ekstrand J. [https://www.researchgate.net/publication/236639717_Injuries_affect_team_performance_negatively_in_professional_football_An_11-year_follow-up_of_the_UEFA_Champions_League_injury_study Injuries affect team performance negatively in professional football: an 11-year follow-up of the UEFA Champions League injury study]. British journal of sports medicine. 2013 Aug 1;47(12):738-42.</ref> | ||
* Financial implications for the healthcare system | * Financial implications for the healthcare system | ||
** Finch et al <ref name=":0">Finch CF, Kemp JL, Clapperton AJ. [https://www.sciencedirect.com/science/article/pii/S1063458415002095 The incidence and burden of hospital-treated sports-related injury in people aged 15+ years in Victoria, Australia, 2004–2010: a future epidemic of osteoarthritis?]. Osteoarthritis and cartilage. 2015 Jul 1;23(7):1138-43.</ref> investigated the trends and burdens of hospital-treated sports injuries in Australia and estimated the direct cost of sport-related injury over 7 years to be $265 million Australian dollars.<ref name=":0" /> | ** Finch et al<ref name=":0">Finch CF, Kemp JL, Clapperton AJ. [https://www.sciencedirect.com/science/article/pii/S1063458415002095 The incidence and burden of hospital-treated sports-related injury in people aged 15+ years in Victoria, Australia, 2004–2010: a future epidemic of osteoarthritis?]. Osteoarthritis and cartilage. 2015 Jul 1;23(7):1138-43.</ref> investigated the trends and burdens of hospital-treated sports injuries in Australia and estimated the direct cost of sport-related injury over 7 years to be $265 million Australian dollars.<ref name=":0" /> | ||
* Financial costs for the individual | * Financial costs for the individual | ||
** The inability to perform has significant impact on an athlete’s earnings. Secrist et al<ref>Secrist ES, Bhat SB, Dodson CC. [https://journals.sagepub.com/doi/full/10.1177/2325967116663921 The financial and professional impact of anterior cruciate ligament injuries in National Football League athletes.] Orthopaedic journal of sports medicine. 2016 Aug 30;4(8):2325967116663921.</ref> showed that players in the National Football League with an ACL injury earned on average $2,070,521 less than salary-matched controls over the 4 years after the injury. | ** The inability to perform has a significant impact on an athlete’s earnings. Secrist et al<ref>Secrist ES, Bhat SB, Dodson CC. [https://journals.sagepub.com/doi/full/10.1177/2325967116663921 The financial and professional impact of anterior cruciate ligament injuries in National Football League athletes.] Orthopaedic journal of sports medicine. 2016 Aug 30;4(8):2325967116663921.</ref> showed that players in the National Football League with an [[Anterior Cruciate Ligament (ACL) Reconstruction|ACL]] injury earned on average $2,070,521 less than salary-matched controls over the 4 years after the injury. | ||
* Implications for long term health | * Implications for long term health | ||
** It has been shown that knee injuries such as ACL or meniscal injury | ** It has been shown that knee injuries such as ACL or [[Meniscal Lesions|meniscal]] injury increase the odds of subsequently developing [[knee]] [[Osteoarthritis|OA]]<ref>Poulsen E, Goncalves GH, Bricca A, Roos EM, Thorlund JB, Juhl CB. Knee osteoarthritis risk is increased 4-6 fold after knee injury–a systematic review and meta-analysis. British journal of sports medicine. 2019 Dec 1;53(23):1454-63.</ref><ref>Snoeker B, Turkiewicz A, Magnusson K, Frobell R, Yu D, Peat G, Englund M. Risk of knee osteoarthritis after different types of knee injuries in young adults: a population-based cohort study. British journal of sports medicine. 2020 Jun 1;54(12):725-30.</ref> | ||
* Career progression in sports | * Career progression in sports | ||
** Larukain et al<ref name=":1">Larruskain J, Lekue JA, Martin-Garetxana I, Barrio I, McCall A, Gil SM. Injuries are negatively associated with player progression in an elite football academy. Science and Medicine in Football. 2021 Jun 16(just-accepted)</ref> demonstrated a negative association between injuries and player progression in an elite football academy with players that progressed to the next level having a lower injury burden and higher match availability compared to players that did not progress.<ref name=":1" /> | ** Larukain et al<ref name=":1">Larruskain J, Lekue JA, Martin-Garetxana I, Barrio I, McCall A, Gil SM. Injuries are negatively associated with player progression in an elite football academy. Science and Medicine in Football. 2021 Jun 16(just-accepted)</ref> demonstrated a negative association between injuries and player progression in an elite football academy with players that progressed to the next level having a lower injury burden and higher match availability compared to players that did not progress.<ref name=":1" /> | ||
Injury Prediction | === Injury Prediction === | ||
Can we predict injuries? In literature, there is the issue of prediction or association. Most of the available literature looks at retrospective studies where an association between a certain physical factor and an injury is seen, as opposed to using a certain physical factor in a retrospective manner to investigate if it can actually predict an injury.<ref>McCall A, Fanchini M, Coutts AJ. Prediction: the modern-day sport-science and sports-medicine “quest for the holy grail”. International journal of sports physiology and performance. 2017 May 1;12(5):704-6.</ref> | |||
Can we predict injuries? | |||
In recent years, much of the literature on screening tests suggests that these tests are not able to predict which athlete will sustain an injury, so clinicians are moving away from this idea.<ref>Bahr R. Why screening tests to predict injury do not work—and probably never will…: a critical review. British journal of sports medicine. 2016 Jul 1;50(13):776-80.</ref> However, this does not mean that screening should not be performed, as "screening remains essential in our efforts to protect athletes’ health."<ref>Verhagen E, van Dyk N, Clark N, Shrier I. Do not throw the baby out with the bathwater; screening can identify meaningful risk factors for sports injuries. British journal of sports medicine. 2018;52(19):1223-4.</ref> The following video provides a good explanation on injury risk and screening. | |||
{{#ev:youtube|lvP_KtQf3Xc|300}}<ref>Clinical Athlete. Injury risk and screening. Available from https://www.youtube.com/watch?v=lvP_KtQf3Xc [last accessed 25/8/2021]</ref> | |||
An infographic explaining prediction versus association in sports injuries can be found [https://ylmsportscience.com/2018/03/19/prediction-the-modern-day-sport-science-and-sports-medicine-quest-for-the-holy-grail/ here]. | |||
=== Factors Involved in the Development of Injuries === | |||
There are various factors that play a role in the risk of injury occurrence, and these factors can interact with each other:<ref name=":2">Herrington LC, Munro AG, Jones PA. Assessment of factors associated with injury risk. In: Performance Assessment in Strength and Conditioning 2018 Oct 9 (pp. 53-95). Routledge.</ref> | |||
* Training-related factors | |||
** Training volume, [[Load Management|load]], intensity | |||
** Type of training | |||
** Training and competition schedule | |||
** Rest | |||
* Motor control factors | |||
**[[Posture]] | |||
** [[Gait|Movement patterns]] | |||
** [[Muscle]] tone | |||
** Technique | |||
** Sport specific movements | |||
* Psychological factors<ref>Chang C, Putukian M, Aerni G, Diamond A, Hong G, Ingram Y, Reardon CL, Wolanin A. Mental health issues and psychological factors in athletes: detection, management, effect on performance and prevention: American Medical Society for Sports Medicine Position Statement—Executive Summary. British journal of sports medicine. 2020 Feb 1;54(4):216-20.</ref> | |||
** Beliefs | |||
** Fears | |||
** Coping strategies | |||
** Self-efficacy | |||
** Catastrophising | |||
** Emotional status ([[Stress and Health|stress]], [[depression]], anxiety) | |||
* Health-related factors | |||
** Diet | |||
** Medication | |||
** General health | |||
** Fatigue | |||
** [[Sleep: Regulation and Assessment|Sleep patterns]] | |||
* Non-modifiable factors | |||
** Gender | |||
** Age | |||
** Maturation stage | |||
** [[Body Composition|Body type]] | |||
** [[Genetic Conditions and Inheritance|Genetics]] | |||
** Previous injuries | |||
* Environmental factors | |||
** Training/competition surface | |||
** Equipment | |||
** Clothing | |||
** Weather | |||
** Coaching | |||
* Conditioning factors | |||
**[[Strength Training|Strength]] | |||
** [[Endurance Exercise|Endurance]] | |||
** [[Muscle Fibre Types|Muscle length]] | |||
**[[Range of Motion|Joint range of motion]] | |||
** Chronic capacity | |||
Social | * Additional demands | ||
** Home | |||
** Work | |||
** Family | |||
** Social | |||
** Leadership | |||
** Media | |||
** Sponsors | |||
* Other factors | |||
** Sport specific skill level | |||
** Ranking and status | |||
** Goals of athlete – short- and long-term | |||
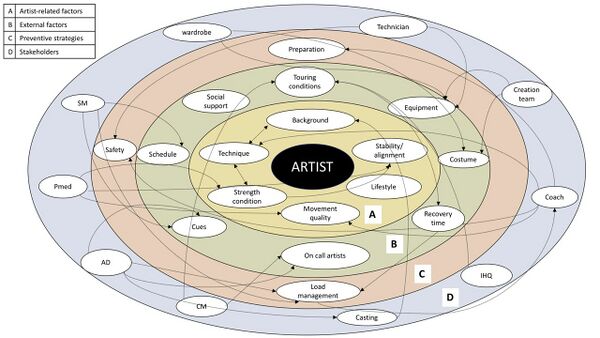
When considering injury screening, it is important to consider the myriad of factors that can influence injury occurrence. Furthermore, it is unlikely that these can be reduced to a single factor that may lead to injury.<ref name=":2" /> Factors that are commonly screened for in musculoskeletal injury risk screening are: | |||
* Strength and conditioning | |||
* Movement quality | |||
* Stability/alignment | |||
From the map by Bolling et al<ref name=":3">Bolling C, Mellette J, Pasman HR, Van Mechelen W, Verhagen E. [https://bmjopensem.bmj.com/content/5/1/e000492 From the safety net to the injury prevention web: applying systems thinking to unravel injury prevention challenges and opportunities in Cirque du Soleil.] BMJ open sport & exercise medicine. 2019 Feb 1;5(1):e000492.</ref> it is evident that these factors are just a few of the many factors that can be involved in injury occurrence.<ref name=":3" />Athlete-related factors can also include background, technique, lifestyle.<ref name=":3" /> External factors can include: recovery time, equipment, social support, schedules.<ref name=":3" /> Preventative strategies can include: preparation and load management.<ref name=":3" /> See the map below for more detail and read the complete article: [https://bmjopensem.bmj.com/content/5/1/e000492 From the safety net to the injury prevention web: applying systems thinking to unravel injury prevention challenges and opportunities in Cirque du Soleil.]<ref name=":3" /> | |||
[[File:Bolling injury prevention.jpg|center|A multilevel system map with factors, strategies and stakeholders in relation to injury and its prevention. Starting at the centre of the map (ie, the athlete) and moving outwards; (A) entails artist-related intrinsic injury factors; (B) presents external injury factors; (C) describes the main preventive strategies (eg, load management, safety and preparation) which are driven by the factors from the inner two circles; (D) represents the stakeholders in the system as well as how they connect to the strategies and factors across the multiple levels.<ref name=":3" />|alt=|thumb|600x600px]] | |||
== Predisposition to Injuries == | |||
Instead of trying to predict injury occurrence, it may be more appropriate to identify athletes who are predisposed and where possible modify the predisposition. | Instead of trying to predict injury occurrence, it may be more appropriate to identify athletes who are predisposed and where possible modify the predisposition. | ||
Non-modifiable predispositions | * Non-modifiable predispositions include: | ||
** Anatomy | |||
** Genetics | |||
** Previous injury | |||
** Environmental factors | |||
* Modifiable predispositions include: | |||
** Strength | |||
** Movement | |||
** Skill | |||
** Flexibility | |||
** State of the athlete e.g. tired or stressed? | |||
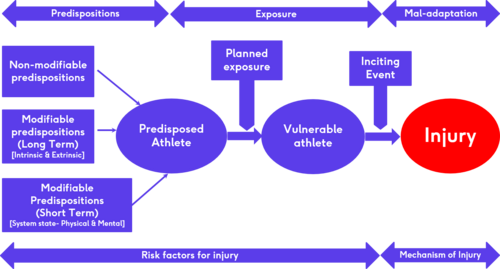
This flow diagram created by Dr Lee Herrington illustrates how predispositions and exposure to load can lead to vulnerability in an athlete and, in combination with an inciting event, can lead to injury mechanisms and occurrences. | |||
[[File:Injury predisposition flow diagram.png|center|thumb|Injury predisposition|alt=|500x500px]] | |||
=== Considerations in Identifying Predisposed Athletes === | |||
* Understand the nature of the sport and the injuries occurring | |||
** Common injuries vs catastrophic injuries (for example hamstring injuries vs ACL injuries soccer) | |||
* Identify which injury needs to be targeted as this will determine what type of screening tests will be used | |||
* Do these specific injuries have modifiable factors? | |||
* Are there clearly definable physical qualities related to the injury? Can these modifiable factors be clearly defined in terms of certain physical qualities? | |||
* Can these physical qualities be identified with reliable screening tests? | |||
* Can these physical qualities be influenced, modified or changed? (For example – blue eyes may be a predisposing factor to a certain type of injury and can easily and reliably be screened for, but eye colour cannot be changed, modified or influenced.) | |||
* Traumatic injuries in the sport – how influenceable are traumatic injuries through screening and training? | |||
=== Screening for Neuromuscular Control of Movement === | |||
[[Neuromuscular Exercise Program|Neuromuscular]] control is the ability to perform a movement in the best possible way to minimise loading stress or maximise the distribution of loading stresses on the tissue involved.<ref name=":2" /> An important part of “movement screening” is to identify the high-risk movement tasks and determine if these tasks can be broken down into closed skills. A closed skill is undertaken in a controlled environment where the athlete only focuses on that specific skill (e.g. [[Single Leg Squat Test|single leg squat]] or single-leg landing).<ref name=":2" /> An open skill is undertaken in a very chaotic and random environment (e.g. single-leg landing in the middle of a sporting environment such as competition or match). The context in which these movements take pace will have an influence on performance, as well as the risk for injury. For example, an athlete may pass a closed skill test/task such as single-leg landing at the pre-season screening, but still get injured (i.e. ACL injury) as a result of a single-leg landing in a sporting environment such as a competition. | |||
==== Selecting a Screening Test/Task ==== | |||
Factors to consider when selecting a screening test or task include:<ref name=":2" /> | |||
* Nature of activities undertaken in the specific sport | |||
* Nature of the major injuries in the specific sport (are these linked to specific movements or activities?) | |||
* Athlete’s injury history (can previous injuries be linked to specific movements or activities?) | |||
==== Factors Influencing Neuromuscular Control of Movement ==== | |||
Various factors can have an impact on an athlete's ability to perform a specific screening test or task. These include:<ref name=":2" /> | |||
* [[Strength-Duration Curve|Strength]] | |||
* Joint range of motion | |||
* [[Stretching|Muscle length]] – [[flexibility]] | |||
* [[Proprioception]] – joint position sense | |||
* Movement dissociation | |||
* Sport specific [[Motor Control and Learning|skill]] | |||
=== Building a Paradigm for Injury Risk Screening === | |||
* Consider predisposition versus prediction of injuries | |||
** Screening tests cannot predict if an athlete will get injured, but we can screen and look for predisposed athletes. Remember that being predisposed to a certain injury does not mean that an athlete will get injured. Also, if an athlete does not have a predisposition to an injury, this is not a guarantee that the athlete will not be injured. Athletes become vulnerable to injury when they are exposed to load and inciting events (see flow diagram above). | |||
* Identify if force generation, force absorption or movement skill are an issue in predisposition | |||
* Identify the predisposing movement task/s | |||
* Break down the identified movement task into closed skills that can be measured reliably | |||
* If the athlete fails the test/task, identify the reasons for failure | |||
* Build ways to improve the skill in a controlled environment, but then also in training and competition environments | |||
=== Examples of Screening Tests === | |||
* Lower quadrant tests | |||
** [[Single Leg Squat Test|Single-leg squat]] | |||
** [https://journals.humankinetics.com/view/journals/jsr/30/8/article-p1242.xml Single-leg landing] | |||
** [http://mars.s2p.si/e_files/content/Drop%20Jump.pdf Drop jump Test] | |||
** [[Star Excursion Balance Test]] | |||
** [[Hop Test|Hop for distance tests]] | |||
* Upper quadrant tests | |||
** [[Glenohumeral Joint|Glenohumeral Internal Rotation Deficit (GIRD)]] | |||
** Closed chain upper limb test | |||
* [[Functional Movement Screen (FMS)]] | |||
* [http://s3.amazonaws.com/ustaassets/assets/1/15/11940_highperformance_profile_lowres.pdf United States Tennis Association High Performance Profile] | |||
* [https://www.researchgate.net/publication/311426830_The_nine_test_screening_battery_-_Normative_values_on_a_group_of_recreational_athletes Nine Test Screening Battery]<ref>Flodström F, Heijne A, Batt ME, Frohm A. The nine test screening battery-normative values on a group of recreational athletes. International journal of sports physical therapy. 2016 Dec;11(6):936.</ref> | |||
* [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4275191/ Athletic Ability Assessment]<ref>McKeown I, Taylor‐McKeown K, Woods C, Ball N. Athletic ability assessment: a movement assessment protocol for athletes. International journal of sports physical therapy. 2014 Dec;9(7):862.</ref> | |||
* [https://www.springboks.rugby/general/boksmart-medical-protocol-screening-of-players/ Boksmart pre-participation screening of players] | |||
** This website has various documents that can be downloaded such as the musculoskeletal assessment form and protocol as well as various other assessment documents. | |||
== Resources == | == Resources == | ||
# | * [[Risk Factors and Injury Mechanisms in Sports Injuries|Risk factors and injury mechanisms in sports injuries]] | ||
# | * Rod Whiteley, Sports Physiotherapist. Aspetar. [https://www.facebook.com/SASportsMedicineAssociation/videos/1576806859165507/ If screening is a waste of time as Roald Bahr tells us, why should you still be doing it?] | ||
* Below are two videos you can watch on injury risk screening | |||
<div class="row"> | |||
<div class="col-md-6"> {{#ev:youtube|y0HroNZWmT8|250}} <div class="text-right"><ref>Aspetar. Why screening to predict injury doesn’t work and probably never will. Available from https://www.youtube.com/watch?v=y0HroNZWmT8 [last accessed 19/5/2022]</ref></div></div> | |||
<div class="col-md-6"> {{#ev:youtube|v=jXWWc3wML3o&t=3s|250}} <div class="text-right"><ref>Aspetar. From athlete screening to injury risk management -Prof Roald Bahr. Available from https://www.youtube.com/watch?v=jXWWc3wML3o&t=3s [last accessed 19/5/2022]</ref></div></div> | |||
</div> | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Course Pages]] | |||
[[Category:Plus Content]] | |||
[[Category:Sports Medicine]] | |||
[[Category:Sports Screening Tests]] | |||
Latest revision as of 12:18, 20 November 2023
Top Contributors - Wanda van Niekerk, Jess Bell, Kim Jackson, Tarina van der Stockt, Uchechukwu Chukwuemeka and Lucinda hampton
Introduction[edit | edit source]
Screening is a valuable process for athletes and is commonly practised in several elite sports. One of the common elements of a periodic medical assessment of athletes, is the musculoskeletal screening or examination. For many years, physiotherapists have screened athletes with the aim of identifying the athletes at risk for injury, so that they can then implement injury prevention programmes for these athletes. More recently, the focus has, however, shifted from using screening to predict injuries to rather using screening to identify possible predispositions to injury.
Reasons for the Periodic Medical Assessment of Athletes[edit | edit source]
The main reason for the periodic medical assessment of athletes is to safeguard sports participation, but there are many other additional benefits, including:[1][2]
- Identification of medical conditions that contraindicate sports participation
- Assessment of known injuries and illnesses
- Review of current medications and supplements
- Athlete education
- Baseline testing
- Developing rapport with the athlete
- Specific screening
- Cardiac screening
- Screening for unknown illnesses
- Screening for risk factors for future injury
Read more: Screening in sport and Pre-participation Screening
Why Screen for Injury Risk?[edit | edit source]
Injury rates in sports are increasing despite the increased professionalism of sports science and the use of sports medicine support teams. Although participation in sport is encouraged as part of a healthy lifestyle, the sport-related injury burden is high.[3]
Consequences of Injuries in Sport[edit | edit source]
- Financial implications for the club[4]
- The cost of player injuries on sports leagues and organisations mainly fall into two categories: the direct medical costs and the opportunity cost of time loss injuries and shortened careers. This has led to professional teams offering players contracts contingent upon medical evaluations - players with high injury risk may then be offered short-term contracts.[5]
- Team performance[4]
- A significant relationship between injury rates and time-loss with performance in elite team sports is reported.[6]
- Financial implications for the healthcare system
- Financial costs for the individual
- Implications for long term health
- Career progression in sports
Injury Prediction[edit | edit source]
Can we predict injuries? In literature, there is the issue of prediction or association. Most of the available literature looks at retrospective studies where an association between a certain physical factor and an injury is seen, as opposed to using a certain physical factor in a retrospective manner to investigate if it can actually predict an injury.[12]
In recent years, much of the literature on screening tests suggests that these tests are not able to predict which athlete will sustain an injury, so clinicians are moving away from this idea.[13] However, this does not mean that screening should not be performed, as "screening remains essential in our efforts to protect athletes’ health."[14] The following video provides a good explanation on injury risk and screening.
An infographic explaining prediction versus association in sports injuries can be found here.
Factors Involved in the Development of Injuries[edit | edit source]
There are various factors that play a role in the risk of injury occurrence, and these factors can interact with each other:[16]
- Training-related factors
- Training volume, load, intensity
- Type of training
- Training and competition schedule
- Rest
- Motor control factors
- Posture
- Movement patterns
- Muscle tone
- Technique
- Sport specific movements
- Psychological factors[17]
- Beliefs
- Fears
- Coping strategies
- Self-efficacy
- Catastrophising
- Emotional status (stress, depression, anxiety)
- Health-related factors
- Diet
- Medication
- General health
- Fatigue
- Sleep patterns
- Environmental factors
- Training/competition surface
- Equipment
- Clothing
- Weather
- Coaching
- Conditioning factors
- Strength
- Endurance
- Muscle length
- Joint range of motion
- Chronic capacity
- Additional demands
- Home
- Work
- Family
- Social
- Leadership
- Media
- Sponsors
- Other factors
- Sport specific skill level
- Ranking and status
- Goals of athlete – short- and long-term
When considering injury screening, it is important to consider the myriad of factors that can influence injury occurrence. Furthermore, it is unlikely that these can be reduced to a single factor that may lead to injury.[16] Factors that are commonly screened for in musculoskeletal injury risk screening are:
- Strength and conditioning
- Movement quality
- Stability/alignment
From the map by Bolling et al[18] it is evident that these factors are just a few of the many factors that can be involved in injury occurrence.[18]Athlete-related factors can also include background, technique, lifestyle.[18] External factors can include: recovery time, equipment, social support, schedules.[18] Preventative strategies can include: preparation and load management.[18] See the map below for more detail and read the complete article: From the safety net to the injury prevention web: applying systems thinking to unravel injury prevention challenges and opportunities in Cirque du Soleil.[18]
Predisposition to Injuries[edit | edit source]
Instead of trying to predict injury occurrence, it may be more appropriate to identify athletes who are predisposed and where possible modify the predisposition.
- Non-modifiable predispositions include:
- Anatomy
- Genetics
- Previous injury
- Environmental factors
- Modifiable predispositions include:
- Strength
- Movement
- Skill
- Flexibility
- State of the athlete e.g. tired or stressed?
This flow diagram created by Dr Lee Herrington illustrates how predispositions and exposure to load can lead to vulnerability in an athlete and, in combination with an inciting event, can lead to injury mechanisms and occurrences.
Considerations in Identifying Predisposed Athletes[edit | edit source]
- Understand the nature of the sport and the injuries occurring
- Common injuries vs catastrophic injuries (for example hamstring injuries vs ACL injuries soccer)
- Identify which injury needs to be targeted as this will determine what type of screening tests will be used
- Do these specific injuries have modifiable factors?
- Are there clearly definable physical qualities related to the injury? Can these modifiable factors be clearly defined in terms of certain physical qualities?
- Can these physical qualities be identified with reliable screening tests?
- Can these physical qualities be influenced, modified or changed? (For example – blue eyes may be a predisposing factor to a certain type of injury and can easily and reliably be screened for, but eye colour cannot be changed, modified or influenced.)
- Traumatic injuries in the sport – how influenceable are traumatic injuries through screening and training?
Screening for Neuromuscular Control of Movement[edit | edit source]
Neuromuscular control is the ability to perform a movement in the best possible way to minimise loading stress or maximise the distribution of loading stresses on the tissue involved.[16] An important part of “movement screening” is to identify the high-risk movement tasks and determine if these tasks can be broken down into closed skills. A closed skill is undertaken in a controlled environment where the athlete only focuses on that specific skill (e.g. single leg squat or single-leg landing).[16] An open skill is undertaken in a very chaotic and random environment (e.g. single-leg landing in the middle of a sporting environment such as competition or match). The context in which these movements take pace will have an influence on performance, as well as the risk for injury. For example, an athlete may pass a closed skill test/task such as single-leg landing at the pre-season screening, but still get injured (i.e. ACL injury) as a result of a single-leg landing in a sporting environment such as a competition.
Selecting a Screening Test/Task[edit | edit source]
Factors to consider when selecting a screening test or task include:[16]
- Nature of activities undertaken in the specific sport
- Nature of the major injuries in the specific sport (are these linked to specific movements or activities?)
- Athlete’s injury history (can previous injuries be linked to specific movements or activities?)
Factors Influencing Neuromuscular Control of Movement[edit | edit source]
Various factors can have an impact on an athlete's ability to perform a specific screening test or task. These include:[16]
- Strength
- Joint range of motion
- Muscle length – flexibility
- Proprioception – joint position sense
- Movement dissociation
- Sport specific skill
Building a Paradigm for Injury Risk Screening[edit | edit source]
- Consider predisposition versus prediction of injuries
- Screening tests cannot predict if an athlete will get injured, but we can screen and look for predisposed athletes. Remember that being predisposed to a certain injury does not mean that an athlete will get injured. Also, if an athlete does not have a predisposition to an injury, this is not a guarantee that the athlete will not be injured. Athletes become vulnerable to injury when they are exposed to load and inciting events (see flow diagram above).
- Identify if force generation, force absorption or movement skill are an issue in predisposition
- Identify the predisposing movement task/s
- Break down the identified movement task into closed skills that can be measured reliably
- If the athlete fails the test/task, identify the reasons for failure
- Build ways to improve the skill in a controlled environment, but then also in training and competition environments
Examples of Screening Tests[edit | edit source]
- Lower quadrant tests
- Upper quadrant tests
- Glenohumeral Internal Rotation Deficit (GIRD)
- Closed chain upper limb test
- Functional Movement Screen (FMS)
- United States Tennis Association High Performance Profile
- Nine Test Screening Battery[19]
- Athletic Ability Assessment[20]
- Boksmart pre-participation screening of players
- This website has various documents that can be downloaded such as the musculoskeletal assessment form and protocol as well as various other assessment documents.
Resources[edit | edit source]
- Risk factors and injury mechanisms in sports injuries
- Rod Whiteley, Sports Physiotherapist. Aspetar. If screening is a waste of time as Roald Bahr tells us, why should you still be doing it?
- Below are two videos you can watch on injury risk screening
References[edit | edit source]
- ↑ Targett S, Clarsen B. Periodic medical assessment of athletes. In: Brukner P, Clarsen B, Cook J, Cools A, Crossley K, Hutchinson M, McCroy P, Bahr R, Khan K. Brukner and Khan's Clinical Sports Medicine: Injuries, Volume 1, 5e. Sydney: McGraw Hill Education. 2017
- ↑ Nabhan D, Taylor D, Lewis M, Bahr R. Protecting the world’s finest athletes: periodic health evaluation practices of the top performing National Olympic Committees from the 2016 Rio or 2018 PyeongChang Olympic Games. British Journal of Sports Medicine. 2021 Sep 1;55(17):961-7.
- ↑ Emery CA, Pasanen K. Current trends in sport injury prevention. Best Practice & Research Clinical Rheumatology. 2019 Feb 1;33(1):3-15.
- ↑ 4.0 4.1 Eliakim E, Morgulev E, Lidor R, Meckel Y. Estimation of injury costs: financial damage of English Premier League teams’ underachievement due to injuries. BMJ Open Sport & Exercise Medicine. 2020 May 1;6(1):e000675.
- ↑ Walia B, Boudreaux CJ. The cost of players’ injuries to professional sports leagues and other sports organizations. Managerial Finance. 2020 Jul 31.
- ↑ Hägglund M, Waldén M, Magnusson H, Kristenson K, Bengtsson H, Ekstrand J. Injuries affect team performance negatively in professional football: an 11-year follow-up of the UEFA Champions League injury study. British journal of sports medicine. 2013 Aug 1;47(12):738-42.
- ↑ 7.0 7.1 Finch CF, Kemp JL, Clapperton AJ. The incidence and burden of hospital-treated sports-related injury in people aged 15+ years in Victoria, Australia, 2004–2010: a future epidemic of osteoarthritis?. Osteoarthritis and cartilage. 2015 Jul 1;23(7):1138-43.
- ↑ Secrist ES, Bhat SB, Dodson CC. The financial and professional impact of anterior cruciate ligament injuries in National Football League athletes. Orthopaedic journal of sports medicine. 2016 Aug 30;4(8):2325967116663921.
- ↑ Poulsen E, Goncalves GH, Bricca A, Roos EM, Thorlund JB, Juhl CB. Knee osteoarthritis risk is increased 4-6 fold after knee injury–a systematic review and meta-analysis. British journal of sports medicine. 2019 Dec 1;53(23):1454-63.
- ↑ Snoeker B, Turkiewicz A, Magnusson K, Frobell R, Yu D, Peat G, Englund M. Risk of knee osteoarthritis after different types of knee injuries in young adults: a population-based cohort study. British journal of sports medicine. 2020 Jun 1;54(12):725-30.
- ↑ 11.0 11.1 Larruskain J, Lekue JA, Martin-Garetxana I, Barrio I, McCall A, Gil SM. Injuries are negatively associated with player progression in an elite football academy. Science and Medicine in Football. 2021 Jun 16(just-accepted)
- ↑ McCall A, Fanchini M, Coutts AJ. Prediction: the modern-day sport-science and sports-medicine “quest for the holy grail”. International journal of sports physiology and performance. 2017 May 1;12(5):704-6.
- ↑ Bahr R. Why screening tests to predict injury do not work—and probably never will…: a critical review. British journal of sports medicine. 2016 Jul 1;50(13):776-80.
- ↑ Verhagen E, van Dyk N, Clark N, Shrier I. Do not throw the baby out with the bathwater; screening can identify meaningful risk factors for sports injuries. British journal of sports medicine. 2018;52(19):1223-4.
- ↑ Clinical Athlete. Injury risk and screening. Available from https://www.youtube.com/watch?v=lvP_KtQf3Xc [last accessed 25/8/2021]
- ↑ 16.0 16.1 16.2 16.3 16.4 16.5 Herrington LC, Munro AG, Jones PA. Assessment of factors associated with injury risk. In: Performance Assessment in Strength and Conditioning 2018 Oct 9 (pp. 53-95). Routledge.
- ↑ Chang C, Putukian M, Aerni G, Diamond A, Hong G, Ingram Y, Reardon CL, Wolanin A. Mental health issues and psychological factors in athletes: detection, management, effect on performance and prevention: American Medical Society for Sports Medicine Position Statement—Executive Summary. British journal of sports medicine. 2020 Feb 1;54(4):216-20.
- ↑ 18.0 18.1 18.2 18.3 18.4 18.5 18.6 Bolling C, Mellette J, Pasman HR, Van Mechelen W, Verhagen E. From the safety net to the injury prevention web: applying systems thinking to unravel injury prevention challenges and opportunities in Cirque du Soleil. BMJ open sport & exercise medicine. 2019 Feb 1;5(1):e000492.
- ↑ Flodström F, Heijne A, Batt ME, Frohm A. The nine test screening battery-normative values on a group of recreational athletes. International journal of sports physical therapy. 2016 Dec;11(6):936.
- ↑ McKeown I, Taylor‐McKeown K, Woods C, Ball N. Athletic ability assessment: a movement assessment protocol for athletes. International journal of sports physical therapy. 2014 Dec;9(7):862.
- ↑ Aspetar. Why screening to predict injury doesn’t work and probably never will. Available from https://www.youtube.com/watch?v=y0HroNZWmT8 [last accessed 19/5/2022]
- ↑ Aspetar. From athlete screening to injury risk management -Prof Roald Bahr. Available from https://www.youtube.com/watch?v=jXWWc3wML3o&t=3s [last accessed 19/5/2022]