Multidisciplinary and Interdisciplinary Management of the Amputee: Difference between revisions
| Line 125: | Line 125: | ||
== Resources == | == Resources == | ||
[https://www.sahealth.sa.gov.au/wps/wcm/connect/7b1770804b32fa9e8708afe79043faf0/Amputee+Rehabilitation+Model+of+Care.pdf?MOD=AJPERES&CACHEID=7b1770804b32fa9e8708afe79043faf0 Model of Amputee Rehabilitation in South Australia]. Government of South Australia, Statewide Rehabilitation Clinical Network. 2012 | |||
[http://www.healthquality.va.gov/amputation/amp_sum_508.pdf Clinical Practice Guideline for Rehabilitation of Lower Limb Amputation]. Department of Veterans Affairs, Department of Defense. 2007 | |||
== References == | == References == | ||
Revision as of 16:16, 11 March 2015
Original Editor - Caroline Cater as part of the WCPT Network for Amputee Rehabilitation Project
Top Contributors - Admin, Aicha Benyaich, Sheik Abdul Khadir, Tony Lowe, Richard Benes, Tarina van der Stockt, Kim Jackson, 127.0.0.1, Lauren Lopez, Rachael Lowe, Simisola Ajeyalemi, Amrita Patro and Jess Bell
Introduction[edit | edit source]
To provide an effective and efficient service the team work together towards goals agreed with the patient. The physiotherapist plays a key role in coordinating patient rehabilitation.
Multi-disciplinary approach (MDT)[edit | edit source]
A specialist MDT achieves the best prosthetic outcomes.
- Professionals working parallel with clear roles.
- Each professional sets their own individual goals with the patients and communicates these goals and outcomes with the rest of the team where appropriate.
- Lead by Consultant or team leader.
- Little overlap between disciplines.
The MDT is recognized internationally as the amputee rehabilitation model of choice, although there is little published literature to support this (BACPAR, 2006).
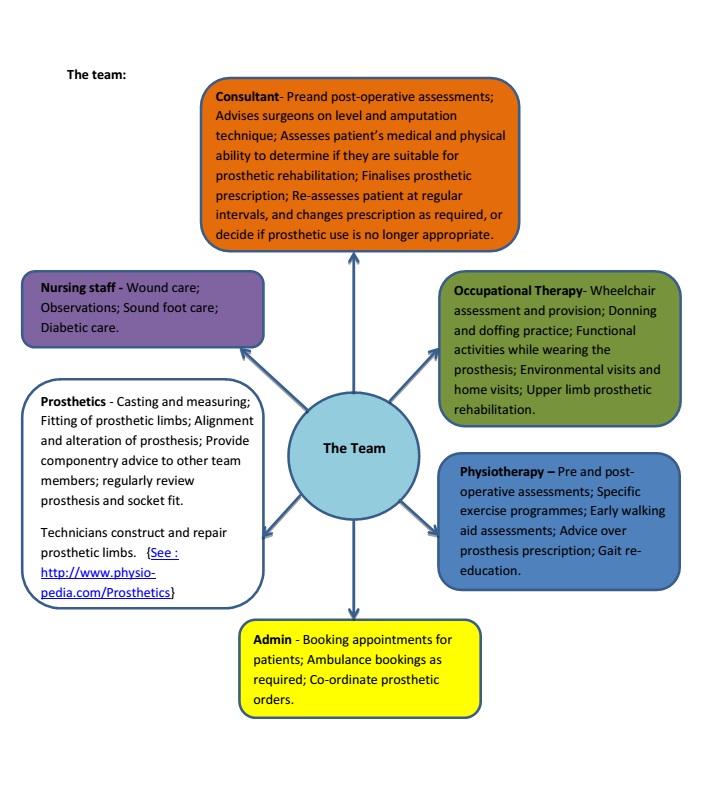
For amputee rehabilitation the core MDT may include: physiotherapist, occupational therapist, prosthetist, rehabilitation doctor, counsellor and nurse.
Inter disciplinary approach (IDT) [1][edit | edit source]
- Professionals involved in joint problem solving, working beyond their own scope of practice.
- Treatment goals overlap and collaborate with other disciplines.
- Regular communication between team members.
Evidence based clinical guidelines set in 2012 by BACPAR [2] stated:
The IDT approach has started to become more prominent in a few areas of the NHS.This style aims to achieve the optimum outcome for the patients by all professionals working towards the same goals, and working together with other disciplines to problem solve and provide treatment. Korner 2009, compares these two style of working, MDT versus IDT, with a clear outline of how the two approaches differ.Within amputee rehabilitation many limb centres are starting to adopt the IDT approach. As communication between prosthetists, physiotherapists, doctors and other healthcare professionals improve,the team is able to work together more closely and achieve better outcomes.
The Team[edit | edit source]
“Care for patients with an amputation traumatic and non-traumatic is complex and requires from multiple medical, surgical and rehabilitation specialties in order to:
- Develop a patient centred treatment plan that includes comprehensive knowledge and best practice for each discipline
- Reduce the risk of missing potential complications factors that may negatively influence operative and rehabilitation outcomes
- Enhance patient and family education”
“The composition of the team at each phase within the amputee service must be appropriate to the types of service being provided and the needs of the amputee. The patient is to remain at the centre of all decision making and be an integral member of the team that is providing the care. “ The rehabilitation process should have an educational element that empowers patients and carers to take an active role in their present and future management.
The rehabilitation treatment plan is utilized to guide the care of a patient who has undergone an amputation throughout the entire course of rehabilitation. the treatment plan is based on evaluation by all specialties involved in the rehabilitation process, and acts as a guide for all team members to address goals important to the patient and family. the level of rehabilitation intervention is contemplated from the date of admission to the hospital and determined after the amputation surgery and prior to discharge from the hospital. the rehabilitative process includes:
- Ongoing medical assessment of impairments
- Therapy interventions to address disabilities or activity limitation
| Patient Journey | The team management | Physiotherapy management | |
|---|---|---|---|
| 1. | Pre-amputation | Subjective assessment - History of present condition; Past medical history; Drug history; Social History. Objective assessment - Range of movement (ROM); Muscle power; Limb for amputation; Pulses; Skin integrity. Collaborating all findings to decide on most appropriate level of amputation for the individual and, if they are likely to become a limb wearer, which level of amputation would be most appropriate. |
Focus is on the objective assessment looking at ROM and muscle power. Using assessment findings, knowledge of prosthetic componentry and gait patterns, provide a clinically reasoned recommended level of amputation to the consultant. Provide patient with appropriate exercises to aid post-amputation mobility. |
| 2. | Immediately post-amputation | Medical care; Wound care; Discharge planning. |
Transfer practice, and specific exercises to improve strength; increase exercise tolerance; maintain ROM. |
| 3. | Pre-prosthetic rehabilitation | Monitoring patient progress; counselling if required; Patient goals; deciding on prosthetic prescription with whole team and all appropriate information (including how the patient has managed with EWA and patient goals) | Early walking aids(EWA) assessment:
Using EWA to help decide on a patient’s suitability for a prosthetic limb, and liaising with whole team regardPre-fitting management of the amputee |
| 4. | Casting and measuring |
Prosthetists cast and measure a patient’s residuum. |
Physiotherapist may be needed to assist in the cast appointment, to ensure a neutral alignment of the pelvis is obtained. |
| 5. | Fitting of prosthesis |
Prosthetists fit the primary prosthesis to the patient, ensuring the alignment and length are correct in a standing and walking. Prosthetics |
Physiotherapy input is beneficial at this point, to help with mobility, alignment and length. |
| 6. | Gait Re-education | Prosthetists will help problem solve and adjust prosthesis as required. | The physiotherapist takes a lead role at this stage. Beginning with educating the patient about donning and doffing the prosthesis, skin integrity and weight bearing areas on their residuum. A gait rehabilitation programme can then commence. Gait in prosthetic rehabilitation |
| 7. | Review | Patient will be reviewed regularly by the consultant and prosthetic team.Assessing the individual is still suitable for prosthetic use, the prosthetic prescription is still the most appropriate option for the patient and any required changes are made to the prosthesis as the patient changes. | The consultant and/or prosthetist may ask for physiotherapy input. For example if the patient is having a change of prescription, their goals have changed, their mobility has decreased/increased. The physiotherapist may be required to re-commence a gait rehabilitation programme with the patient or advice only may be required. |
Mechanisms and importance of communication systems between services
[edit | edit source]
Communication within the IDT is critical and should regularly occur to ensure that the members of the team are informed and aware of a patient’s progress. This is most commonly achieved by a goal setting meeting.This may be held fortnightly or monthly depending on the limb centre and their service. This meeting allows the team to discuss patient goals (which have been clearly defined in the outcome measure COPM) enabling the team to decide on patient focused SMART goals.
Additionally the regular meeting ensures that all team members are aware and up to date with patient progress and any issues or concerns can be discussed with a joint approach to problem solving.
Alternatively an email system may be set up, which can be particularly useful for satellite clinics at different hospital sites. This can be set up as a generic email within the nhs mail system, and works well if all team members are check it regularly and respond in a timely manner.
Telephone contact is also a very useful option to connect members of staff at different sites, and again is particularly useful for team members at satellite clinics to liaise and problem solve with the wider team.
Resources[edit | edit source]
Model of Amputee Rehabilitation in South Australia. Government of South Australia, Statewide Rehabilitation Clinical Network. 2012
Clinical Practice Guideline for Rehabilitation of Lower Limb Amputation. Department of Veterans Affairs, Department of Defense. 2007
References[edit | edit source]
- ↑ Körner, M. (2010) Interprofessional teamwork in medical rehabilition: a comparison of multidisciplinary and interdisciplinary team approach, Clinical Rehabilitation, 24 (8)745-755
- ↑ Broomhead, P., Clark, K., Dawes, D., Hale, C., Lambert, A., Quinlivan, D., Randell, T., Shepherd, R., Withpetersen, J. (2012) Evidence Based Clinical Guidelines for the Managements of Adults with Lower Limb Prostheses, 2nd Edition,Chartered Society of Physiotherapy: London