McArdle's Disease: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) (Removed copyright violation image) |
||
| (129 intermediate revisions by 7 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox">'''Original Editors '''- [[User:Edward Foring|Ed Foring]] as part of [[Pathophysiology of Complex Patient Problems|Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | |||
'''Original Editors '''- [[User:Edward Foring|Ed Foring]] as part of [[Pathophysiology of Complex Patient Problems|Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Definition/Description< | == Definition/Description == | ||
[[File:Chromosome-DNA-gene copy.jpg|right|frameless]] | |||
McArdle disease is a [[Genetic Conditions and Inheritance|genetic disorder]] that mainly affects [[Muscle Cells (Myocyte)|skeletal muscles]]. It occurs due to the deficiency or absence of an [[Enzymes|enzyme]] called myophosphorylase, a key substance that the [[Muscle|muscles]] need to break down [[glycogen]] into sugar (glucose) for energy. Symptoms include painful [[Exercise-Associated Muscle Cramps|muscle cramps]], weakness, and fatigue manifested during periods of [[Physical Activity|physical activity]].<ref name=":0">Khattak ZE, Ashraf M. [https://www.statpearls.com/articlelibrary/viewarticle/24796/ McArdle Disease.] StatPearls [Internet]. 2020 Aug 15. Available:https://www.statpearls.com/articlelibrary/viewarticle/24796/ (accessed 23.10.2021)</ref> The disease can lead to dark [[urine]]. | |||
* Severe, uncontrolled McArdle disease can cause life-threatening [[kidney]] problems.<ref name=":1">Cedars Sinai [https://www.cedars-sinai.org/health-library/diseases-and-conditions/m/mcardle-disease.html McArdle Disease] Available: https://www.cedars-sinai.org/health-library/diseases-and-conditions/m/mcardle-disease.html (accessed 23.10.2021)</ref> | |||
* To avoid the unpleasant symptoms associated with this condition and improve the [[Quality of Life|quality of life]], the disease requires prompt diagnosis and treatment.<ref name=":0" /> | |||
== Etiology == | |||
McArdle disease typically results from mutations involving the muscle-specific isoform of the glycogen phosphorylase enzyme. This enzyme plays a key role in the first step of [[Glycolysis|glycogenolysis]] that release glucose-1-phosphate monomers in muscle fibers. As a result, [[Carbohydrates|carbohydrate]] metabolism of the skeletal-muscle is affected, and energy cannot be generated from the glycogen stores of muscles. | |||
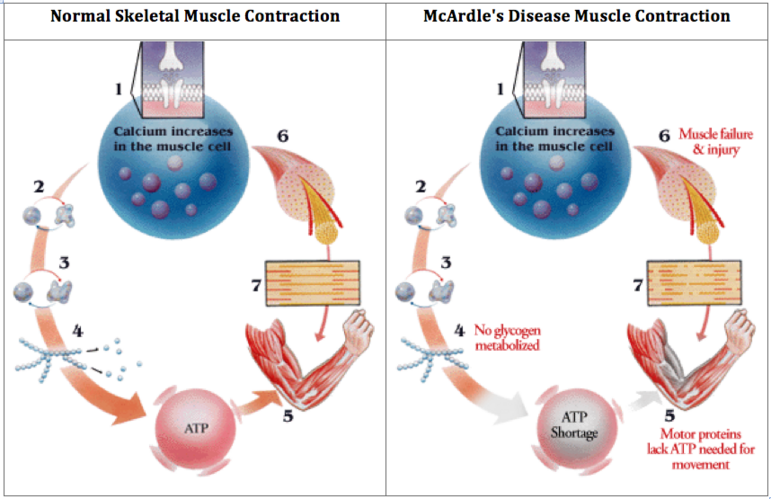
<br> | Image 2:How muscle contraction differs in an unaffected muscle compared to one with McArdle’s Disease.<br> | ||
[[Image:Screen Shot 2017-04-04 at 10.14.25 PM.png|center|771x771px|alt=]]<ref name="p1">MedPoster 1992. nobelprize.org. [cited 3 April 2011]. Available from: http://nobelprize.org/nobel_prizes/medicine/laureates/1992/illpres/glycogen.html</ref><ref name="p2">McArdlesDisease.org. [cited 17 March 2011]. Available from: www.mcardledisease.org</ref> | |||
< | == Epidemiology == | ||
The exact prevalence of McArdle disease is not precisely known and appears to range from 1 in 50,000 to 1 in 200,000 in the United States. <ref name=":0" /> | |||
== Characteristics/Clinical Presentation == | |||
McArdle Disease patients can have critical episodes of early fatigue when exercising, muscle pain (myalgia), myoglobinuria (when muscles break down and release myoglobin in urine, making it brown/red in colour), and then subsequent kidney failure<ref name=":2">Brain Foundation McArdle Disease Award - 2012 Available: https://brainfoundation.org.au/research-grants/2012/mcardle-disease-award/ (accessed 23.10.2021)</ref>. Some common symptoms of McArdle disease are: | |||
* Better able to do aerobic exercise after 8 to 10 minutes (second-wind phenomenon) | |||
* Brownish red urine, especially after periods of activity | |||
* Easily tiring during activity, with stiffness or weakness soon after starting exercise | |||
* Muscle cramping | |||
* Muscle pain | |||
* Lasting (permanent) weakness in the thigh or other muscles. This happens in a small portion of people with the condition. | |||
Most of the time, people notice these symptoms before age 15. Often, people assume the symptoms are “growing pains” or due to some other cause. Different people may have symptoms of different severity eg person noticing that the symptoms seem worse or better at different times.<ref name=":1" /> | |||
== Diagnosis == | |||
Some diagnostic tests include: | |||
| | * [[Blood Tests|Blood tests]] to check for muscle enzymes, such as creatine kinase | ||
| | * DNA blood tests for known McArdle disease mutations | ||
* Electromyography to measure the electrical activity of the muscles | |||
* Forearm exercise test | |||
* [[MRI Scans|MRI]] studies of your muscles | |||
* Muscle biopsy to examine the muscle cells for glycogen buildup | |||
* Urine tests to check for myoglobin, which darkens the urine<ref name=":1" /> | |||
| | == Associated Co-morbidities == | ||
*[[Chronic Kidney Disease|'''Renal''' '''Failure''']]: Kidney dysfunction and failure are associated with rhadbomyolysis and myoglobinuria. | |||
| | *'''[[Gout]]''': Inhibited ATP production leads to the production or purine metabolites. These metabolites are converted to uric acid, which can lead to hyperuricemia. <ref name="p1" /><ref name="p2" /><ref>Driver MDCB. Gout Causes, Diet, Symptoms, Treatment & Medication [Internet]. MedicineNet. [cited 2017Apr5]. Available from: http://www.medicinenet.com/gout_gouty_arthritis/article.htm</ref> | ||
| | == Treatment == | ||
[[File:Fish.jpeg|right|frameless]] | |||
Patients with McArdle Disease cannot utilise their glycogen energy stores in their skeletal muscles. Despite a great deal of intensive investigation, no effective treatment for McArdle Disease has been found.<ref name=":2" /> | |||
Image 3: Creatine rich food, most people get creatine through seafood and red meat (though at levels far below those found in synthetically made creatine supplements) | |||
Persons may be able to use certain diet and exercise strategies to help control the problem. A well-designed low or moderate exercise routine may help the body get the most out of its' ability to use glucose. Overdoing exercise can harm the muscles and kidneys in people with McArdle disease. A healthcare team is vital in creating the best care plan for the situation. Some therapies used to help manage McArdle disease are: | |||
| | * Careful attention to a diet rich in carbohydrates | ||
* [[Creatine and Exercise|Creatine]] supplements | |||
* Eating or drinking prescribed amounts of sucrose before exercise | |||
* Prescribed, moderate aerobic exercise plan | |||
* Other medicines, such as ACE inhibitors | |||
People with McArdle disease need to work with their care team and physio to establish a safe exercise plan. | |||
There are currently no medications used to treat McArdle's Disease.<ref name=":1" /> | |||
== Diet == | |||
Certain dietary interventions which confer favorable effects include taking a sugary meal before planning exercise - for example, having a drink containing 75g sucrose 40 minutes before exercise alleviates typical symptoms of exercise intolerance. A diet rich in carbohydrates results in much better outcomes in comparison to a protein-rich diet. Other nutritional agents that were helpful for some patients but could not yield convincing outcomes during actual experimental studies include branched-chain amino acids, depot glucagon preparations, verapamil, dantrolene sodium, vitamin B6, high dose D-ribose, and high-dose creatine ingestion.<ref name=":0" /> | |||
== Physical Therapy Management == | |||
The physical therapist has an important role in keeping the patient active and avoiding inactivity due to fatigue.'''<br>'''Optimal exercise programs for managing McArdle’s Disease are aerobic based; they provide light resistance along with a [[Aerobic Exercise|cardiovascular]] component. | |||
| | *A plan of care incorporating low to moderate intensity [[Aerobic Exercise|aerobic physical activity]] can improve symptoms and reduce susceptibility to injury of the muscle. | ||
*The goal is to achieve the "second wind" for each muscle group that is being worked. | |||
*Light to moderate resistance training can also help, but allow adequate time to rest in between sets. | |||
*As a rule, do not work the muscles to absolute fatigue, and be sure to target larger muscle groups. | |||
*If strenuous activity must be done, use a 6 second rule. Only do that activity for 6 seconds prior to resting to ensure that only the phosphagen energy system is used in [[Anaerobic Exercise|anaerobic activity]].<br> | |||
'''Physical therapists can promote flexibility in order to prevent muscle contractures and reduce pain.''' | |||
*[[Stretching]] should be very light because maximal stretching will work the muscle anaerobically by inducing a protective contraction from the [[Golgi Tendon Organ|Golgi tendon]]. This strong protective contraction can lead to muscle damage. | |||
*Stretching following walking may offer immediate and dramatic pain relief to individuals with McArdle’s Disease. | |||
*For active individuals, stretching should take place very frequently to help reduce cramping. If not, muscles may become tight due to the toxic build up throughout activity and stretching can become painful. | |||
*Physical therapists should encourage a stretch that feels sufficient without causing pain. | |||
'''Physical therapists should promote active participation by patients in managing their disease.''' | |||
* | *Individuals with McArdle’s Disease can easily overexert themselves and become injured without even realizing it. | ||
*It is important that they be conscious of their energy levels, blood sugar, [[Pulse rate|heart rate]], and general well-being. | |||
*It is | |||
For a brief discussion of treating a patient with McArdle's Disease, refer to the video below. {{#ev:youtube|qsnDu-fLdRs}} | |||
< | <ref name="p5">Reference G. glycogen storage disease type V. Genetics Home Reference. 2017 [cited 18 March 2017]. Available from: https://ghr.nlm.nih.gov/condition/glycogen-storage-disease-type-v</ref><ref name="p0">Olafsen A. Quest - Article - McArdle’s Disease: The Right Diagnosis Can Lighten the Load - A Quest Article | Muscular Dystrophy Association. Muscular Dystrophy Association. 2017 [cited 18 March 2017]. Available from: https://www.mda.org/quest/article/mcardles-disease-diagnosis</ref><ref name="p5" /><ref name="p7">MedScape. [cited 19 April 2011]. Available from: http://www.medscape.org/viewarticle/581307_4</ref><ref>Exercise for Homeschoolers [Internet]. Texas Rock Gym. [cited 2017Apr5]. Available from: http://www.texasrockgym.com/exercise-for-homeschoolers/</ref> | ||
< | == Alternative/Holistic Management == | ||
[[Massage]]''':''' Individuals with McArdle’s Disease claim that massage therapy can be beneficial in maintaining an active lifestyle. Any massage should be light and fluid using effleurage techniques. Deep and hard massage for trigger point or myofascial release can be damaging to the muscle and should be avoided. Massages help push fatigue causing toxins out of the muscles and into the blood stream where they can be excreted from the body. It is recommended that individuals with McArdle’s Disease take in plenty of fluids following a massage to help flush the body of toxins. Pain with massage is a sign that rhabdomyolysis may be occurring. Do not continue massage therapy with pain.<ref name="p1" /><ref name="p2" /><ref>Home [Internet]. Natural Tranquility Massage and Bodywork LLC. [cited 2017Apr5]. Available from: http://naturaltranquilitymassage.com/</ref> | |||
== Differential Diagnosis == | |||
* | * [[Rhabdomyolysis]] | ||
*' | * [[Fibromyalgia]] | ||
* [[Muscular Dystrophy]] | |||
* [[Myositis Ossificans of the Quadriceps|Myositis]] | |||
* Tarui's Disease: A condition in which there exists a deficiency of the phosphofructokinase enzyme, which is needed to facilitate the breakdown of glucose into energy in muscle during exercise. Tarui’s Disease is also a glycogen storage deficiency, so it has many similarities to McArdle’s Disease. Consequently, they are treated in a similar manner. <ref name="p0" /><ref name="p1" /><ref name="p2" /><ref name="p3">Baechle Thomas R and Roger W Earle. Essentials of Strength Training and Conditioning. Human Kinetics. Champaign,IL 2008.</ref><ref name="p4">McArdle’s Disease (Glycogen Storage Disease Type V). Patient.info. 2017 [cited 18 March 2017]. Available from: http://patient.info/doctor/mcardles-disease-glycogen-storage-disease-type-v</ref> | |||
==Case Study McArdle Disease== | |||
This [[Case Study McArdle Disease|case]] demonstrates some of the day-to-day struggles of living with McArdle's Disease along with associated signs and symptoms of the disease. It also discusses abnormal lab values and possible physical therapy interventions and outcomes | |||
= | <ref name="p9">Quinlivan R, Martinuzzi A, Schoser B. Pharmacological and nutritional treatment for McArdle disease (Glycogen Storage Disease type V). 2017.</ref> | ||
== References == | |||
Special thank you to Andrew Wakelin, McArdle’s Disease (GSD Type V) Coordinator for AGSD UK for review and insight towards this page. | |||
<references /> | |||
[[Category:Conditions]] | |||
[[Category:Paediatrics - Conditions]] | |||
[[Category:Genetic Disorders]] | |||
[ | |||
Latest revision as of 15:28, 23 July 2023
Top Contributors - Edward Foring, Kaylynn Schwamb, Michael Helton, Lucinda hampton, Elaine Lonnemann, Kim Jackson, Admin, 127.0.0.1, Simone Potts and WikiSysop
Definition/Description[edit | edit source]
McArdle disease is a genetic disorder that mainly affects skeletal muscles. It occurs due to the deficiency or absence of an enzyme called myophosphorylase, a key substance that the muscles need to break down glycogen into sugar (glucose) for energy. Symptoms include painful muscle cramps, weakness, and fatigue manifested during periods of physical activity.[1] The disease can lead to dark urine.
- Severe, uncontrolled McArdle disease can cause life-threatening kidney problems.[2]
- To avoid the unpleasant symptoms associated with this condition and improve the quality of life, the disease requires prompt diagnosis and treatment.[1]
Etiology[edit | edit source]
McArdle disease typically results from mutations involving the muscle-specific isoform of the glycogen phosphorylase enzyme. This enzyme plays a key role in the first step of glycogenolysis that release glucose-1-phosphate monomers in muscle fibers. As a result, carbohydrate metabolism of the skeletal-muscle is affected, and energy cannot be generated from the glycogen stores of muscles.
Image 2:How muscle contraction differs in an unaffected muscle compared to one with McArdle’s Disease.
Epidemiology[edit | edit source]
The exact prevalence of McArdle disease is not precisely known and appears to range from 1 in 50,000 to 1 in 200,000 in the United States. [1]
Characteristics/Clinical Presentation[edit | edit source]
McArdle Disease patients can have critical episodes of early fatigue when exercising, muscle pain (myalgia), myoglobinuria (when muscles break down and release myoglobin in urine, making it brown/red in colour), and then subsequent kidney failure[5]. Some common symptoms of McArdle disease are:
- Better able to do aerobic exercise after 8 to 10 minutes (second-wind phenomenon)
- Brownish red urine, especially after periods of activity
- Easily tiring during activity, with stiffness or weakness soon after starting exercise
- Muscle cramping
- Muscle pain
- Lasting (permanent) weakness in the thigh or other muscles. This happens in a small portion of people with the condition.
Most of the time, people notice these symptoms before age 15. Often, people assume the symptoms are “growing pains” or due to some other cause. Different people may have symptoms of different severity eg person noticing that the symptoms seem worse or better at different times.[2]
Diagnosis[edit | edit source]
Some diagnostic tests include:
- Blood tests to check for muscle enzymes, such as creatine kinase
- DNA blood tests for known McArdle disease mutations
- Electromyography to measure the electrical activity of the muscles
- Forearm exercise test
- MRI studies of your muscles
- Muscle biopsy to examine the muscle cells for glycogen buildup
- Urine tests to check for myoglobin, which darkens the urine[2]
Associated Co-morbidities[edit | edit source]
- Renal Failure: Kidney dysfunction and failure are associated with rhadbomyolysis and myoglobinuria.
- Gout: Inhibited ATP production leads to the production or purine metabolites. These metabolites are converted to uric acid, which can lead to hyperuricemia. [3][4][6]
Treatment[edit | edit source]
Patients with McArdle Disease cannot utilise their glycogen energy stores in their skeletal muscles. Despite a great deal of intensive investigation, no effective treatment for McArdle Disease has been found.[5]
Image 3: Creatine rich food, most people get creatine through seafood and red meat (though at levels far below those found in synthetically made creatine supplements)
Persons may be able to use certain diet and exercise strategies to help control the problem. A well-designed low or moderate exercise routine may help the body get the most out of its' ability to use glucose. Overdoing exercise can harm the muscles and kidneys in people with McArdle disease. A healthcare team is vital in creating the best care plan for the situation. Some therapies used to help manage McArdle disease are:
- Careful attention to a diet rich in carbohydrates
- Creatine supplements
- Eating or drinking prescribed amounts of sucrose before exercise
- Prescribed, moderate aerobic exercise plan
- Other medicines, such as ACE inhibitors
People with McArdle disease need to work with their care team and physio to establish a safe exercise plan.
There are currently no medications used to treat McArdle's Disease.[2]
Diet[edit | edit source]
Certain dietary interventions which confer favorable effects include taking a sugary meal before planning exercise - for example, having a drink containing 75g sucrose 40 minutes before exercise alleviates typical symptoms of exercise intolerance. A diet rich in carbohydrates results in much better outcomes in comparison to a protein-rich diet. Other nutritional agents that were helpful for some patients but could not yield convincing outcomes during actual experimental studies include branched-chain amino acids, depot glucagon preparations, verapamil, dantrolene sodium, vitamin B6, high dose D-ribose, and high-dose creatine ingestion.[1]
Physical Therapy Management[edit | edit source]
The physical therapist has an important role in keeping the patient active and avoiding inactivity due to fatigue.
Optimal exercise programs for managing McArdle’s Disease are aerobic based; they provide light resistance along with a cardiovascular component.
- A plan of care incorporating low to moderate intensity aerobic physical activity can improve symptoms and reduce susceptibility to injury of the muscle.
- The goal is to achieve the "second wind" for each muscle group that is being worked.
- Light to moderate resistance training can also help, but allow adequate time to rest in between sets.
- As a rule, do not work the muscles to absolute fatigue, and be sure to target larger muscle groups.
- If strenuous activity must be done, use a 6 second rule. Only do that activity for 6 seconds prior to resting to ensure that only the phosphagen energy system is used in anaerobic activity.
Physical therapists can promote flexibility in order to prevent muscle contractures and reduce pain.
- Stretching should be very light because maximal stretching will work the muscle anaerobically by inducing a protective contraction from the Golgi tendon. This strong protective contraction can lead to muscle damage.
- Stretching following walking may offer immediate and dramatic pain relief to individuals with McArdle’s Disease.
- For active individuals, stretching should take place very frequently to help reduce cramping. If not, muscles may become tight due to the toxic build up throughout activity and stretching can become painful.
- Physical therapists should encourage a stretch that feels sufficient without causing pain.
Physical therapists should promote active participation by patients in managing their disease.
- Individuals with McArdle’s Disease can easily overexert themselves and become injured without even realizing it.
- It is important that they be conscious of their energy levels, blood sugar, heart rate, and general well-being.
For a brief discussion of treating a patient with McArdle's Disease, refer to the video below.
Alternative/Holistic Management[edit | edit source]
Massage: Individuals with McArdle’s Disease claim that massage therapy can be beneficial in maintaining an active lifestyle. Any massage should be light and fluid using effleurage techniques. Deep and hard massage for trigger point or myofascial release can be damaging to the muscle and should be avoided. Massages help push fatigue causing toxins out of the muscles and into the blood stream where they can be excreted from the body. It is recommended that individuals with McArdle’s Disease take in plenty of fluids following a massage to help flush the body of toxins. Pain with massage is a sign that rhabdomyolysis may be occurring. Do not continue massage therapy with pain.[3][4][11]
Differential Diagnosis[edit | edit source]
- Rhabdomyolysis
- Fibromyalgia
- Muscular Dystrophy
- Myositis
- Tarui's Disease: A condition in which there exists a deficiency of the phosphofructokinase enzyme, which is needed to facilitate the breakdown of glucose into energy in muscle during exercise. Tarui’s Disease is also a glycogen storage deficiency, so it has many similarities to McArdle’s Disease. Consequently, they are treated in a similar manner. [8][3][4][12][13]
Case Study McArdle Disease[edit | edit source]
This case demonstrates some of the day-to-day struggles of living with McArdle's Disease along with associated signs and symptoms of the disease. It also discusses abnormal lab values and possible physical therapy interventions and outcomes
References[edit | edit source]
Special thank you to Andrew Wakelin, McArdle’s Disease (GSD Type V) Coordinator for AGSD UK for review and insight towards this page.
- ↑ 1.0 1.1 1.2 1.3 Khattak ZE, Ashraf M. McArdle Disease. StatPearls [Internet]. 2020 Aug 15. Available:https://www.statpearls.com/articlelibrary/viewarticle/24796/ (accessed 23.10.2021)
- ↑ 2.0 2.1 2.2 2.3 Cedars Sinai McArdle Disease Available: https://www.cedars-sinai.org/health-library/diseases-and-conditions/m/mcardle-disease.html (accessed 23.10.2021)
- ↑ 3.0 3.1 3.2 3.3 MedPoster 1992. nobelprize.org. [cited 3 April 2011]. Available from: http://nobelprize.org/nobel_prizes/medicine/laureates/1992/illpres/glycogen.html
- ↑ 4.0 4.1 4.2 4.3 McArdlesDisease.org. [cited 17 March 2011]. Available from: www.mcardledisease.org
- ↑ 5.0 5.1 Brain Foundation McArdle Disease Award - 2012 Available: https://brainfoundation.org.au/research-grants/2012/mcardle-disease-award/ (accessed 23.10.2021)
- ↑ Driver MDCB. Gout Causes, Diet, Symptoms, Treatment & Medication [Internet]. MedicineNet. [cited 2017Apr5]. Available from: http://www.medicinenet.com/gout_gouty_arthritis/article.htm
- ↑ 7.0 7.1 Reference G. glycogen storage disease type V. Genetics Home Reference. 2017 [cited 18 March 2017]. Available from: https://ghr.nlm.nih.gov/condition/glycogen-storage-disease-type-v
- ↑ 8.0 8.1 Olafsen A. Quest - Article - McArdle’s Disease: The Right Diagnosis Can Lighten the Load - A Quest Article | Muscular Dystrophy Association. Muscular Dystrophy Association. 2017 [cited 18 March 2017]. Available from: https://www.mda.org/quest/article/mcardles-disease-diagnosis
- ↑ MedScape. [cited 19 April 2011]. Available from: http://www.medscape.org/viewarticle/581307_4
- ↑ Exercise for Homeschoolers [Internet]. Texas Rock Gym. [cited 2017Apr5]. Available from: http://www.texasrockgym.com/exercise-for-homeschoolers/
- ↑ Home [Internet]. Natural Tranquility Massage and Bodywork LLC. [cited 2017Apr5]. Available from: http://naturaltranquilitymassage.com/
- ↑ Baechle Thomas R and Roger W Earle. Essentials of Strength Training and Conditioning. Human Kinetics. Champaign,IL 2008.
- ↑ McArdle’s Disease (Glycogen Storage Disease Type V). Patient.info. 2017 [cited 18 March 2017]. Available from: http://patient.info/doctor/mcardles-disease-glycogen-storage-disease-type-v
- ↑ Quinlivan R, Martinuzzi A, Schoser B. Pharmacological and nutritional treatment for McArdle disease (Glycogen Storage Disease type V). 2017.