Lumbosacral Biomechanics: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editors '''[[User:Bert Lasat|Bert Lasat]]<br> | '''Original Editors '''[[User:Bert Lasat|Bert Lasat]]<br> | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
Revision as of 03:03, 28 November 2022
Original Editors Bert Lasat
Top Contributors - Lucinda hampton, Liza De Dobbeleer, Bert Lasat, Admin, Uchechukwu Chukwuemeka, Katherine Knight, Mariam Hashem, 127.0.0.1 and Simisola Ajeyalemi
Introduction[edit | edit source]
Biomechanics is the study of forces and their effects when applied to humans. Basic musculoskeletal biomechanics concepts are important for clinicians eg physical and occupational therapists and orthopaedic surgeons. A therapist assessment of a patient typically includes a biomechanical analysis. As the lumbosacral region is the most important region in the vertebral column in terms of mobility and weight bearing it is important to look at its biomechanics.[1]
As the lowest section of the mobile human spine, the lumbosacral spines main role lies in its ability to support the upper body by transmitting forces and bending moments to the pelvis via both sacroiliac joints. Like all regions of the spine, the lumbosacral spine protects the spinal cord and nerve roots from damage by providing a protective sheath. Mechanical stability is required to fulfill this task and to prevent premature mechanical and biologic deterioration of its structures. A complex interaction between the active (muscles), passive (osteoligamentous spine), and neural components is necessary to prevent instability.
Biomechanics: Lumbosacral Region[edit | edit source]
The 3 movements in the spine are flexion, extension, rotation and lateral flexion. These movements occur as a combination of rotation and translation in the following 3 planes of motion: sagittal, coronal and horizontal[2]. These movements result in various forces acting on the lumbar spine and sacrum: compressive force, tensile force, shear force, bending moment and torsional moment[3].
For example, with lumbar flexion, a compressive force is applied to the anterior aspect of the disc and a distractive force is applied to the posterior aspect of the disc. The opposite forces occur with lumbar extension[4].
The lumbar spine complex forms an effective load-bearing system. When a load is applied externally to the vertebral column, it produces stresses to the stiff vertebral body and the relatively elastic disc, causing strains to be produced more easily in the disc[5]. Pressure within the nucleus pulposus is greater than zero, even at rest, providing a “preload” mechanism allowing for greater resistance to applied forces[6]. Hydrostatic pressure increases within the intervertebral disc resulting in an outward pressure towards the vertebral endplates resulting in bulging of the annulus fibrosis and tensile forces within the concentric annular fibres. This transmission of forces effectively slows the application of pressure onto the adjacent vertebra, acting as a shock absorber[2]. The intervertebral discs are therefore an essential biomechanical feature, effectively acting as a fibrocartilage “cushion” transmitting force between adjacent vertebrae during spinal movement. The lumbar disc is more predisposed to injury compared with other spinal regions due to: the annular fibres being in a more parallel arrangement and thinner posteriorly compared with anteriorly, the nucleus being positioned more posteriorly, and the holes in the cartilaginous endplates[1].
When a load is applied along the spine, “shear” forces occur parallel to the intervertebral disc as the compression of the nucleus results in a lateral bulging of the annulus. Shear forces also occur as one vertebra moves, for example, forwards or backwards with respect to an adjacent vertebra with flexion and extension. Torsional stresses result from the external forces about the axis of twist[1]
and occur in the intervertebral disc with activity such as twisting of the spine.
The zygapophysial or “facet” joints provide stability to the intervertebral joint with respect to shear forces, whilst allowing primarily flexion and extension movement.
Mechanism of Injury / Pathological Process[edit | edit source]
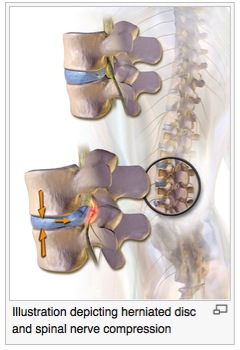
Experiments indicate “intervertebral disc herniation” or prolapse is likely to be as a result of a gradual or fatigue process rather than a traumatic injury [3], however clinically there is often a report of a sudden onset of symptoms associated with an incidental high loading of the spine, often in a flexed posture. The stresses most likely to result in injury to the spine are bending and torsion, and these combined movements reflect shear, compression and tension forces[1]. Twisting movements are more likely to injure the annulus as only half the collagen fibres are orientated to resist the movement in either direction[2]
The degenerative disc changes associated with aging have been considered normal. For example, the concentration levels of proteoglycans within the nucleus reduces with age, from 65% at early adulthood to 30% at the age of 60, corresponding to a reduction in nuclear hydration and concentration of elastic annular fibres over this time, resulting in a less resilient disc. Narrowing of the disc with age has long been considered, however large post-mortem studies indicate that the dimensions of the disc actually increase between the 2nd and 7th decades. Apparent disc narrowing may otherwise be considered a result of a process other than aging[2].
There are also reductions in vertebral endplate nutrition and vertebral body bone density levels. The reduction in support from the underlying bone results in “microfracture” and the migration of nuclear material into the vertebral body known as “Schmorl’s nodes”, usually seen in the thoracolumbar and thoracic spines and have a low incidence below the level of L2. The lumbar facet joint subchondral bone density increases until the age of 50 after which time it decreases, and the joint cartilage continues to thicken with age despite focal changes, particularly where shear forces during repeated flexion and extension are resisted. Other bony changes also occur at the facet joint including “osteophyte” and “wrap-around bumper” formation presumably due to repeated stress at the superior and inferior articular process regions respectively[2].
The processes of degeneration have also been considered as pathological. With respect to the facet joints “osteoarthritis” and “degenerative joint disease” are common diagnoses. “Spondylosis” and “intervertebral osteochondrosis” are also terms used to describe degenerative changes at the sites of the vertebrae and neural foraminae. “Degenerative disc disease” and are also common diagnoses.
The process of degeneration of the lumbar spine has been described in 3 phases[7][8]:
- Stage 1: “Early degeneration” involves increased laxity of the facet joints, fibrillation of the articular cartilage and intervertebral discs display grade 1-2 degenerative changes.
- Stage 2: “Lumbar instability” at the effected level(s) develops due to laxity of the facet capsules, cartilage degeneration and grade 2-3 degenerative disc disease. Segmental Instability: may be defined as loss of motion and segmental stiffness such that force application to that motion segment will produce greater displacements than would occur in a normal structure[7]. Mechanical testing suggests the intervertebral disc is most susceptible to herniation at this stage[3].
- Stage 3: “Fixed deformity” results from repair processes such as facet and peridiscal osteophytes effectively stabilising the motion segment. There is advanced facet joint degeneration (or “facet joint syndrome”) and grade 3-4 disc degeneration. Of clinical importance is altered spinal canal dimensions due to fixed deformity and osteophyte formation.
Importantly, the incidence of spondylosis and osteoarthritis are the same in patients with symptoms and without symptoms, raising the question of whether these conditions should always be viewed as pathological diagnoses[2]. This has clinical implications particularly with respect to interpretation of radiological investigation findings, and how results are presented to and discussed with patients.
Outcome Measures[edit | edit source]
Outcome measures regarding pain and disability include:
- Oswestry Disability Index
- Roland-Morris Disability Questionnaire
- Short-form McGill Pain Questionnaire
- Spinal Cord Independence Measure
- Numeric Pain Rating Scale
- Visual Analogue Scale
For further assessment of psychosocial factors associated with lumbosacral conditions, the following outcome measures may be useful:
- Orebro Musculoskeletal Pain Screening Questionnaire
- Depression Anxiety Stress Scale
- Fear Avoidance Beliefs Questionnaire
- Tampa Scale of Kinesiophobia
- Chronic Pain Acceptance Questionnaire
- Pain Catastrophizing Scale
Also see, Outcome Measures Database
Examination[edit | edit source]
Refer to Lumbar examination.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Jensen M Biomechanics of the lumbar intervertebral disk: a review. Physical Therapy. 1980; 60(6):765-773.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Bogduk, N. (2012). Radiological and Clinical Anatomy of the Lumbar Spine (5th ed.). China: Churchill Livingstone.
- ↑ 3.0 3.1 3.2 Adams M., Bogduk N., Burton K. Dolan P.. The Biomechanics of Back Pain. Eds. 2002. p238
- ↑ McKenzie, R. (1981). The lumbar spine : mechanical diagnosis and therapy. Waikanae, New Zealand: Spinal Publications.
- ↑ White A, Panjabi M. Clinical Biomechanics of the Spine. 1978, Philadelphia: JB Lippincott Co.
- ↑ Hirsch C. The reaction of intervertebral discs to compression forces. J Bone Joint Surg (Am) 1955; 37:1188-1191
- ↑ 7.0 7.1 Frymoyer JW, Selby DK. Segmental instability. Spine 1985; 10:280-286
- ↑ Kirkaldy-Wallis WH, Wedge JH, Yong-Hing K, Reilly J. Pathology and pathogenesis of lumbar spondylosis and stenosis. Spine 1978; 3(4):319-328