Lewy Body Disease
Original Editor - Henry Tan, Kevin Lam, Alex Mong, Andrew To as part of the Queen's University Neuromotor Function Project
Top Contributors - Henry Tan, Andrew To, Alex Mong, Lucinda hampton, Kim Jackson, Kevin Lam, Vidya Acharya, Claire Knott, 127.0.0.1, Evan Thomas and Lauren Lopez
Introduction[edit | edit source]
Lewy body disease or Lewy body dementia (LBD), is a neurodegenerative disease (specifically a synucleinopathy) related to Parkinson disease.[1]
Lewy body disease or Lewy body dementia (LBD) has been found to be strongly linked to a protein called alpha-synuclein. Abnormal accumulation of this protein in certain regions of the brain causes dramatic cognitive and motor deficits affecting behavior, mood, movement, and thinking. LBD is one of the most common causes of dementia along with Alzheimers disease (AD)[2]. It is also classified as a parkinsonism plus syndrome.
Types of LBD[edit | edit source]
There are 2 types of LBD generally described in the literature:[3]
- Dementia with Lewy Bodies: dementia occurring first or within one year of movement disorder.
- Parkinson Disease Dementia: dementia occurring in a patient who receives a diagnosed of Parkinson's disease and then develops dementia symptoms after one year or more of the diagnosis.
People with either type generally develop similar symptoms as the disease progresses. Distinct Parkinsonian symptoms such as slowness of movement, rigidity, REM sleep behaviour disorder and visual hallucinations can help to distinguish DLB from Alzheimer’s disease.[2]
Epidemiology[edit | edit source]
LBD occurs in older patients (onset typically in 50-70 years of age), and is sporadic. It is the second most common neurodegenerative cause of dementia in older patients (after AD), accounting for 15-20% of cases.[1]
Etiology[edit | edit source]
The etiology of LBD is unknown. Genetics, environmental factors, and changes linked to aging, may have a role and further research is still ongoing.[4]
Clinical Presentation[edit | edit source]
The clinical features of LBD are the consequence of the blockage of information transfer from the striatum to the cortex, more notably the frontal lobe.
Signs and symptoms include:[5]
- Recurrent visual hallucinations
- Visuospatial impairment (Stroop test, Clockface test)
- Executive function deficits (Nelson Card sort test)
- Parkinsonian motor features (mild gait impairments, resting tremor)
- Early extrapyramidal features (dystonia, akathisia, muscle rigidity, bradykinesia, tremor, tardive dyskinesia
- Fluctuating cognitive impairment (periods of coherence and alertness alternating with sequences of confusion and unresponsiveness)
- Attentional deficits
- Poor postural stability
- Neuroleptic sensitivity
- Orthostatic hypotension
Pathophysiology[edit | edit source]
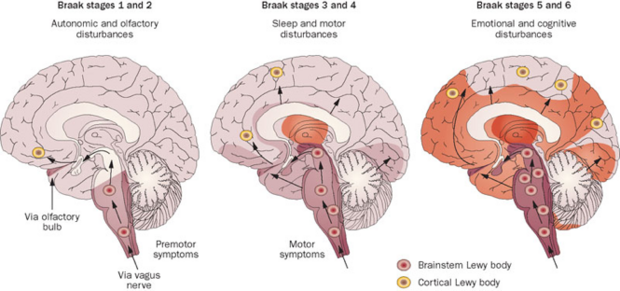
The characteristic feature of dementia with Lewy bodies is the accumulation of Lewy bodies throughout the brain. These intracellular inclusions result from the aggregation of misfolded α-synuclein. Neurofibrillary tangles are also present, however they lack an amyloid core, as seen in AD[1].
Source (http://labiotech.eu/major-cns-disease-milestones-in-biotech-2015/)
Diagnostic Procedures[edit | edit source]
It is difficult to diagnose LBD and due to similarities with AD and Parkinson’s symptoms, patients are often misdiagnosed.[6] Best practice in the diagnosis of LBD should include a thorough subjective examination, physical examination and neurological evaluation.
- Core features should be identified including fluctuations in cognition, visual hallucinations and any motor parkinsonism. If at least two of these symptoms are present, there is a greater likelihood an individual has DLB [3]
- Motor Parkinsonism features include rigidity, bradykinesia, masked face, stopped posture and shuffling gait[3]. With changes in cognition, a patient can experience variations in attention and alertness. They can also experience confusion from time to time and have fluctuations in mental abilities and behaviour [3]. If a patient experiences motor parkinsonism more than a year after a diagnosis of DLB, it is more appropriate to diagnose the patient with Parkinson's with dementia instead [3]
- Ultimately, the most definitive evidence of LBD is obtained via post mortem autopsies.[6]. Cortical and subcortical atrophy can be observed as well as atrophy of the grey matter of the temporal, frontal, and parietal lobes and the insular cortex with diagnostic imaging of patients with LBD[7]. There can also be volume loss in the hippocampus, amygdala and the basal ganglia, specifically the substantia nigra [7]. There can be atrophy of the nigrostriatal system and compromised dopamine transporters. This is more commonly seen in PDD [7].
Outcome Measures[edit | edit source]
The Unified Parkinson’s Disease Rating Scale (UPDRS) was used in a study in the assessment of parkinsonism in patients with Lewy Body Disease. The study suggests that use of the 5-item sub-scale of the UPDRS “provides a reliable and generally applicable instrument for the assessment of parkinsonism in patients with Lewy Body Disease”.[8]
Management[edit | edit source]
There is no effective treatment for LBD and the condition is progressive. The available pharmacological agents are only used to treat behavioral symptoms. Home care nurses play a crucial role in regularly assessing the patient and providing support services. Education of the caregiver is essential, the loved ones needing to be aware of the behavior changes, hallucinations, and fluctuations in cognition. Caregivers have to monitor the patient closely as they have a love level of functioning, with most unable to perform ADLs and are prone to falls and aspiration pneumonia. The pharmacist needs to educate caregivers that no medical therapy cures the cognitive changes and the drugs simply manage behavior and motor deficits ( and many have adverse effects). A mental health nurse is often needed as depression is common. Close communication between members of the interprofessional team is vital to improve outcomes.[4]
Physiotherapy Management[edit | edit source]
Physiotherapy for Lewy Body Disease is similar to that of Parkinson’s Disease. It can help manage parkinsonism that is prevalent in LBD by providing intervention which will encourage strengthening and flexibility exercises and gait training. Aerobic exercise should be included to optimise cardiovascular fitness.[6] Physiotherapy is especially helpful in improving balance and postural stability to minimize the risk of falls. With the addition of exercise, non-motor symptoms such as cognitive decline, sleep problems and fatigue will also improve. As the disease progresses and the dementia increases, exercise can be hard to do. Therefore, it is important to incorporate exercise in the early and middle stages of Lewy Body Disease. A study[9] suggests that a high-intensity functional exercise program has positive outcomes on balance in these patients.
Tips to help make exercise easier to maintain:[6]
- Provide visual cues by demonstrating exercises
- Play upbeat music or music the person enjoys
- Arrange exercise classes or include the support/care-person
- Do exercises in sitting
- Make exercise fun and enjoyable
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Radiopedia Dementia with Lewy bodies Available:https://radiopaedia.org/articles/dementia-with-lewy-bodies (accessed 13.9.2022)
- ↑ 2.0 2.1 National Institute on Aging. Lewy Body Dementia: Information for Patients, Families, and Professionals. (Accessed 4 May 2017). https://www.nia.nih.gov/alzheimers/publication/lewy-body-dementia/basics-lewy-body-dementia
- ↑ 3.0 3.1 3.2 3.3 3.4 McKeith IG, Galasko D, Kosaka K, Perry EK, Dickson DW, Hansen LA, Salmon DP, Lowe J, Mirra SS, Byrne EJ, Lennox G. Consensus guidelines for the clinical and pathologic diagnosis of dementia with Lewy bodies (DLB) Report of the consortium on DLB international workshop. Neurology. 1996 Nov 1;47(5):1113-24. PMID:8909416
- ↑ 4.0 4.1 Haider A, Spurling BC, Sánchez-Manso JC. Lewy body dementia. InStatPearls [Internet] 2021 Jul 12. StatPearls Publishing.Available:https://www.ncbi.nlm.nih.gov/books/NBK482441/ (accessed 13.9.2022)
- ↑ Gnanalingham KK, Byrne EJ, Thornton A, Sambrook MA, Bannister P. Motor and cognitive function in Lewy body dementia: comparison with Alzheimer's and Parkinson'ss. Journal of Neurology, Neurosurgery & Psychiatry. 1997 Mar 1;62(3):243-52. http://jnnp.bmj.com/content/jnnp/62/3/243.full.pdf
- ↑ 6.0 6.1 6.2 6.3 Lewy Body Dementia Association. What is LBD? Available from: https://www.lbda.org/category/3437/what-is-lbd.htm [Accessed May 5, 2017]
- ↑ 7.0 7.1 7.2 Morra LF, Donovick PJ. Clinical presentation and differential diagnosis of dementia with Lewy bodies: a review. International journal of geriatric psychiatry. 2014 Jun 1;29(6):569-76. DOI: 10.1002/gps.4039
- ↑ Boot B. P. Comprehensive treatment of dementia with Lewy bodies. Alzheimer’s Research Therapy, 2015 May 29; 7:45. DOI: 10.1186/s13195-015-0128-z
- ↑ Sondell A, Littbrand H, Holmberg H, Lindelöf N, Rosendahl E. Is the Effect of a High-Intensity Functional Exercise Program on Functional Balance Influenced by Applicability and Motivation among Older People with Dementia in Nursing Homes?. The journal of nutrition, health & aging. 2019 Dec 1;23(10):1011-20.









