Intersection Syndrome: Difference between revisions
No edit summary |
No edit summary |
||
| Line 25: | Line 25: | ||
The syndrome is typically the result of repetitive extension and flexion exercises or activities. It is commonly seen in sporting activities such as rowing or canoeing, skiing, racquet sports, and horseback riding. There is no significant difference in injury pattern found in men versus women | The syndrome is typically the result of repetitive extension and flexion exercises or activities. It is commonly seen in sporting activities such as rowing or canoeing, skiing, racquet sports, and horseback riding. There is no significant difference in injury pattern found in men versus women | ||
== | == Examination/Clinical Presentation == | ||
Look for | |||
* Swelling over the distal forearm as there can be some cases that present with a palpable finding on exam 4 cm - 6 cm proximal to Lister's tubercle. | |||
* Crepitus is a very common finding on the exam over the site of irritation (a finding that is specific to intersection syndrome). | |||
* The two dorsal compartments cross the movements of pronation and supination, create friction resulting in the exam finding of crepitus. | |||
* Pronation is typically found more uncomfortable than supination.<ref name=":0" /> | |||
* The [[Finkelstein Test|Finkelstein’s]] test resulted in uneasiness. The Finkelstein’s test is a passive stretch test with ulnar abduction and flexion of the thumb<ref name=":2">Costa CR, Morrison WB, Carrino JA. [https://www.ajronline.org/doi/full/10.2214/ajr.181.5.1811245 MRI features of intersection syndrome of the forearm.] American Journal of Roentgenology. 2003 Nov;181(5):1245-9.Available from:https://www.ajronline.org/doi/full/10.2214/ajr.181.5.1811245 (last accessed 1.4.2020)</ref>. | |||
# Intersection syndrome is a clinical diagnosis, although a musculoskeletal ultrasound can easily confirm it. Ultrasound technology has pushed musculoskeletal medicine forward in both diagnosis and treatment provided by physicians. | |||
# Plain film imaging and CT will not be helpful in the diagnosis of Intersection syndrome. | |||
# MRI would give excellent soft tissue picture and diagnosis, although MRI would not be a cost- or time-effective choice<ref name=":0" /> | |||
== Differential Diagnosis == | == Differential Diagnosis == | ||
| Line 40: | Line 43: | ||
* Extensor pollicis longus (EPL) tendinitis | * Extensor pollicis longus (EPL) tendinitis | ||
== | == Medical Management == | ||
Treatment is conservative management with rest and activity modification. | |||
Corticosteroid injection has shown significant improvement and is a known next best step if little or no improvement has been made with other conservative treatment. | |||
Anti-inflammatory medications are maybe useful for acute injury and pain relief. | |||
Common medications are ibuprofen, naproxen, meloxicam or diclofenac. Acetaminophen also may be utilized for pain relief as well. | |||
<br>Surgery is only required in case of persisting symptoms after an already adequate course of conservative treatment.<ref name=":2" /> | |||
Surgery is contraindicated in patients with vague nonspecific complaints or in those patients who have not received or been compliant with recommended unoperative measures. | |||
== | == Physical Therapy Management == | ||
<br>The | The intersection syndrome is usually managed conservatively.<br>The first step of this management includes modification of work and sport activities, which will help to reduce stress on the wrist and splinting. | ||
Secondly oral nonsteroidal inflammatory medication or local ice-pack placement can also reduce pain. | |||
A temporary splint for protection and comfort at night may also be beneficial (a neutral position with a splint), an activity change and anti-inflammatory medication is normally appropriate to control the symptoms. | |||
Conservative management with immobilization (a neutral position with a splint), an activity change and anti-inflammatory medication is normally appropriate to control the symptoms. | Conservative management with immobilization (a neutral position with a splint), an activity change and anti-inflammatory medication is normally appropriate to control the symptoms. | ||
Taping can eliminate crepitus<ref>Kaneko S, Takasaki H. [https://www.ncbi.nlm.nih.gov/pubmed/21471652 Forearm pain, diagnosed as intersection syndrome, managed by taping: a case series]. journal of orthopaedic & sports physical therapy. 2011 Jul;41(7):514-9. Available from:https://www.ncbi.nlm.nih.gov/pubmed/21471652 (last accessed 1.4.2020)</ref>. | |||
If surgical intervention was performed physical therapy after a surgical intervention should occur. | |||
Includes | |||
* Therapeutic exercises | |||
* Joint and scar mobilization | |||
* soft tissue massage | |||
* stretching | |||
* physical agents. | |||
* Patient education concerning activity modification. | |||
=== References === | |||
<br> | |||
[[Category:Injury]] | [[Category:Injury]] | ||
| Line 82: | Line 90: | ||
[[Category:Sports Medicine]] | [[Category:Sports Medicine]] | ||
[[Category:Sports Injuries]] | [[Category:Sports Injuries]] | ||
<references /> | |||
Revision as of 08:03, 1 April 2020
Original Editors - Emilie Depasse
Top Contributors - Kim Jackson, Lucinda hampton, Emilie Depasse, Evan Thomas, Vidya Acharya and Wanda van Niekerk
Introduction[edit | edit source]
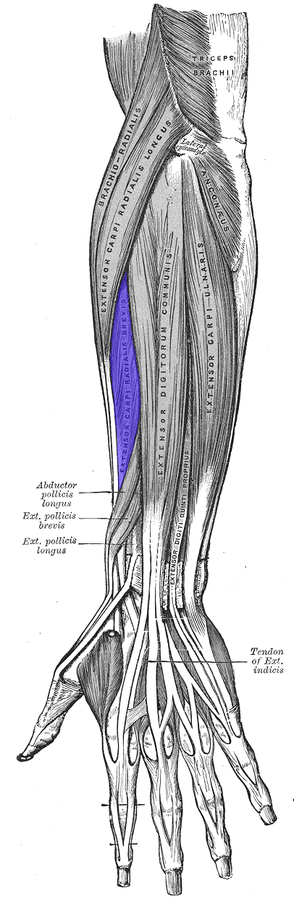
Intersection syndrome is a condition that affects the first and second compartments of the dorsal wrist extensors. The condition is thought to occur as a result of repetitive friction at the junction in which the tendons of the first dorsal compartment cross over the second, creating a tenosynovitis. This is typically noted as a pain just proximal and dorsal to the radial styloid, or also noted anatomically by 4 cm - 6 cm proximal to Lister's tubercle[1]
The term "intersection syndrome" refers to the intersection (at an angle of around 60°) of the musculotendinous junctions of the first and second extensor compartment tendons[2].
The intersection syndrome is a relative uncommon disorder that is often misdiagnosed with other conditions, such as ‘De Quervain’s tenosynovitis.[3]
Pathology[edit | edit source]
The musculotendinous junctions of the first extensor compartment tendons (abductor pollicis longus and extensor pollicis brevis tendons) intersect the second extensor compartment tendons (extensor carpi radialis longus and extensor carpi radialis brevis tendons).
This intersection is at an angle of approximately 60°, approximately 4 cm proximal to Lister's tubercle (a bony protuberance on the dorsal surface of the distal radius).
In intersection syndrome there is tenosynovitis particularly of the second extensor compartment possibly caused by friction from the overlying first compartment tendons[2]
The presentation is typically one that the patient complains of pain or tenderness over the dorsal aspect of the wrist proximal to the radial styloid. There may also be swelling and crepitus that is palpable on the exam with wrist and/or thumb extension[1]
Epidemiology[edit | edit source]
The syndrome is typically the result of repetitive extension and flexion exercises or activities. It is commonly seen in sporting activities such as rowing or canoeing, skiing, racquet sports, and horseback riding. There is no significant difference in injury pattern found in men versus women
Examination/Clinical Presentation[edit | edit source]
Look for
- Swelling over the distal forearm as there can be some cases that present with a palpable finding on exam 4 cm - 6 cm proximal to Lister's tubercle.
- Crepitus is a very common finding on the exam over the site of irritation (a finding that is specific to intersection syndrome).
- The two dorsal compartments cross the movements of pronation and supination, create friction resulting in the exam finding of crepitus.
- Pronation is typically found more uncomfortable than supination.[1]
- The Finkelstein’s test resulted in uneasiness. The Finkelstein’s test is a passive stretch test with ulnar abduction and flexion of the thumb[4].
- Intersection syndrome is a clinical diagnosis, although a musculoskeletal ultrasound can easily confirm it. Ultrasound technology has pushed musculoskeletal medicine forward in both diagnosis and treatment provided by physicians.
- Plain film imaging and CT will not be helpful in the diagnosis of Intersection syndrome.
- MRI would give excellent soft tissue picture and diagnosis, although MRI would not be a cost- or time-effective choice[1]
Differential Diagnosis[edit | edit source]
- De Quervain tenosynovitis (first extensor compartment involvement only, located more distal at the radial styloid)[2]
- Muscle strain
- Entrapment of the dorsal radial sensory nerve as it emerges beneath the brachioradialis (Wartenberg’s syndrome)
- Thumb CMC arthritis
- Extensor pollicis longus (EPL) tendinitis
Medical Management[edit | edit source]
Treatment is conservative management with rest and activity modification.
Corticosteroid injection has shown significant improvement and is a known next best step if little or no improvement has been made with other conservative treatment.
Anti-inflammatory medications are maybe useful for acute injury and pain relief.
Common medications are ibuprofen, naproxen, meloxicam or diclofenac. Acetaminophen also may be utilized for pain relief as well.
Surgery is only required in case of persisting symptoms after an already adequate course of conservative treatment.[4]
Surgery is contraindicated in patients with vague nonspecific complaints or in those patients who have not received or been compliant with recommended unoperative measures.
Physical Therapy Management[edit | edit source]
The intersection syndrome is usually managed conservatively.
The first step of this management includes modification of work and sport activities, which will help to reduce stress on the wrist and splinting.
Secondly oral nonsteroidal inflammatory medication or local ice-pack placement can also reduce pain.
A temporary splint for protection and comfort at night may also be beneficial (a neutral position with a splint), an activity change and anti-inflammatory medication is normally appropriate to control the symptoms.
Conservative management with immobilization (a neutral position with a splint), an activity change and anti-inflammatory medication is normally appropriate to control the symptoms.
Taping can eliminate crepitus[5].
If surgical intervention was performed physical therapy after a surgical intervention should occur.
Includes
- Therapeutic exercises
- Joint and scar mobilization
- soft tissue massage
- stretching
- physical agents.
- Patient education concerning activity modification.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Michols NJ, Kiel J. Intersection Syndrome. InStatPearls [Internet] 2019 Apr 2. StatPearls Publishing.Available from:https://www.ncbi.nlm.nih.gov/books/NBK430899/ (last accessed 1.4.2020)
- ↑ 2.0 2.1 2.2 Radiopedia Intersection Syndrome Available from: https://radiopaedia.org/articles/intersection-syndrome (last accessed 1.4.2020)
- ↑ de Lima JE, Kim HJ, Albertotti F, Resnick D. Intersection syndrome: MR imaging with anatomic comparison of the distal forearm. Skeletal radiology. 2004 Nov 1;33(11):627-31.Available from:https://www.ncbi.nlm.nih.gov/pubmed/15365785 (last accessed 1.4.2020)
- ↑ 4.0 4.1 Costa CR, Morrison WB, Carrino JA. MRI features of intersection syndrome of the forearm. American Journal of Roentgenology. 2003 Nov;181(5):1245-9.Available from:https://www.ajronline.org/doi/full/10.2214/ajr.181.5.1811245 (last accessed 1.4.2020)
- ↑ Kaneko S, Takasaki H. Forearm pain, diagnosed as intersection syndrome, managed by taping: a case series. journal of orthopaedic & sports physical therapy. 2011 Jul;41(7):514-9. Available from:https://www.ncbi.nlm.nih.gov/pubmed/21471652 (last accessed 1.4.2020)