Iliocostalis Lumborum: Difference between revisions
No edit summary |
No edit summary |
||
| Line 43: | Line 43: | ||
== Clinical Relevance: == | == Clinical Relevance: == | ||
Myofascial pain<ref>Roldan CJ, Huh BK. Iliocostalis Thoracis-Lumborum Myofascial Pain: Reviewing a Subgroup of a Prospective, Randomized, Blinded Trial. A Challenging Diagnosis with Clinical Implications. Pain physician. 2016 Aug 1;19:363-72.https://www.ncbi.nlm.nih.gov/pubmed/27454266</ref> of Iliocostalis Lumborum muscle causes anterior torso pain. The pain of myofascial origin is a well-recognized pathology characterized by the presence of two components: ''referred pain; which is'' ''often distant from its source'' and specific to each muscle, and the ''trigger point, a localized hyperirritable band present in the affected muscle'' and able to reproduce the referred pain when stimulated. The most common locations of pain were the right-lower quadrant and the left side of the chest. | |||
often resulted in extensive workups before ITL myofascial pain was diagnosed. TP injections were diagnostic and therapeutic of ITL myofascial pain.Unsurprisingly, since the referred pain of MP of the ITL muscle is located at the frontal aspect of the torso (chest, abdomen, and pelvis), it can represent a clinical challenge even to seasoned clinicians. Because the literature on ITL MP is sparse, I considered relevant to characterize the manifestations, diagnosis, and clinical implications of ITL MP. Myofascial pain (MP) commonly coexists in patients with acute or chronic pain of other etiologies. The uniqueness of the clinical presentation of some MPs and the lack of training of most specialties represent a clinical challenge. Thus, many patients with MPS receive less than optimal management of this condition. | |||
* Investigative studies like EMG<ref>Geroin C, Squintani G, Morini A, Donato F, Smania N, Gandolfi M, Tamburin S, Fasano A, Tinazzi M. Pisa syndrome in Parkinson’s disease: electromyographic quantification of paraspinal and non-paraspinal muscle activity. Functional neurology. 2017 Jul;32(3):143.https://www.ncbi.nlm.nih.gov/pubmed/29042003</ref> have shown the involvement of Iliocostalis Lumborum along with external obliques in Pisa Syndrome, which is defined as a reversible lateral bending of the trunk with a tendency to lean to one side<ref>Barone P, Santangelo G, Amboni M, Pellecchia MT, Vitale C. Pisa syndrome in Parkinson's disease and parkinsonism: clinical features, pathophysiology, and treatment. The Lancet Neurology. 2016 Sep 1;15(10):1063-74.https://www.ncbi.nlm.nih.gov/pubmed/27571158</ref>. This is a frequent and often disabling complication of Parkinson's disease. As some forms of Pisa syndrome are potentially reversible, there is growing consensus on the importance of its early recognition and the importance of pharmacological adjustment and rehabilitation.<ref>Tinazzi M, Geroin C, Gandolfi M, Smania N, Tamburin S, Morgante F, Fasano A. Pisa syndrome in Parkinson's disease: An integrated approach from pathophysiology to management. Movement Disorders. 2016 Dec 1;31(12):1785-95.https://www.ncbi.nlm.nih.gov/pubmed/27779784</ref> | |||
Pisa Syndrome <ref>Barone P, Santangelo G, Amboni M, Pellecchia MT, Vitale C. Pisa syndrome in Parkinson's disease and parkinsonism: clinical features, pathophysiology, and treatment. The Lancet Neurology. 2016 Sep 1;15(10):1063-74.https://www.ncbi.nlm.nih.gov/pubmed/27571158</ref> | |||
== Assessment<ref name=":0" /> == | == Assessment<ref name=":0" /> == | ||
Revision as of 22:29, 27 June 2018
Original Editor - Oyemi Sillo
Lead Editors - Vidya Acharya, Oyemi Sillo, Kim Jackson, Abbey Wright, Lucinda hampton, Evan Thomas, WikiSysop and 127.0.0.1
Description[edit | edit source]
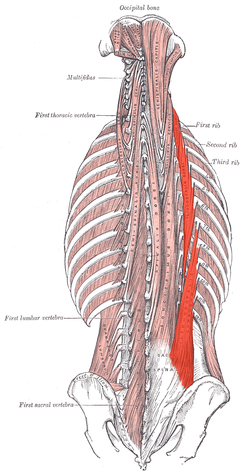
Iliocostalis Lumborum belongs to the lateral column of the Sacrospinalis group of muscles.[1] It is the most inferior and lateral of the erector spinae muscles.[2]
Anatomy[edit | edit source]
Origin[edit | edit source]
Anterior surface of a broad and thick tendon w attached to the medial crest of sacrum, spinous processes of the lumbar vertebrae, 11th and 12th thoracic vertebrae, posterior part of the medial lip of iliac crest, supra-spinous ligament and the lateral crest of sacrum[3].
Insertion[edit | edit source]
By tendons into inferior borders of the angles of the lower 6 or 7 ribs[3][4]
Nerve Supply[edit | edit source]
Dorsal rami of thoracic and lumbar spinal nerves (T7 to L3)[5]
Blood Supply[edit | edit source]
Dorsal branches of the lumbar arteries from the aorta. Dorsal branches of the lateral sacral artery from the internal iliac artery.[5]
Muscle Fibre[edit | edit source]
Characterised by Type 1 muscle fibre, indicating the tonic holding and stabilisation function.[6]
Action[edit | edit source]
- Extension of Spine: Acting bilaterally, extension and hyperextension of the spine. Acting unilaterally, laterally flexes the spine[4]
- Respiration: It assists as an accessory muscle of expiration, due to its insertion on the ribs[7]
- Stabilization of Spine: Iliocostalis lumborum along with multifidus contribute to support and control the orientation of lumbar spine.[6]
Clinical Relevance:[edit | edit source]
Myofascial pain[8] of Iliocostalis Lumborum muscle causes anterior torso pain. The pain of myofascial origin is a well-recognized pathology characterized by the presence of two components: referred pain; which is often distant from its source and specific to each muscle, and the trigger point, a localized hyperirritable band present in the affected muscle and able to reproduce the referred pain when stimulated. The most common locations of pain were the right-lower quadrant and the left side of the chest.
often resulted in extensive workups before ITL myofascial pain was diagnosed. TP injections were diagnostic and therapeutic of ITL myofascial pain.Unsurprisingly, since the referred pain of MP of the ITL muscle is located at the frontal aspect of the torso (chest, abdomen, and pelvis), it can represent a clinical challenge even to seasoned clinicians. Because the literature on ITL MP is sparse, I considered relevant to characterize the manifestations, diagnosis, and clinical implications of ITL MP. Myofascial pain (MP) commonly coexists in patients with acute or chronic pain of other etiologies. The uniqueness of the clinical presentation of some MPs and the lack of training of most specialties represent a clinical challenge. Thus, many patients with MPS receive less than optimal management of this condition.
- Investigative studies like EMG[9] have shown the involvement of Iliocostalis Lumborum along with external obliques in Pisa Syndrome, which is defined as a reversible lateral bending of the trunk with a tendency to lean to one side[10]. This is a frequent and often disabling complication of Parkinson's disease. As some forms of Pisa syndrome are potentially reversible, there is growing consensus on the importance of its early recognition and the importance of pharmacological adjustment and rehabilitation.[11]
Assessment[3][edit | edit source]
Power[edit | edit source]
Position: Prone with hands clasped behind buttocks or head.
Fixation: Examiner must stabilize the legs firmly on the table.
Test: Trunk extension
Pressure: If performed with hands behind back no pressure is needed.
Weakness[edit | edit source]
Bilateral weakness of low back muscles results in a lumbar kyphosis and increased thoracic kyphosis.
Unilateral weakness results in lateral curvature with convexity towards the weak side.
Length[edit | edit source]
Bilateral contracture of low back muscles results in lordosis.
Unilateral contracture results in scoliosis with convexity to the opposite side.
Treatment[edit | edit source]
Strengthening[edit | edit source]
References[edit | edit source]
- ↑ Gray, Henry. Anatomy of the Human Body. Philadelphia: Lea & Febiger, 1918; Bartleby.com, 2000. www.bartleby.com/107/.
- ↑ Muscles That Influence the Spine; Barclay W. Bakkum, Gregory D. Cramer, in Clinical Anatomy of the Spine, Spinal Cord, and Ans (Third Edition), 2014 https://www.sciencedirect.com/topics/neuroscience/iliocostalis
- ↑ 3.0 3.1 3.2 Muscle Testing and Function;4th Edition; Kendall, McCreary, Provance; Page No.138.
- ↑ 4.0 4.1 http://www.wheelessonline.com/ortho/iliocostalis_lumborum_1
- ↑ 5.0 5.1 http://www.anatomyexpert.com/app/structure/5243/
- ↑ 6.0 6.1 Therapeutic Exercise for Spine Segmental Stabilization in Low Back Pain; Richardson, Jull, Hodges, Hides; Scientific Basis; Page No.24.
- ↑ Muscles Testing and Function;4th Edition; Kendall, McCreary, Provance; Accessory Muscles of Respiration, Page No.330.
- ↑ Roldan CJ, Huh BK. Iliocostalis Thoracis-Lumborum Myofascial Pain: Reviewing a Subgroup of a Prospective, Randomized, Blinded Trial. A Challenging Diagnosis with Clinical Implications. Pain physician. 2016 Aug 1;19:363-72.https://www.ncbi.nlm.nih.gov/pubmed/27454266
- ↑ Geroin C, Squintani G, Morini A, Donato F, Smania N, Gandolfi M, Tamburin S, Fasano A, Tinazzi M. Pisa syndrome in Parkinson’s disease: electromyographic quantification of paraspinal and non-paraspinal muscle activity. Functional neurology. 2017 Jul;32(3):143.https://www.ncbi.nlm.nih.gov/pubmed/29042003
- ↑ Barone P, Santangelo G, Amboni M, Pellecchia MT, Vitale C. Pisa syndrome in Parkinson's disease and parkinsonism: clinical features, pathophysiology, and treatment. The Lancet Neurology. 2016 Sep 1;15(10):1063-74.https://www.ncbi.nlm.nih.gov/pubmed/27571158
- ↑ Tinazzi M, Geroin C, Gandolfi M, Smania N, Tamburin S, Morgante F, Fasano A. Pisa syndrome in Parkinson's disease: An integrated approach from pathophysiology to management. Movement Disorders. 2016 Dec 1;31(12):1785-95.https://www.ncbi.nlm.nih.gov/pubmed/27779784