Hip Quadrant Test: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) (Updated categories) |
||
| (22 intermediate revisions by 9 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original Editor ''' [[User:Laurent Chapelle|Laurent Chapelle]] | |||
{ | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | |||
== Definition/Description == | |||
The Hip Quadrant test is a passive test that is used to assess if the hip is the source of a patient's symptoms. The hip quadrant test is also known as the quadrant scour test<ref name="p3">] Peter H. Seidenberg,Jimmy D. Bowen - The Hip and Pelvis in Sports Medicine and Primary Care pg. 33. Peter H. Seidenberg and Jimmy D. Bowen (editors). Springer (publisher) Evidence level: 5 grade of recommendation: F</ref><ref name=":1">Cook CE, Hegedus EJ. ''Orthopedic Physical Examination: An Evidence based Approach.'' Upper Saddle River, NJ: Pearson Prentice Hall; 2008.</ref>. This test is not to be confused with the quadrant test for the lumbar spine.<ref name="p6">Lyle MA, Manes S, McGuinness M, Ziaei S, Iversen MD.Relationship of physical examination findings and self-reported symptom severity and physical function in patients with degenerative lumbar conditions. Phys Ther. 2005 Feb;85(2):120-33. Evidence level: 2a grade of recommendation: B</ref> | |||
<br> | |||
== Clinically Relevant Anatomy == | |||
[[File:Anatomy human hip.jpg|thumb]] | |||
The hip articulation is true diarthroidal ball and-socket style joint, formed from the head of the femur as it articulates with the acetabulum of the pelvis. This joint serves as the main connection between the lower extremity and the trunk, and typically works in a closed kinematic chain<ref>Hip Anatomy. (2017, June 6). ''Physiopedia,'' . Retrieved 10:17, December 14, 2017 from https://www.physio-pedia.com/index.php?title=Hip_Anatomy&oldid=172875.</ref>. Thus is designed for stability and weight-bearing – rather than a large range of movement. Motions available at the hip joint are flexion, extension, abduction, adduction, internal rotation and external rotation. The ligaments of the hip joint act to increase stability. They can be divided into two groups – intracapsular and extracapsular. | |||
For more detailed information on the anatomy of the [[Hip Anatomy|hip]], [[Lumbar|lumbar spine]] and [[Sacroiliac Joint]]. | |||
The | The most important structures of the art. coxae are the fossa acetabuli, facies lunata, labrum acetabuli, lig. transversum acetabuli, caput femoris, lig. ischiofemorale, lig iliofemorale and lig. pubofemorale. The art. Coxae is an articulation sphaeroidea.<ref name="p0">Human anatomy atlas Sobotta part 2: lower extremity pg 263 – 272. Bohn Stafleu, Van Loghum
3th print R. Putz and R. Pabst</ref> <ref name="fig. 1">figure 1: http://www.healthbase.com/resources/images/</ref> | ||
<br> | <br> | ||
== Purpose == | |||
== Purpose | |||
The purpose of the Hip Quadrant test is to determine if there is a nonspecific hip pathology and a change in ROM. This test does so by completing the ROM from flexion and adduction to flexion and abduction<ref name="p1">M. Lynn Palmer – Fundamentals of musculoskeletal assessment techniques pg. 305. Second edition, M lynn palmer and Marcia E. Epler. Uppincott Williams and Willens (publisher) Evidence level: 5 grade of recommendation: F</ref><ref name=":1" />. This test is also capable to detect early hip degeneration.<ref name="p5">Manning C, Hudson Z. Comparison of hip joint range of motion in professional youth and senior team footballers with age-matched controls: an indication of early degenerative change? Phys Ther Sport. 2009 Feb;10(1):25-9. Epub 2008 Dec 24.fckLREvidence level: 3a grade of recommendation: C</ref> | |||
<br> | <br> | ||
== Technique == | == Technique == | ||
The patient | The patient is positioned in supine on the plinth. The therapist stands on the side of the leg to be tested. The affected limb is placed in adduction and a compression force is applied and maintained through the femur through a range of 70-140 degrees of hip flexion. The test is repeated in abduction. A positive test is a reproduction of the patient's worst pain that they came with into the clinic.<ref name=":0">https://www.thestudentphysicaltherapist.com/hip-quadrant-test.html</ref><ref name="p7" /><ref name="p1" /><ref name="p3" /><ref name="p3" /><br>{{#ev:youtube|rUO8zeHKOxI}}<br> | ||
== Interpretation == | |||
The test is considered positive if the patient has any pain. The test is also positive if the therapist can feel any crepitus or if there is a leathery end feeling or if there’s a loss in ROM.<ref name="p1" /><ref name=":1" /> | |||
The test is considered negative if you can go from flexion-adduction to flexion-abduction in an arch, a normal ROM and with a normal end-feeling.<ref name="p1" /><ref name="p3" /> | |||
< | |||
= | This test works by scouring the femoral acetabular joint for pathology. The compression of the femur, through the various ranges, stresses the bone, labrum, cartilage, ligaments, etc. While this test has been labeled as the "hip clearing test," due to the low diagnostic accuracy, it should not necessarily be used as such. Consider the results of the rest of your exam when trying to determine the pathology.<ref name=":0" /><br> | ||
== Dysfunction == | |||
<br> | A positive Hip Quadrant test is an indication that there might be arthritis, an osteochondral defect, avascular necrosis, joint capsule tightness and/or an acetabular labrum defect<ref name="p4">Mitchell B, McCrory P, Brukner P, O'Donnell J, Colson E, Howells R. Hip joint pathology: clinical presentation and correlation between magnetic resonance arthrography, ultrasound, and arthroscopic findings in 25 consecutive cases. Clin J Sport Med. 2003 May;13(3):152-6. Evidence level: 2c grade of recommendation: C</ref>. This test also detects if the patients hip can move through the full range of motion.<ref name="p7">Thomas A. Souza Differential Diagnosis and Management for the Chiropractor: Protocols and algorithms pg 345. Fourth edition, Thomas A. Souza, DC, DACBSP. Jean and Bartlett publishers (Sanburry, Massachusetts). Evidence level: 5 grade of recommendation: F</ref><br> | ||
== | == Evidence == | ||
Th hip quadrant test does not give us any significantly useful information. Due to the wide range of structures that can be stressed, its results should be interpreted with caution. No validity or reliability studies could be located for its diagnostic validity. | |||
Minimal data is available on the significance of the Hip Quadrant alone. However, the American College of Rheumatology provide an alternative method for the diagnosis of hip OA. | |||
There are 2 cluster diagnoses which are: | |||
'''Cluster 1:''' | |||
# Pain in the hip | |||
# <115 degrees of hip flexion | |||
# < 15 degrees of hip IR | |||
'''Cluster 2:''' | |||
# Pain with hip IR | |||
# > 60 minutes of AM stiffness | |||
# > 50 years old<ref name=":2">Altman R, Alarcon G, Appelrouth D, et al. The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. ''Arthritis Rheum'' 1991: 34l 505-514.</ref> | |||
# | |||
If at least 4 of 5 variables were present, the positive LR was equal to 24.3 (95% confidence interval: 4.4-142.1), increasing the probability of hip OA to 91%.<ref name=":2" /> | |||
== References == | |||
<references /> | |||
[[Category:Special_Tests]] | |||
[[Category:Hip]] | |||
[[Category:Musculoskeletal/Orthopaedics]] | |||
[[Category:Sports Medicine]] | |||
[[Category:Assessment]] | |||
[[Category:Athlete Assessment]] | |||
[[Category:Hip - Assessment and Examination]] | |||
[[Category:Hip - Special Tests]] | |||
Latest revision as of 20:55, 31 January 2021
Original Editor Laurent Chapelle
Top Contributors - Rachael Lowe, Tyler Shultz, Oyemi Sillo, Laurent Chapelle, Kim Jackson, Admin, WikiSysop, Adam Vallely Farrell, Evan Thomas, 127.0.0.1 and Wanda van Niekerk
Definition/Description[edit | edit source]
The Hip Quadrant test is a passive test that is used to assess if the hip is the source of a patient's symptoms. The hip quadrant test is also known as the quadrant scour test[1][2]. This test is not to be confused with the quadrant test for the lumbar spine.[3]
Clinically Relevant Anatomy[edit | edit source]
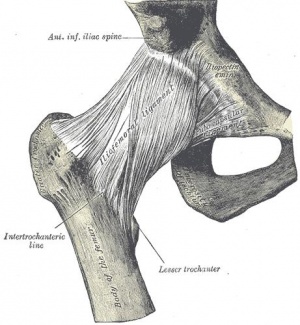
The hip articulation is true diarthroidal ball and-socket style joint, formed from the head of the femur as it articulates with the acetabulum of the pelvis. This joint serves as the main connection between the lower extremity and the trunk, and typically works in a closed kinematic chain[4]. Thus is designed for stability and weight-bearing – rather than a large range of movement. Motions available at the hip joint are flexion, extension, abduction, adduction, internal rotation and external rotation. The ligaments of the hip joint act to increase stability. They can be divided into two groups – intracapsular and extracapsular.
For more detailed information on the anatomy of the hip, lumbar spine and Sacroiliac Joint.
The most important structures of the art. coxae are the fossa acetabuli, facies lunata, labrum acetabuli, lig. transversum acetabuli, caput femoris, lig. ischiofemorale, lig iliofemorale and lig. pubofemorale. The art. Coxae is an articulation sphaeroidea.[5] [6]
Purpose[edit | edit source]
The purpose of the Hip Quadrant test is to determine if there is a nonspecific hip pathology and a change in ROM. This test does so by completing the ROM from flexion and adduction to flexion and abduction[7][2]. This test is also capable to detect early hip degeneration.[8]
Technique[edit | edit source]
The patient is positioned in supine on the plinth. The therapist stands on the side of the leg to be tested. The affected limb is placed in adduction and a compression force is applied and maintained through the femur through a range of 70-140 degrees of hip flexion. The test is repeated in abduction. A positive test is a reproduction of the patient's worst pain that they came with into the clinic.[9][10][7][1][1]
Interpretation[edit | edit source]
The test is considered positive if the patient has any pain. The test is also positive if the therapist can feel any crepitus or if there is a leathery end feeling or if there’s a loss in ROM.[7][2]
The test is considered negative if you can go from flexion-adduction to flexion-abduction in an arch, a normal ROM and with a normal end-feeling.[7][1]
This test works by scouring the femoral acetabular joint for pathology. The compression of the femur, through the various ranges, stresses the bone, labrum, cartilage, ligaments, etc. While this test has been labeled as the "hip clearing test," due to the low diagnostic accuracy, it should not necessarily be used as such. Consider the results of the rest of your exam when trying to determine the pathology.[9]
Dysfunction[edit | edit source]
A positive Hip Quadrant test is an indication that there might be arthritis, an osteochondral defect, avascular necrosis, joint capsule tightness and/or an acetabular labrum defect[11]. This test also detects if the patients hip can move through the full range of motion.[10]
Evidence[edit | edit source]
Th hip quadrant test does not give us any significantly useful information. Due to the wide range of structures that can be stressed, its results should be interpreted with caution. No validity or reliability studies could be located for its diagnostic validity.
Minimal data is available on the significance of the Hip Quadrant alone. However, the American College of Rheumatology provide an alternative method for the diagnosis of hip OA.
There are 2 cluster diagnoses which are:
Cluster 1:
- Pain in the hip
- <115 degrees of hip flexion
- < 15 degrees of hip IR
Cluster 2:
- Pain with hip IR
- > 60 minutes of AM stiffness
- > 50 years old[12]
If at least 4 of 5 variables were present, the positive LR was equal to 24.3 (95% confidence interval: 4.4-142.1), increasing the probability of hip OA to 91%.[12]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 ] Peter H. Seidenberg,Jimmy D. Bowen - The Hip and Pelvis in Sports Medicine and Primary Care pg. 33. Peter H. Seidenberg and Jimmy D. Bowen (editors). Springer (publisher) Evidence level: 5 grade of recommendation: F
- ↑ 2.0 2.1 2.2 Cook CE, Hegedus EJ. Orthopedic Physical Examination: An Evidence based Approach. Upper Saddle River, NJ: Pearson Prentice Hall; 2008.
- ↑ Lyle MA, Manes S, McGuinness M, Ziaei S, Iversen MD.Relationship of physical examination findings and self-reported symptom severity and physical function in patients with degenerative lumbar conditions. Phys Ther. 2005 Feb;85(2):120-33. Evidence level: 2a grade of recommendation: B
- ↑ Hip Anatomy. (2017, June 6). Physiopedia, . Retrieved 10:17, December 14, 2017 from https://www.physio-pedia.com/index.php?title=Hip_Anatomy&oldid=172875.
- ↑ Human anatomy atlas Sobotta part 2: lower extremity pg 263 – 272. Bohn Stafleu, Van Loghum 3th print R. Putz and R. Pabst
- ↑ figure 1: http://www.healthbase.com/resources/images/
- ↑ 7.0 7.1 7.2 7.3 M. Lynn Palmer – Fundamentals of musculoskeletal assessment techniques pg. 305. Second edition, M lynn palmer and Marcia E. Epler. Uppincott Williams and Willens (publisher) Evidence level: 5 grade of recommendation: F
- ↑ Manning C, Hudson Z. Comparison of hip joint range of motion in professional youth and senior team footballers with age-matched controls: an indication of early degenerative change? Phys Ther Sport. 2009 Feb;10(1):25-9. Epub 2008 Dec 24.fckLREvidence level: 3a grade of recommendation: C
- ↑ 9.0 9.1 https://www.thestudentphysicaltherapist.com/hip-quadrant-test.html
- ↑ 10.0 10.1 Thomas A. Souza Differential Diagnosis and Management for the Chiropractor: Protocols and algorithms pg 345. Fourth edition, Thomas A. Souza, DC, DACBSP. Jean and Bartlett publishers (Sanburry, Massachusetts). Evidence level: 5 grade of recommendation: F
- ↑ Mitchell B, McCrory P, Brukner P, O'Donnell J, Colson E, Howells R. Hip joint pathology: clinical presentation and correlation between magnetic resonance arthrography, ultrasound, and arthroscopic findings in 25 consecutive cases. Clin J Sport Med. 2003 May;13(3):152-6. Evidence level: 2c grade of recommendation: C
- ↑ 12.0 12.1 Altman R, Alarcon G, Appelrouth D, et al. The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum 1991: 34l 505-514.