Hip Pain and Mobility Deficits
Original Editors - Tyler Shultz
Top Contributors - Tyler Shultz, Sehriban Ozmen, Amanda Ager, Admin, Evan Thomas, Kim Jackson, Lauren Lopez, WikiSysop and Vidya Acharya
This article is currently under review and may not be up to date. Please come back soon to see the finished work! (13/02/2020)
Background[edit | edit source]
Hip pain can arise for a variety of reasons, most commonly caused by hip osteoarthritis (OA). OA is of a chronic nature, most commonly characterized as a form of chronic arthritis. This can present with joint pain, swelling, stiffness, and reduced mobility.
Risk factors include being overweight or obesity, joint injury and increasing in age. At present, there is currently no cure for OA, but there are many treatments and approaches to managing the long-term symptoms of this disease. This page will address the aspect of hip pain and associated mobility deficits.
Clinical Practice Guidelines (updated 2017)[edit | edit source]
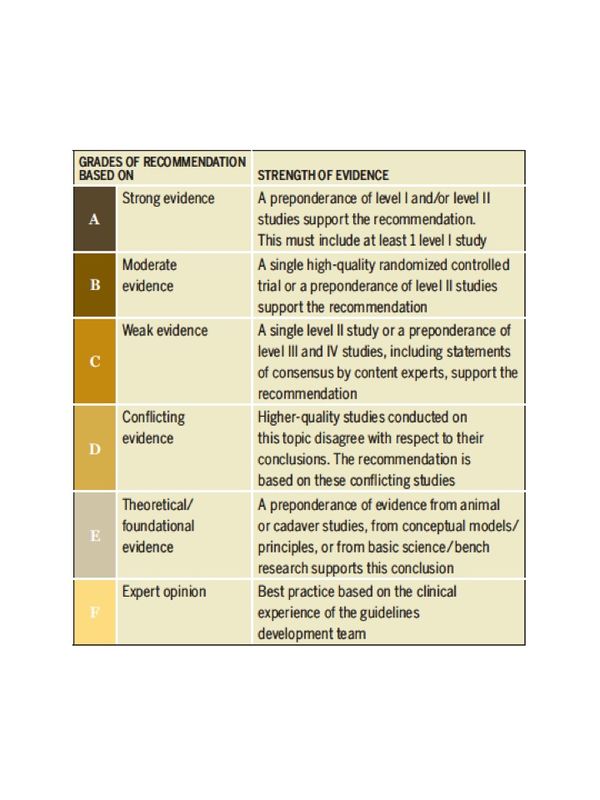
The following guidelines have been retrieved from Cibulka et al. (2017)[1]. (Table 1)
The purpose of this clinical guideline is to describe the evidence based physical therapy practice including diagnosis, prognosis, intervention and assessment of outcome for musculoskeletal disorders related to hip osteoarthritis that are commonly managed with orthopaedic physical therapy techniques.
Diagnosis & Classification Recommendations[edit | edit source]
Diagnosis/Classification (Grade: A)
Moderate anterior or lateral hip pain during weight-bearing activities, morning stiffness less than 1 hour in duration after wakening, hip internal rotation range of motion less than 24° or internal rotation and hip flexion 15° less than the nonpainful side, and/or increased hip pain associated with passive hip internal rotation.
Risk Factors (Grade: A)
Clinicians should consider the following as risk factors for hip osteoarthritis:
- Age over 50 years
- Hip developmental disorders
- History of previous hip injury
Pathoanatomical Features (Grade: B)
Clinicians should assess for impairments in mobility of the hip joint and strength of the surrounding muscles, especially the hip abductor muscles, when a patient present with hip pain.
Differential Diagnosis (Grade: F)
Clinicians should revise the diagnosis and change their plan of care, or refer the patient to the appropriate clinician, when the patient’s history, reported activity limitations, or impairments of body function and structure are not consistent with those presented in the diagnosis/classification section of this guideline, or when the patient’s symptoms are not diminishing with interventions aimed at normalization of the patient’s impairments of body function.
Examination Recommendations[edit | edit source]
Outcome Measures (Grade: A)
Clinicians should use validated outcome measures that include domains of hip pain, body function impairment, activity limitation, and participation restriction to assess outcomes of treatment of hip osteoarthritis.
Measures to assess hip pain may include the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain subscale, Brief Pain Inventory (BPI), pressure pain threshold (PPT), and pain visual analog scale (VAS).
Activity limitation and participation restriction outcome measures may include the WOMAC physical function subscale, the Hip disability and Osteoarthritis Outcome Score (HOOS), Lower Extremity Functional Scale (LEFS), and Harris Hip Score (HHS).
Activity Limitation and Participation Restriction Measures
To assess activity limitation, participation restrictions, and changes in the patient’s level of function over the episode of care, clinicians should utilize reliable and valid physical performance measures, such as the 6-minute walk test, 30-second chair stand, stair measure, timed up-and-go test, self-paced walk, timed single-leg stance, 4-square step test, and step test. (Grade: A)
Clinicians should measure balance performance and activities that predict the risk of falls in adults with hip osteoarthritis, especially those with decreased physical function or a high risk of falls because of past history. Recommended balance tests for patients with osteoarthritis include the Berg Balance Scale, 4-square step test, and timed single-leg stance test. (Grade: A)
Clinicians should use published recommendations from the Academy of Geriatric Physical Therapy of the American Physical Therapy Association6 to guide fall risk management in patients with hip osteoarthritis to assess and manage fall risk.(Grade: F)
Physical Impairment
When examining a patient with hip pain/hip osteoarthritis over an episode of care, clinicians should document the flexion, abduction, and external rotation (FABER or Patrick’s) test and passive hip range of motion and hip muscle strength, including internal rotation, external rotation, flexion, extension, abduction, and adduction. (Grade: A)
Intervention & Treatment Recommendations[edit | edit source]
Patient Education (Grade: B)
Clinicians should consider the use of patient education to teach activity modification, exercise, weight reduction when overweight, and methods of unloading the arthritic joint.
Manual Therapy (Grade: B)
Clinicians should consider the use of manual therapy procedures to provide short-term pain relief and improve hip mobility and function in patients with mild hip osteoarthritis.
Flexibility, Strengthening, and Endurance Exercise (Grade: B)
Clinicians should consider the use of flexibility, strengthening, and endurance exercises in patients with hip osteoarthritis.
Functional, Gait, and Balance Training (Grade: C)
Functional, gait, and balance training, including the use of assistive devices such as canes, crutches, and walkers, can be used in patients with hip osteoarthritis to improve function associated with weight-bearing activities.
Other Resources:[edit | edit source]
Hip Pain and Mobility Guidelines (Revision 2017): https://www.jospt.org/doi/pdf/10.2519/jospt.2017.0301
Guideline for the Management of Knee and Hip Osteoarthritis, 2nd Ed.: http://www.acsep.org.au/content/Document/guideline-for-the-management-of-knee-and-hip-oa-2nd-edition.pdf
References[edit | edit source]
- ↑ Cibulka, M,T., Bloom, N.J., Enseki, K.R., Macdonald, C.W., Woehrle, J., & McDonough, CM. (2017). Hip Pain and Mobility Deficits-Hip Osteoarthritis: Revision 2017. J Orthop Sports Phys Ther. 2017 Jun;47(6):A1-A37. doi: 10.2519/jospt.2017.0301.