Hip Pain and Mobility Deficits: Difference between revisions
Tyler Shultz (talk | contribs) No edit summary |
Kim Jackson (talk | contribs) m (Kim Jackson moved page Hip Pain & Mobility Deficits to Hip Pain and Mobility Deficits: Corrected Title) |
||
| (44 intermediate revisions by 9 users not shown) | |||
| Line 1: | Line 1: | ||
''' | <div class="editorbox"> '''Original Editor '''- [[User:Tyler Shultz|Tyler Shultz]] <br> | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | |||
== | == Introduction == | ||
Hip joint pain is a common clinical problem that can be seen in adulthood at any age or activity level. <ref name=":0">Chamberlain, R. (2021). [https://www.aafp.org/pubs/afp/issues/2021/0115/p81.html Hip pain in adults: evaluation and differential diagnosis.] ''American family physician'', ''103''(2), 81-89.</ref> The purpose of this page is to describe the evidence-based physical therapy practice including diagnosis, assessment and interventions for hip pain in adults. | |||
Hip pain can arise for a variety of reasons, most commonly caused by [[Hip Osteoarthritis|hip osteoarthritis]] (OA). Non-arthritic hip joint pain can arise due to the conditions such as [[Femoroacetabular Impingement|femoroacetabular impingement syndrome]] (FAIS), developmental [[Hip Dysplasia|dysplasia of the hip]] (DDH), hip instability, [[Labral Tear|acetabular labral tears]], osteochondral lesions, loose bodies, and ligamentum teres tears. <ref>Enseki, K. R., Bloom, N. J., Harris-Hayes, M., Cibulka, M. T., Disantis, A., Di Stasi, S., ... & Beattie, P. F. (2023). [https://www.jospt.org/doi/full/10.2519/jospt.2023.0302 Hip Pain and Movement Dysfunction Associated With Nonarthritic Hip Joint Pain: A Revision: Clinical Practice Guidelines Linked to the International Classification of Functioning, Disability, and Health from the Academy of Orthopaedic Physical Therapy and American Academy of Sports Physical Therapy of the American Physical Therapy Association.] ''Journal of Orthopaedic & Sports Physical Therapy'', (7), CPG1-CPG70.</ref> | |||
== | == Clinically Relevant Anatomy== | ||
< | [[File:Hip joint Primal.png|left|thumb|Hip joint]] | ||
The hip joint is a synovial, ball-and-socket joint between the head of the femur and the acetabulum of the pelvis. It moves in 3 different axes led by [[Functional Anatomy of the Hip-Muscles and Fascia|hip muscles]] and has inherent stability primarily caused by its bony components/articulations. (e.g.the depth of the acetabulum covers almost the entire head of the femur; the acetabular labrum, a fibrocartilaginous structure surrounding the acetabulum, deepens the hip socket and maintains negative pressure.) The joint capsule includes the [[iliofemoral ligament]], pubofemoral and ischiofemoral ligaments and they function by restricting movements. Ligamentum teres at the head of the femur acts as a carrier for the foveal artery which prevents avascular necrosis; these two structures can be injured by [[Hip Dislocation|hip dislocation]]. <ref>Gold, M., Munjal, A., & Varacallo, M. (2017). [https://www.ncbi.nlm.nih.gov/books/NBK470555/ Anatomy, bony pelvis and lower limb, hip joint].</ref><ref>Glenister, R., & Sharma, S. (2018). [https://www.ncbi.nlm.nih.gov/books/NBK526019/ Anatomy, bony pelvis and lower limb, hip].</ref> | |||
== Aetiology == | |||
Possible causes of hip joint pain according to the common pain locations are: <ref name=":0" /> | |||
=== Anterior Hip Pain === | |||
* Referred pain: From intra-abdominal or intrapelvic causes | |||
* Extra-articular: Flexor tendon | |||
* Intra-articular: [[Femoroacetabular Impingement|Femoroacetabular impingement]], [[Labral Tear|labral tear]], femoral neck stress fracture, [[Avascular Necrosis Femoral Head|avascular necrosis]], [[osteoarthritis]], [[Femoral Neck Hip Fracture|hip fracture]] | |||
=== Lateral Hip Pain === | |||
* [[Greater Trochanteric Pain Syndrome|Greater trochanteric pain syndrome]], including bursitis, gluteus medius tendinopathy or tear, external snapping, or iliotibial band friction | |||
=== Posterior Hip Pain === | |||
* Referred pain: From intra-abdominal or intrapelvic causes | |||
* [[Deep Gluteal Pain Syndrome|Deep gluteal syndrome]] | |||
* Ischiofemoral impingement | |||
* Lumbar spine or muscle | |||
* [[Sacroiliac Joint Syndrome|Sacroiliac joint pain]] | |||
* Proximal hamstring tendinopathy or tear | |||
==Diagnostic Procedures== | |||
=== Anamnesis === | |||
History taking should include: | |||
* Personal history of developmental hip dysplasia | |||
* Slipped capital femoral epiphysis | |||
* Sports activities and injuries | |||
* Family history of hip problems | |||
* Location and quality of pain | |||
* Aggravating and alleviating factors | |||
* Mechanical symptoms <ref>Wilson, J. J., & Furukawa, M. (2014). [https://www.aafp.org/pubs/afp/issues/2014/0101/p27.html Evaluation of the patient with hip pain]. ''American family physician'', ''89''(1), 27-34.</ref><ref>Kamegaya, M., Saisu, T., Nakamura, J., Murakami, R., Segawa, Y., & Wakou, M. (2011). Drehmann sign and femoro-acetabular impingement in SCFE. ''Journal of Pediatric Orthopaedics'', ''31''(8), 853-857.</ref> | |||
=== Physical Examination === | |||
* Gait analysis: Especially for [[Gait: Antalgic|antalgic]] or [[Trendelenburg Gait|Trendelenburg gait]] <ref name=":0" /> | |||
* Evaluation of the range of motion (including passive ROM) in the hip joint and associated pain <ref name=":0" /> <ref name=":1">Cibulka, M,T., Bloom, N.J., Enseki, K.R., Macdonald, C.W., Woehrle, J., & McDonough, CM. (2017). [https://www.jospt.org/doi/10.2519/jospt.2017.0301 Hip Pain and Mobility Deficits-Hip Osteoarthritis: Revision 2017]. J Orthop Sports Phys Ther. 2017 Jun;47(6):A1-A37. doi: 10.2519/jospt.2017.0301.</ref> | |||
* Strength testing of the muscles overlying the hip joint: Especially the hip abductor muscles <ref name=":0" /><ref name=":1" /> | |||
* Palpation of the painful area <ref name=":0" /> | |||
* Special tests: Flexion, abduction, and external rotation (FABER or Patrick’s) <ref name=":1" /> | |||
==Outcome Measures== | |||
Clinicians should use validated outcome measures that include domains of hip pain, body function impairment, activity limitation, and participation restriction to assess outcomes of treatment of hip osteoarthritis: | |||
* Measures to assess hip pain: Western Ontario and McMaster Universities Osteoarthritis Index ([[WOMAC Osteoarthritis Index|WOMAC]]) pain subscale, [[Brief Pain Inventory - Short Form|Brief Pain Inventory]] (BPI), pressure pain threshold (PPT), pain visual analog scale ([[Visual Analogue Scale|VAS)]]. <ref name=":1" /> | |||
* Measure to assess activity limitation and participation restriction: WOMAC physical function subscale, the Hip disability and Osteoarthritis Outcome Score (HOOS), Lower Extremity Functional Scale (LEFS), and Harris Hip Score (HHS). <ref name=":1" /> | |||
* To assess activity limitation, participation restrictions, and changes in the patient’s level of function over the episode of care, clinicians should utilize reliable and valid physical performance measures, such as the 6-minute walk test, 30-second chair stand, stair measure, timed up-and-go test, self-paced walk, timed single-leg stance, 4-square step test, and step test. | |||
* 4-square step test, timed [[Single Leg Stance Test|single-leg stance test]], and the [[Berg Balance Scale]] are also recommended to measure balance performance and activities for patients with hip OA especially those with decreased physical function or a high risk of falls because of past history. <ref name=":1" /> | |||
Recommended outcome measures at baseline and at least 1 other follow-up point for patients with with nonarthritic hip joint are listed below: | |||
* To assess the impact of impairments of body function and structure on activity limitations and participation restrictions: [[International Hip Outcome Tool (iHOT)|International Hip Outcome Tool]] (iHOT), Copenhagen Hip and Groin Outcome Score (HAGOS), [[Hip Outcome Score]] (HOS) ADL, and/or HOS Sports-Related Activities (SRA). | |||
* To assess depression, anxiety, low self-efficacy, and kinesiophobia: patient-reported outcome measure (PROM). | |||
==Management / Interventions== | |||
=== Guidelines For Hip Pain Related To [[Hip Osteoarthritis]] === | |||
=== '''Patient Education''' === | |||
Clinicians should provide patient education combined with exercise and/or manual therapy. Education should include teaching activity modification, exercise, supporting weight reduction when overweight, and methods of unloading the arthritic joints. '''(Grade: B)''' | |||
==== '''Manual Therapy''' ==== | |||
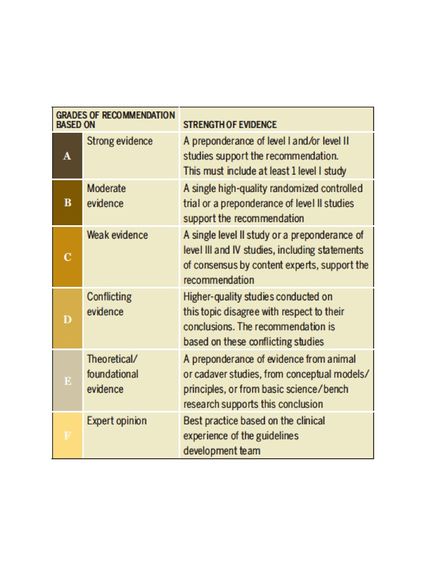
Clinicians should use manual therapy for patients with mild to moderate hip osteoarthritis and impairment of joint mobility, flexibility, and/or pain. Manual therapy may include thrust, nonthrust, and soft tissue mobilization. Doses and duration may range from 1 to 3 times per week over 6 to 12 weeks in patients with mild to moderate hip osteoarthritis. As hip motion improves, clinicians should add exercises including stretching and strengthening to augment and sustain gains in the patient’s range of motion, flexibility, and strength. '''(Grade: A)'''[[File:Levels of Evidence.jpg|570x570px|thumb|Table 1<ref name=":2">Cibulka, M,T., Bloom, N.J., Enseki, K.R., Macdonald, C.W., Woehrle, J., & McDonough, CM. (2017). [https://www.jospt.org/doi/10.2519/jospt.2017.0301 Hip Pain and Mobility Deficits-Hip Osteoarthritis: Revision 2017]. J Orthop Sports Phys Ther. 2017 Jun;47(6):A1-A37. doi: 10.2519/jospt.2017.0301.</ref>]] | |||
==== '''Flexibility, Strengthening, and Endurance Exercise''' ==== | |||
Clinicians should use individualized flexibility, strengthening, and endurance exercises to address impairments in hip range of motion, specific muscle weaknesses, and limited thigh (hip) muscle flexibility. For group-based exercise programs, effort should be made to tailor exercises to address patients’ most relevant physical impairments. Dosage and duration of treatment for effect should range from 1 to 5 times per week over 6 to 12 weeks in patients with mild to moderate hip osteoarthritis. '''(Grade: B)''' | |||
==== '''Functional, Gait, and Balance Training''' ==== | |||
Clinicians should provide impairment-based functional, gait, and balance training, including the proper use of assistive devices (canes, crutches, walkers), to patients with hip osteoarthritis and activity limitations, balance impairment, and/or gait limitations when associated problems are observed and documented during the history or physical assessment of the patient. '''(Grade: C)''' | |||
Clinicians should individualize prescription of therapeutic activities based on the patient’s values, daily life participation, and functional activity needs. '''(Grade: C)''' | |||
==== '''Modalities''' ==== | |||
Clinicians may use ultrasound (1 MHz; 1 W/cm2 for 5 minutes each to the anterior, lateral, and posterior hip for a total of 10 treatments over a 2-week period) in addition to exercise and hot packs in the short-term management of pain and activity limitation in individuals with hip osteoarthritis. '''(Grade: B)''' | |||
==== '''Bracing''' ==== | |||
Clinicians should not use bracing as a first line of treatment. A brace may be used after exercise or manual therapies are unsuccessful in improving participation in activities that require turning/pivoting for patients with mild to moderate hip osteoarthritis, especially in those with bilateral hip osteoarthritis.'''(Grade: F)''' | |||
==== '''Weight Loss''' ==== | |||
In addition to providing exercise intervention, clinicians should collaborate with physicians, nutritionists, or dietitians to support weight reduction in individuals with hip osteoarthritis who are overweight or obese. '''(Grade: C)''' | |||
== Differential Diagnosis == | |||
* [[Femoroacetabular Impingement]]: Young, athletic patient, gradual onset, pain with hip range of motion, history of slipped capital femoral epiphysis or [[Developmental dysplasia of the hip (DDH)|developmental dysplasia]], positive FABER test result <ref name=":0" /> | |||
* [[Avascular Necrosis Femoral Head|Avascular necrosis]]: Middle or older age, smoking, alcohol use, systemic corticosteroid use, hemoglobinopathies, chemotherapy, metabolic syndrome, and obesity. [[Gait: Antalgic|Antalgic gait]], pain with range of motion, limited range of motion. <ref name=":0" /> | |||
* [[Hip Osteoarthritis|Hip osteoarthritis]]: Moderate anterior or lateral hip pain during weight-bearing activities, morning stiffness less than 1 hour in duration after wakening, hip internal rotation range of motion less than 24° or internal rotation and hip flexion 15° less than the nonpainful side, and/or increased hip pain associated with passive hip internal rotation. <ref name=":2" /> | |||
* [[Femoral Neck Hip Fracture|Hip fracture]]: Older age, [[osteoporosis]], fall/trauma, inability to walk on the affected limb, shortened, externally rotated, abducted leg. <ref name=":0" /> | |||
* [[Greater Trochanteric Pain Syndrome|Greater trochanteric pain syndrome]]: No injury, middle age, female sex, overweight, pain with sleeping on affected hip, pain aggravated by physical activity or sitting for long periods, tenderness to palpation over the lateral hip/ greater trochanter, Trendelenburg gait or positive [[Trendelenburg Sign|Trendelenburg]] test, positive resisted external derotation test. <ref name=":0" /> | |||
* [[Deep Gluteal Pain Syndrome|Deep gluteal syndrome:]] Deep buttock pain, no injury, worse with sitting (especially in a car), sciatica (burning pain shooting down the leg) <ref name=":0" /> | |||
* Ischiofemoral impingement: Gradual onset of deep buttock pain that worsens with activities requiring a long stride (e.g., running). <ref name=":0" /> | |||
* [[Sacroiliac Joint Syndrome|Sacroiliac joint pain]]: No history of lumbar spinal issues, tenderness over the sacroiliac joint, no tenderness above L5. <ref name=":0" /> | |||
* Proximal hamstring tendinopathy or tear: Overuse injury with hip extension activities (vs. acute injury with forceful hip extension), tenderness to palpation over the ischial tuberosity, pain with hamstring strength testing, acute tears cause ecchymosis of the posterior thigh. <ref name=":0" /> | |||
==Resources == | |||
* Hip Pain and Mobility Guidelines (Revision 2017): https://www.jospt.org/doi/pdf/10.2519/jospt.2017.0301 | |||
* Guideline for the Management of Knee and Hip Osteoarthritis, 2nd Ed.: http://www.acsep.org.au/content/Document/guideline-for-the-management-of-knee-and-hip-oa-2nd-edition.pdf | |||
* Management of Falls in Community-Dwelling Older Adults: Clinical Guidance Statement From the Academy of Geriatric Physical Therapy of the American Physical Therapy Association: https://academic.oup.com/ptj/article/95/6/815/2686335?login=false | |||
== References == | |||
<references /> | <references /> | ||
[[Category: | [[Category:Interventions]] | ||
[[Category:Hip - Interventions]] | |||
[[Category:Clinical_Guidelines]] | |||
[[Category:Hip - Guidelines]] | |||
[[Category:Hip]] | |||
[[Category:Osteoarthritis]] | |||
[[Category:EBP]] | |||
[[Category:Musculoskeletal/Orthopaedics]] | |||
[[Category:Older People/Geriatrics]] | |||
[[Category:Older People/Geriatrics - Conditions]] | |||
Latest revision as of 11:25, 24 July 2023
Top Contributors - Tyler Shultz, Sehriban Ozmen, Amanda Ager, Admin, Evan Thomas, Kim Jackson, Lauren Lopez, WikiSysop and Vidya Acharya
Introduction[edit | edit source]
Hip joint pain is a common clinical problem that can be seen in adulthood at any age or activity level. [1] The purpose of this page is to describe the evidence-based physical therapy practice including diagnosis, assessment and interventions for hip pain in adults.
Hip pain can arise for a variety of reasons, most commonly caused by hip osteoarthritis (OA). Non-arthritic hip joint pain can arise due to the conditions such as femoroacetabular impingement syndrome (FAIS), developmental dysplasia of the hip (DDH), hip instability, acetabular labral tears, osteochondral lesions, loose bodies, and ligamentum teres tears. [2]
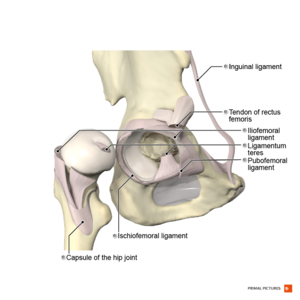
Clinically Relevant Anatomy[edit | edit source]
The hip joint is a synovial, ball-and-socket joint between the head of the femur and the acetabulum of the pelvis. It moves in 3 different axes led by hip muscles and has inherent stability primarily caused by its bony components/articulations. (e.g.the depth of the acetabulum covers almost the entire head of the femur; the acetabular labrum, a fibrocartilaginous structure surrounding the acetabulum, deepens the hip socket and maintains negative pressure.) The joint capsule includes the iliofemoral ligament, pubofemoral and ischiofemoral ligaments and they function by restricting movements. Ligamentum teres at the head of the femur acts as a carrier for the foveal artery which prevents avascular necrosis; these two structures can be injured by hip dislocation. [3][4]
Aetiology[edit | edit source]
Possible causes of hip joint pain according to the common pain locations are: [1]
Anterior Hip Pain[edit | edit source]
- Referred pain: From intra-abdominal or intrapelvic causes
- Extra-articular: Flexor tendon
- Intra-articular: Femoroacetabular impingement, labral tear, femoral neck stress fracture, avascular necrosis, osteoarthritis, hip fracture
Lateral Hip Pain[edit | edit source]
- Greater trochanteric pain syndrome, including bursitis, gluteus medius tendinopathy or tear, external snapping, or iliotibial band friction
Posterior Hip Pain[edit | edit source]
- Referred pain: From intra-abdominal or intrapelvic causes
- Deep gluteal syndrome
- Ischiofemoral impingement
- Lumbar spine or muscle
- Sacroiliac joint pain
- Proximal hamstring tendinopathy or tear
Diagnostic Procedures[edit | edit source]
Anamnesis[edit | edit source]
History taking should include:
- Personal history of developmental hip dysplasia
- Slipped capital femoral epiphysis
- Sports activities and injuries
- Family history of hip problems
- Location and quality of pain
- Aggravating and alleviating factors
- Mechanical symptoms [5][6]
Physical Examination[edit | edit source]
- Gait analysis: Especially for antalgic or Trendelenburg gait [1]
- Evaluation of the range of motion (including passive ROM) in the hip joint and associated pain [1] [7]
- Strength testing of the muscles overlying the hip joint: Especially the hip abductor muscles [1][7]
- Palpation of the painful area [1]
- Special tests: Flexion, abduction, and external rotation (FABER or Patrick’s) [7]
Outcome Measures[edit | edit source]
Clinicians should use validated outcome measures that include domains of hip pain, body function impairment, activity limitation, and participation restriction to assess outcomes of treatment of hip osteoarthritis:
- Measures to assess hip pain: Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain subscale, Brief Pain Inventory (BPI), pressure pain threshold (PPT), pain visual analog scale (VAS). [7]
- Measure to assess activity limitation and participation restriction: WOMAC physical function subscale, the Hip disability and Osteoarthritis Outcome Score (HOOS), Lower Extremity Functional Scale (LEFS), and Harris Hip Score (HHS). [7]
- To assess activity limitation, participation restrictions, and changes in the patient’s level of function over the episode of care, clinicians should utilize reliable and valid physical performance measures, such as the 6-minute walk test, 30-second chair stand, stair measure, timed up-and-go test, self-paced walk, timed single-leg stance, 4-square step test, and step test.
- 4-square step test, timed single-leg stance test, and the Berg Balance Scale are also recommended to measure balance performance and activities for patients with hip OA especially those with decreased physical function or a high risk of falls because of past history. [7]
Recommended outcome measures at baseline and at least 1 other follow-up point for patients with with nonarthritic hip joint are listed below:
- To assess the impact of impairments of body function and structure on activity limitations and participation restrictions: International Hip Outcome Tool (iHOT), Copenhagen Hip and Groin Outcome Score (HAGOS), Hip Outcome Score (HOS) ADL, and/or HOS Sports-Related Activities (SRA).
- To assess depression, anxiety, low self-efficacy, and kinesiophobia: patient-reported outcome measure (PROM).
Management / Interventions[edit | edit source]
Guidelines For Hip Pain Related To Hip Osteoarthritis[edit | edit source]
Patient Education[edit | edit source]
Clinicians should provide patient education combined with exercise and/or manual therapy. Education should include teaching activity modification, exercise, supporting weight reduction when overweight, and methods of unloading the arthritic joints. (Grade: B)
Manual Therapy[edit | edit source]
Clinicians should use manual therapy for patients with mild to moderate hip osteoarthritis and impairment of joint mobility, flexibility, and/or pain. Manual therapy may include thrust, nonthrust, and soft tissue mobilization. Doses and duration may range from 1 to 3 times per week over 6 to 12 weeks in patients with mild to moderate hip osteoarthritis. As hip motion improves, clinicians should add exercises including stretching and strengthening to augment and sustain gains in the patient’s range of motion, flexibility, and strength. (Grade: A)
Flexibility, Strengthening, and Endurance Exercise[edit | edit source]
Clinicians should use individualized flexibility, strengthening, and endurance exercises to address impairments in hip range of motion, specific muscle weaknesses, and limited thigh (hip) muscle flexibility. For group-based exercise programs, effort should be made to tailor exercises to address patients’ most relevant physical impairments. Dosage and duration of treatment for effect should range from 1 to 5 times per week over 6 to 12 weeks in patients with mild to moderate hip osteoarthritis. (Grade: B)
Functional, Gait, and Balance Training[edit | edit source]
Clinicians should provide impairment-based functional, gait, and balance training, including the proper use of assistive devices (canes, crutches, walkers), to patients with hip osteoarthritis and activity limitations, balance impairment, and/or gait limitations when associated problems are observed and documented during the history or physical assessment of the patient. (Grade: C)
Clinicians should individualize prescription of therapeutic activities based on the patient’s values, daily life participation, and functional activity needs. (Grade: C)
Modalities[edit | edit source]
Clinicians may use ultrasound (1 MHz; 1 W/cm2 for 5 minutes each to the anterior, lateral, and posterior hip for a total of 10 treatments over a 2-week period) in addition to exercise and hot packs in the short-term management of pain and activity limitation in individuals with hip osteoarthritis. (Grade: B)
Bracing[edit | edit source]
Clinicians should not use bracing as a first line of treatment. A brace may be used after exercise or manual therapies are unsuccessful in improving participation in activities that require turning/pivoting for patients with mild to moderate hip osteoarthritis, especially in those with bilateral hip osteoarthritis.(Grade: F)
Weight Loss[edit | edit source]
In addition to providing exercise intervention, clinicians should collaborate with physicians, nutritionists, or dietitians to support weight reduction in individuals with hip osteoarthritis who are overweight or obese. (Grade: C)
Differential Diagnosis[edit | edit source]
- Femoroacetabular Impingement: Young, athletic patient, gradual onset, pain with hip range of motion, history of slipped capital femoral epiphysis or developmental dysplasia, positive FABER test result [1]
- Avascular necrosis: Middle or older age, smoking, alcohol use, systemic corticosteroid use, hemoglobinopathies, chemotherapy, metabolic syndrome, and obesity. Antalgic gait, pain with range of motion, limited range of motion. [1]
- Hip osteoarthritis: Moderate anterior or lateral hip pain during weight-bearing activities, morning stiffness less than 1 hour in duration after wakening, hip internal rotation range of motion less than 24° or internal rotation and hip flexion 15° less than the nonpainful side, and/or increased hip pain associated with passive hip internal rotation. [8]
- Hip fracture: Older age, osteoporosis, fall/trauma, inability to walk on the affected limb, shortened, externally rotated, abducted leg. [1]
- Greater trochanteric pain syndrome: No injury, middle age, female sex, overweight, pain with sleeping on affected hip, pain aggravated by physical activity or sitting for long periods, tenderness to palpation over the lateral hip/ greater trochanter, Trendelenburg gait or positive Trendelenburg test, positive resisted external derotation test. [1]
- Deep gluteal syndrome: Deep buttock pain, no injury, worse with sitting (especially in a car), sciatica (burning pain shooting down the leg) [1]
- Ischiofemoral impingement: Gradual onset of deep buttock pain that worsens with activities requiring a long stride (e.g., running). [1]
- Sacroiliac joint pain: No history of lumbar spinal issues, tenderness over the sacroiliac joint, no tenderness above L5. [1]
- Proximal hamstring tendinopathy or tear: Overuse injury with hip extension activities (vs. acute injury with forceful hip extension), tenderness to palpation over the ischial tuberosity, pain with hamstring strength testing, acute tears cause ecchymosis of the posterior thigh. [1]
Resources[edit | edit source]
- Hip Pain and Mobility Guidelines (Revision 2017): https://www.jospt.org/doi/pdf/10.2519/jospt.2017.0301
- Guideline for the Management of Knee and Hip Osteoarthritis, 2nd Ed.: http://www.acsep.org.au/content/Document/guideline-for-the-management-of-knee-and-hip-oa-2nd-edition.pdf
- Management of Falls in Community-Dwelling Older Adults: Clinical Guidance Statement From the Academy of Geriatric Physical Therapy of the American Physical Therapy Association: https://academic.oup.com/ptj/article/95/6/815/2686335?login=false
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 Chamberlain, R. (2021). Hip pain in adults: evaluation and differential diagnosis. American family physician, 103(2), 81-89.
- ↑ Enseki, K. R., Bloom, N. J., Harris-Hayes, M., Cibulka, M. T., Disantis, A., Di Stasi, S., ... & Beattie, P. F. (2023). Hip Pain and Movement Dysfunction Associated With Nonarthritic Hip Joint Pain: A Revision: Clinical Practice Guidelines Linked to the International Classification of Functioning, Disability, and Health from the Academy of Orthopaedic Physical Therapy and American Academy of Sports Physical Therapy of the American Physical Therapy Association. Journal of Orthopaedic & Sports Physical Therapy, (7), CPG1-CPG70.
- ↑ Gold, M., Munjal, A., & Varacallo, M. (2017). Anatomy, bony pelvis and lower limb, hip joint.
- ↑ Glenister, R., & Sharma, S. (2018). Anatomy, bony pelvis and lower limb, hip.
- ↑ Wilson, J. J., & Furukawa, M. (2014). Evaluation of the patient with hip pain. American family physician, 89(1), 27-34.
- ↑ Kamegaya, M., Saisu, T., Nakamura, J., Murakami, R., Segawa, Y., & Wakou, M. (2011). Drehmann sign and femoro-acetabular impingement in SCFE. Journal of Pediatric Orthopaedics, 31(8), 853-857.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 Cibulka, M,T., Bloom, N.J., Enseki, K.R., Macdonald, C.W., Woehrle, J., & McDonough, CM. (2017). Hip Pain and Mobility Deficits-Hip Osteoarthritis: Revision 2017. J Orthop Sports Phys Ther. 2017 Jun;47(6):A1-A37. doi: 10.2519/jospt.2017.0301.
- ↑ 8.0 8.1 Cibulka, M,T., Bloom, N.J., Enseki, K.R., Macdonald, C.W., Woehrle, J., & McDonough, CM. (2017). Hip Pain and Mobility Deficits-Hip Osteoarthritis: Revision 2017. J Orthop Sports Phys Ther. 2017 Jun;47(6):A1-A37. doi: 10.2519/jospt.2017.0301.