Hip Osteoarthritis: Difference between revisions
Scott Buxton (talk | contribs) mNo edit summary |
Scott Buxton (talk | contribs) mNo edit summary |
||
| Line 33: | Line 33: | ||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
The most important characteristic of hip osteoarthritis is that there’s damage to or loss of the articular cartilage | The most important characteristic of hip osteoarthritis is that there’s damage to or loss of the articular cartilage<ref>Book: CRIELAARD J.M., DEQUEKER J., FAMAEY J.P., FRANCHIMONG P., GRITTEN Ch., HUAUX J.P. et al. ‘Osteoartrose’. Brussel, België: drukkerij Lichtert; maart 1985.</ref>. Another typical characteristic is pain, especially pain that starts when the patient starts moving. This pain decreases when the patient keeps on moving or increases when they load the joint for too long or the wrong way. Later on, they will typically complain of a continuous pain and night pain.<ref>Book: CRIELAARD J.M., DEQUEKER J., FAMAEY J.P., FRANCHIMONG P., GRITTEN Ch., HUAUX J.P. et al. ‘Osteoartrose’. Brussel, België: drukkerij Lichtert; maart 1985.</ref> (Level of evidence: A1) | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
Revision as of 14:33, 18 June 2013
Original Editors - Eric Robertson, Kim Presiaux
Top Contributors - Kim Presiaux, Dorien De Strijcker, Lucinda hampton, Davy Duverger, Leana Louw, Kim Jackson, Laura Ritchie, Johnathan Fahrner, Admin, Rachael Lowe, Scott Buxton, Van Horebeek Erika, Vidya Acharya, Kai A. Sigel, Eric Robertson, Areeba Raja, Loïc Byl, Marius De Bruyn, Kevin Vandebroucq, 127.0.0.1, Bram Van Roost, Shaimaa Eldib and Lauren Lopez Read more.Definition/Description[edit | edit source]
Hip osteoarthritis is a common type of osteoarthritis. Since the hip is a weight-bearing joint, osteoarthritis can cause significant problems. Hip osteoarthritis is caused by deterioration of the articular cartilage of the hip joint.
There are several risk factors[1]: (Level of evidence: A1)
- Previous hip injury
- Previous fracture, which changes hip alignment
- Genetics
- Congenital and developmental hip disease
- Subchondral bone that is too soft or too hard
- Overweight
- Occupation
- Age
- Gender
- Sport
- Menopause
- Sedentary Lifestyle
Clinically Relevant Anatomy[edit | edit source]
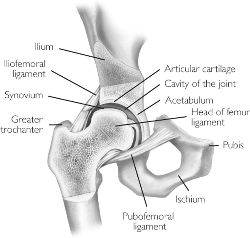
The anatomy of the hip joint is complex and more in-depth information can be found with the link provided. In summary, the hip is a synovial ball and socket joint, with the convex femoral head articulating with the concave acetabulum. Stability of the joint is achieved through a combination of muscle action and several ligaments forming a loose, but strong joint capsule. Ligaments like the iliofemoral ligament, the ischialfemoral ligament and the pubofemoral ligament keep the femoral head had at his place, in the acetabulum. Another ligament, the ligamentum teres, does not provide stability to the hip but offers a portion of blood supply to the femoral head in some individuals.
The femoral head and acetablum are covered by smooth hyaline cartilage, and the acetabulum contains a labrum, which functions to facilitate movement and support the forces passed through the joint.
The hip, despite the requirement to support the weight of the body, has the second largest excursion of motion of any joint in the body.
External Link: [Hip Anatomy Video]
Characteristics/Clinical Presentation[edit | edit source]
The most important characteristic of hip osteoarthritis is that there’s damage to or loss of the articular cartilage[2]. Another typical characteristic is pain, especially pain that starts when the patient starts moving. This pain decreases when the patient keeps on moving or increases when they load the joint for too long or the wrong way. Later on, they will typically complain of a continuous pain and night pain.[3] (Level of evidence: A1)
Differential Diagnosis[edit | edit source]
A thorough patient history and physical examination should aid the clinican in his/her differential diagnosis. Pain location is often a good indicator of intraarticular versus extraarticular disorders. [4] The clinician should differentiate between a multitude of conditions such as: contusions, strains, athletic pubalgia, piriformis syndrome, hamstring syndrome, inflammatory disorders, snapping hip syndrome, bursitis, arthritis, septic arthritis, osteonecrosis, labral tears, fractures and dislocations, and tumors. [4]
Diagnostic Procedures[edit | edit source]
Altman et al. have established guidelines by which clinical diagnosis of hip osteoarthritis can be made. The guidelines, established in 1991, present a 3 pronged approach to diagnosis of hip osteoarthritis including clinical, radiological, and laboratory findings. According to these guidlelines, a patient was considered to have osteoarthritis if they presented with:
- Hip Pain
AND - Hip Internal Rotation ≤ 15 °
Hip Flexion ≤ 115°
OR:
Hip pain and:
- Hip Rotation ≥ 15°
Or : - Pain with Hip Internal Rotation
Or: - Hip stiffness in the AM ≤ 60 minutes
Or: - Age > 50 years
More recently, Sutlive et al. [5] have proposed a clinical prediction rule to identify individuals with hip osteoarthritis presenting with unilateral hip pain. (Level of evidence: A2) This clinical prediction rule is to detect OA in patients with unilateral hip pain.By this way, it assists clinicians in determining which patients require further testing and evaluation, and when to initiate early management, which may minimize the deleterious effects of hip OA and maximize function. This clinical prediction rule is based on 5 predictor variables. If a subject exhibited only 1 or 2 of the predictor variables, the posttest probability of having hip OA only increased from 29% to 33% and 46%, respectively.However, if a subject had at least 3 predictors present, the likelihood of having
hip OA increased from 29% to 68%. If a subject exhibited at least 4 of the 5 predictors, the posttest probability increased further to 91%.
The five predictor variables are:
- Flexion (involved side)
- Internal rotation (involved side)
- Scour test (involved side)
- Patrick’s test (involved side)
- Hip flexion test (involved side)
Outcome Measures[edit | edit source]
Hip Disability and Osteoarthritis Outcome Score
Examination[edit | edit source]
The beginning of OA is characterized by limited abduction and rotation in the hip joint. Later on flexion, extension, and adduction become more difficult.
Physiotherapeutic examination [6]
1) Palpation of M. gluteus medius.
Position: patient lies on his side. Upper leg in adduction and flexion
OA: Zone of greater Trochanter is sensitive and painful.
2)Flexion and forced flexion
Position: patient lies on his back.
OA: Flexion is limited.
3) Extension Position: Patient in prone.
Physiotherapist stabilizes the pelvis and raises the leg.
OA: Amplitude is limited.
4) Abduction and adduction
Position: Patient lies on his back. Physiotherapist stabilizes the pelvis and performs abduction and adduction.
OA: abduction is limited, adduction keeps normal amplitude.
Medical Management
[edit | edit source]
http://www.guidelines.gov/content.aspx?id=36893
Physical Therapy Management
[edit | edit source]
Treatment goals: improve strength, coordination, mobility, balance, stand, stability, flexibility. Reduce pain.
USUAL CARE
Activation of the circulatory:[6] (Level of evidence: A1) Massage and heat therapy (radioation, conductien or conversion) can cause a better blood circulation near the skin, subcutaneous, muscles, tendons, capsules and ligaments. Passive exercises[7]
- Positions patient: supine, hip in 15-30° flexion, 15-30° AB, slight ER
Physiotherapist: perform 3-6 thrusts at the beginning of the first set then perform oscillations.
- Positions patient: supine with hip flexed
Physiotherapist: oscillatory passive mobilizations, applied caudally or laterally to the proximal thigh
- Position patient: Prone with knee flexed.
Physiotherapist: IR until contralateral pelvis rises, apply oscillatory force downwards to contralateral pelvis
- Firm effleurage stroke, deep frictions or sustained pressure trigger point release with the muscle on stretch.
Position patient: Prone. The hip is in 10-15 ° AB.
Physiotherapist: Perform caudally directed oscillations. May perform 3-6 thrusts at the beginning of the first set.
- Position patient: Supine with hip in flexion and adduction.
Physiotherapist: Use body weight to impart passive oscillations to the postero-lateral hip capsule through the long axis of the femur. Add more flexion, adduction, and/or internal rotation to progress.
- Massage of quads, hamstrings, psoas, adductors, abductors, gluteus-muscles
Active exercises
- Knee to chest exercise (strengthens the abdominal muscles and improves the flexibility of the hip, back and neck) Patient lies on the floor with left leg straight and right foot flat on the floor. Grabs his knee and bring it toward to his chest, holds for 30seconds and switches legs.
- Bridging exercise ( strengthens buttock abdominal and hamstrings muscles) Patient lies on his back with knees bent and feet flat on the floor. While tightening abdominal muscles he lifts his pelvis slightly upwards. Hold for 15-20 seconds. Repeat 8-12 times.
- Balance exercises [7]
( Standing weight shifting forwards/ lateral, Standing in double leg stance on foam, Shuttle walking, Stairs)
- Endurance exercises
Walk, cycle, swim
Aquatherapy[6] (Level of evidence: A1) Passive and active mobilization could be done in water as well, by an indifferent temperature (35 degrees), in order to facilitaite recovery of the motorfuntion. In this situation, gravity is greatly reduced thus the burdensome weight and tension at the height of the effected joint will be reduced as well. Advice and education is important in treatment, tell the patient about their condition. Why does it occur? What's the treatment? What's the importance of exercise? This will make the patient have a clear understanding in his condition and will improve the healing process.[7] It’s also very important to tell the patient what they can and can not do. Behavioral graded activities (BGA) is an kind of treatment that contains normal exercise therapy comprising booster sessions. The long term effectiveness has been shown, but it is unclear whether this treatment has a better efficacy than usual care.[8] BGA intervention consists of 3 phases:[9]
- Starting phase: The physiotherapist will educate the patient about his condition. And there will be made a list of treatment goals and problematic activities.
- Treatment phase: increasingly difficult exercises.
- Integration phase: The physiotherapist will support and integrate behavioral changes.
Key Research[edit | edit source]
Hoeksma HL, Dekker J, Ronday HK, Heering A, van der Lubbe N, Vel C, Breedveld FC, van den Ende CH. Comparison of manual therapy and exercise therapy in osteoarthritis of the hip: a randomized clinical trial. Arthritis Rheum. 2004 Oct 15;51(5):722-9.
Peter WF, Jansen MJ, Hurkmans EJ, Bloo H, Dekker J, Dilling RG, Hilberdink W, Kersten-Smit C, de Rooij M, Veenhof C, Vermeulen HM, de Vos RJ, Schoones JW, Vliet Vlieland TP; Guideline Steering Committee - Hip and Knee Osteoarthritis. Physiotherapy in hip and knee osteoarthritis: development of a practice guideline concerning initial assessment, treatment and evaluation. Acta Reumatol Port. 2011 Jul-Sep;36(3):268-81.
French HP, Cusack T, Brennan A, Caffrey A, Conroy R, Cuddy V, FitzGerald OM, Gilsenan C, Kane D, O'Connell PG, White B, McCarthy GM Exercise and manual physiotherapy arthritis research trial (EMPART) for osteoarthritis of the hip: a multicenter randomized controlled trial. Arch Phys Med Rehabil. 2013 Feb;94(2):302-14. doi: 10.1016/j.apmr.2012.09.030
Abbott JH, Robertson MC, Chapple C, Pinto D, Wright AA, Leon de la Barra S, Baxter GD, Theis JC, Campbell AJ; MOA Trial team. Manual therapy, exercise therapy, or both, in addition to usual care, for osteoarthritis of the hip or knee: a randomized controlled trial. 1: clinical effectiveness. Osteoarthritis Cartilage. 2013 Apr;21(4):525-34. doi: 10.1016/j.joca.2012.12.014.
Resources
[edit | edit source]
http://www.guidelines.gov/content.aspx?id=36893
Clinical Bottom Line[edit | edit source]
Depending on the severity of the condition, managment will vary from patient to patient. It is important that the clinician individualizes treatment to each of their patients in order to ensure optimal outcomes.
Recent Related Research (from Pubmed)
[edit | edit source]
References[edit | edit source]
- ↑ Book: REGINSTER et al. 'Osteoarthritis. Clinical and Experimental Aspects'. Springer, Verlag Berlin Heiderlberg, 1999.
- ↑ Book: CRIELAARD J.M., DEQUEKER J., FAMAEY J.P., FRANCHIMONG P., GRITTEN Ch., HUAUX J.P. et al. ‘Osteoartrose’. Brussel, België: drukkerij Lichtert; maart 1985.
- ↑ Book: CRIELAARD J.M., DEQUEKER J., FAMAEY J.P., FRANCHIMONG P., GRITTEN Ch., HUAUX J.P. et al. ‘Osteoartrose’. Brussel, België: drukkerij Lichtert; maart 1985.
- ↑ 4.0 4.1 DeAngelis NA, Busconi BD. Assessment and differential diagnosis of the painful hip. Clinical Orthopaedics. 2003;406:11-18.
- ↑ SUTLIVE et al. 'Development of a Clinical Prediction Rule for Diagnosing Hip Osteoarthritis in Individuals With Unilateral Hip Pain'. J Orthop Sports Phys Ther.: September 2008;38(9):542-50.
- ↑ 6.0 6.1 6.2 CRIELAND, e.a., Osteoartrose, Lichtert, Brussel, 1985 Cite error: Invalid
<ref>tag; name "Crieland" defined multiple times with different content - ↑ 7.0 7.1 7.2 ) Kim L Bennell, Thorlene Egerton, Yong-Hao Pua, J Haxby Abbott, Kevin Sims, Ben Metcalf, Fiona McManus, Tim V Wrigley, Andrew Forbes, Anthony Harris, Rachelle Buchbinder, “EFFICACY OF A MULTIMODAL PHYSIOTHERAPY TREATMENT PROGRAM FOR HIP OSTEOARTHRITIS: A RANDOMISED PLACEBO-CONTROLLED TRIAL PROTOCOL”, 2010, BMC musculoskeletal disorder.
- ↑ cindy veenhof, albère j. a. köke, joost dekker, rob a. oostendorp, johannes w. j. bijlsma, maurits w. van tulder, and cornelia h. m. van den ende, "EFFECTIVENESS OF BEHAVIORAL GRADED ACTIVITY IN PATIENTS WITH OSTEOARTHRITIS OF THE HIP AND/OR KNEE: A RANDOMIZED CLINICAL TRIAL", 2006, Arthritis &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Rheumatism
- ↑ M.F. Pister, C. Veenhof, F.G. Schellevis, D.H. De Bakker, J. Dekker, "LONG-TERM EFFECTIVENESS OF EXERCISE THERAPY IN PATIENTS WITH OSTEOARTHRITIS OF THE HIP OR KNEE: A RANDOMIZED CONTROLLED TRIAL COMPARING TWO DIFFERENT PHYSICAL THERAPY INTERVENTIONS", Osteoarthritis and Cartilage, 2010
see adding references tutorial. </div>