Hip Labral Disorders: Difference between revisions
Kim Jackson (talk | contribs) mNo edit summary |
No edit summary |
||
| (10 intermediate revisions by 6 users not shown) | |||
| Line 6: | Line 6: | ||
== Introduction == | == Introduction == | ||
Disorders of the hip labrum is an umbrella term that includes any issues involving that labrum such as [[Femoroacetabular Impingement|femoroacetabular impingement]] (aka FAI) and acetabular labral tear (ALT). This mechanically induced pathology is thought to result from excessive forces at the hip joint. For example, a tear could decrease the acetabular contact area and increase stress, | Disorders of the hip labrum is an umbrella term that includes any issues involving that labrum such as [[Femoroacetabular Impingement|femoroacetabular impingement]] (aka FAI) and acetabular labral tear (ALT). This mechanically induced pathology is thought to result from excessive forces at the hip joint. For example, a tear could decrease the acetabular contact area and increase stress, resulting in articular damage and destabilising the hip joint.<ref name=":4" /> Amber and Mohan (2018) proposed that the term "fissure" is a better alternative to labral tears, at least in patients over the age of 40, to prevent overdiagnosis and unnecessary medical intervention.<ref>Amber I, Mohan S. Preventing Overdiagnosis of Acetabular Labral "Tears" in 40-Plus-year-old Patients: Shouldn't these be called Labral "Fissures" Instead? Acad Radiol. 2018;25(3):387-390. | ||
</ref> | </ref> | ||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
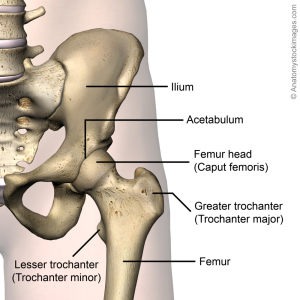
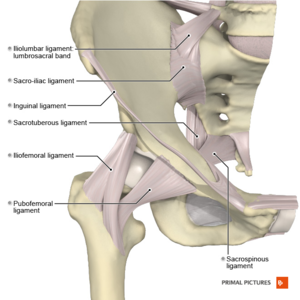
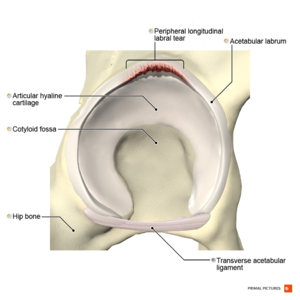
The hip (acetabulofemoral joint) is a synovial joint formed between the femur and acetabulum of the pelvis. The head of the femur is covered by Type II collagen (hyaline cartilage) and proteoglycan. The acetabulum is the concave portion of the ball and socket joint. The acetabulum has a ring of fibrocartilage called the labrum that deepens the acetabulum and improves stability of the hip joint. For a more detailed review of the anatomy of the hip, please see the [[Hip Anatomy]] article. | The hip (acetabulofemoral joint) is a synovial joint formed between the femur and acetabulum of the pelvis. The head of the femur is covered by Type II collagen (hyaline cartilage) and proteoglycan. The acetabulum is the concave portion of the ball and socket joint. The acetabulum has a ring of fibrocartilage called the labrum that deepens the acetabulum and improves the stability of the hip joint. For a more detailed review of the anatomy of the hip, please see the [[Hip Anatomy]] article. | ||
<div class="row"> | <div class="row"> | ||
| Line 21: | Line 21: | ||
== Epidemiology/Aetiology == | == Epidemiology/Aetiology == | ||
The labrum of the hip is susceptible to traumatic injury from the shearing forces that occur with twisting, pivoting and falling. Direct trauma (e.g. motor vehicle collision) is a known cause of acetabular labral tearing.<ref>Lewis C, Sahrmann S. Acetabular labral tears. Physical Therapy. 2006;86(1):110-121.</ref>Additional causes include [[Femoroacetabular Impingement|acetabular impingement]], joint degeneration and childhood disorders such as [[Legg-Calve-Perthes Disease|Legg-Calve-Perthes]] disease, congenital [[Hip Dysplasia|hip dysplasia]] and [[Slipped Capital Femoral Epiphysis|slipped capital femoral epiphysis]].<ref name="SPH">Schmerl M, Pollard H, Hoskins W. Labral Injuries of the hip: a review of diagnosis and management. J Manipulative Physiol Ther. 2005;28(8):632</ref><ref name="BRW">Burgess RM, Rushton A, Wright C, Daborn C. The validity and accuracy of clinical diagnostic tests used to detect labral pathology of the hip: A systematic review. Manual Therapy 16 (2011) 318 – 326.</ref><ref name="GOS" /><ref name="BUR">Burnett SJ, Della Rocca GJ, Prather H, et al. Clinical Presentation of Patients with tears of the Acetabular Labrum. The Journal of Bone Surgery: Volume 88-A · Number 7 · July 2006 pg 1448 - 1456</ref> | The labrum of the hip is susceptible to traumatic injury from the shearing forces that occur with twisting, pivoting and falling. Direct trauma (e.g. motor vehicle collision) is a known cause of acetabular labral tearing.<ref name=":4">Lewis C, Sahrmann S. Acetabular labral tears. Physical Therapy. 2006;86(1):110-121.</ref>Additional causes include [[Femoroacetabular Impingement|acetabular impingement]], joint degeneration and childhood disorders such as [[Legg-Calve-Perthes Disease|Legg-Calve-Perthes]] disease, congenital [[Hip Dysplasia|hip dysplasia]] and [[Slipped Capital Femoral Epiphysis|slipped capital femoral epiphysis]].<ref name="SPH">Schmerl M, Pollard H, Hoskins W. Labral Injuries of the hip: a review of diagnosis and management. J Manipulative Physiol Ther. 2005;28(8):632</ref><ref name="BRW">Burgess RM, Rushton A, Wright C, Daborn C. The validity and accuracy of clinical diagnostic tests used to detect labral pathology of the hip: A systematic review. Manual Therapy 16 (2011) 318 – 326.</ref><ref name="GOS" /><ref name="BUR">Burnett SJ, Della Rocca GJ, Prather H, et al. Clinical Presentation of Patients with tears of the Acetabular Labrum. The Journal of Bone Surgery: Volume 88-A · Number 7 · July 2006 pg 1448 - 1456</ref> While most tears occur in the anterosuperior quadrant, a higher than normal incidence of posterosuperior tears appear in the Asian population due to a higher tendency toward hyperflexion or squatting motions.<ref name="SPH" />The most common mechanism is an external rotation force in a hyperextended position. Microtrauma is believed to be responsible for labral lesions in cases where pain develops gradually. | ||
According to a systematic review by Leiboid et al (2008),<ref name="LHJ" /> | According to a systematic review by Leiboid et al (2008),<ref name="LHJ" /> | ||
| Line 27: | Line 27: | ||
*Hip labral tears commonly occur between 8 to 72 years of age and on average during the fourth decade of life | *Hip labral tears commonly occur between 8 to 72 years of age and on average during the fourth decade of life | ||
*Women are more likely to suffer than men | *Women are more likely to suffer than men | ||
*22-55% of patients | *22-55% of patients with hip or groin pain symptoms are found to have an acetabular labral tear<ref name="comp">Groh MM, Herrera J. A comprehensive review of hip labral tears. Current reviews in musculoskeletal medicine. 2009 Jun 1;2(2):105-17.</ref> | ||
*Up to 74.1% of hip labral tears cannot be attributed to a specific event or cause<ref name="comp" /> | *Up to 74.1% of hip labral tears cannot be attributed to a specific event or cause<ref name="comp" /> | ||
*Hyperabduction, twisting, falling or a direct blow from a car accident were common mechanisms of injury in patients who identified a specific mechanism of injury<ref name="LHJ">Leiboid M, Huijbregts P, Jensen R. Concurrent Criterion-Related Validity of Physical Examination Tests for Hip Labral Lesions: A Systematic Review. The Journal of Manual Manipulative Therapy. [online]. 2008;16(2):E24-41.</ref> | *Hyperabduction, twisting, falling or a direct blow from a car accident were common mechanisms of injury in patients who identified a specific mechanism of injury<ref name="LHJ">Leiboid M, Huijbregts P, Jensen R. Concurrent Criterion-Related Validity of Physical Examination Tests for Hip Labral Lesions: A Systematic Review. The Journal of Manual Manipulative Therapy. [online]. 2008;16(2):E24-41.</ref> | ||
*Women, runners, professional athletes, participants in sports that require frequent external rotation and | *Women, runners, professional athletes, and participants in sports that require frequent external rotation and hyperextension are at increased risk of a hip labral tear. | ||
*Those attending the gym three times a week have an increased risk of developing a hip labral tear<ref name="LHJ" /> | *Those attending the gym three times a week have an increased risk of developing a hip labral tear<ref name="LHJ" /> | ||
Orbell and Smith (2011) note that the incidence of labral tears | Orbell and Smith (2011) note that the incidence of labral tears differs depending on the specific aetiology.<ref name=":0">Orbell S, Smith TO. The physiotherapeutic treatment of acetabular labral tears. A systematic review. Adv Physiother. 2011; 13: 153-161.</ref> | ||
== Mechanism of Injury == | == Mechanism of Injury == | ||
Five common mechanisms of labral tears are widely recognized:<ref name=":0" /> | |||
#[[Femoroacetabular Impingement|Femoroacetabular impingement]] (FAI) | #[[Femoroacetabular Impingement|Femoroacetabular impingement]] (FAI) | ||
#Trauma: This can occur due to a shearing force associated with twisting or falling, | #Trauma: This can occur due to a shearing force associated with twisting or falling, misstepping on uneven ground or colliding with bicycles or vehicles. Repetitive hip hyperextension and external rotation (e.g. in running during terminal stance) can create stress at the chondrolabral junction (typically the 10-12 o'clock position) resulting in microtrauma and eventual labral injury.<ref name=":1">Heiderscheit B, McClinton S. Evaluation and Management of Hip and Pelvis Injuries. Phys Med Rehabil Clin N Am. 2016;27(1):1-29. | ||
</ref> It may also be associated with iliopsoas impingement resulting in labral injury at the 3 o'clock position.<ref name=":1" /> | </ref> It may also be associated with [[Iliopsoas Tendinopathy|iliopsoas]] impingement resulting in labral injury at the 3 o'clock position.<ref name=":1" /> | ||
#Capsular Laxity: This is thought to occur in one of two ways; cartilage disorders (e.g. [[Ehlers-Danlos Syndrome|Ehlers-Danlos syndrome]]) or rotational laxity resulting from excessive external rotation. These forces are often seen in certain sports including ballet, hockey and gymnastics. | #Capsular Laxity: This is thought to occur in one of two ways; cartilage disorders (e.g. [[Ehlers-Danlos Syndrome|Ehlers-Danlos syndrome]]) or rotational laxity resulting from excessive external rotation. These forces are often seen in certain sports including ballet, hockey and gymnastics. | ||
#[[Hip Dysplasia|Hip Dysplasia]]: Certain abnormalities of the femur. acetabulum or both (e.g. shallow acetabulum, femoral or acetabular anteversion, decreased head offset or perpendicular distance from the | #[[Hip Dysplasia|Hip Dysplasia]]: Certain abnormalities of the femur. acetabulum or both (e.g. shallow acetabulum, femoral or acetabular anteversion, decreased head offset or perpendicular distance from the centre of the femoral head to the axis of the femoral shaft) can lead to inadequate containment of the femoral head within the acetabulum, placing increased stress into the anterior portion of the hip joint resulting in impingement and possible tears over time. | ||
#Degeneration | #Degeneration of the joint or surrounding tissues | ||
== Classification == | == Classification == | ||
| Line 54: | Line 54: | ||
{| class="wikitable" | {| class="wikitable" | ||
|Anterior tear | |Anterior tear | ||
| The pain will generally be more consistent and is situated on the anterior hip (anterosuperior quadrant) or at the groin.<ref name="McCarthy">McCarthy JC, Noble PC, Schuck MR, et al. The Otto E. Aufranc Award: the role of labral lesions to development of early degenerative hip disease. Clin Orthop 2001;393:25–37.</ref><ref>O’Leary JA, Berend K, Vail TP. The relationship between diagnosis and outcome in arthroscopy of the hip. Arthroscopy 2001;17:181–188.</ref><ref name="Byrd">Byrd JW. Labral lesions: an elusive source of hip pain case reports and literature review. Arthroscopy 1996;12:603–612.</ref><ref name="Binningsley">Binningsley D. Tear of the acetabular labrum in an elite athlete. Br J Sports Med 2003;37:84–88.</ref><ref name="Hase">Hase T, Ueo T. Acetabularlabral tear: arthroscopic diagnosis and treatment. Arthroscopy 1999;15:138 –141.</ref><ref name="Klaue">Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome: a clinical presentation of dysplasia of the hip. J Bone Joint Surg Br 1991;73:423– 429.</ref> They frequently occur in individuals in European countries and the United States. | | The pain will generally be more consistent and is situated on the anterior hip (anterosuperior quadrant) or at the groin.<ref name="McCarthy">McCarthy JC, Noble PC, Schuck MR, et al. The Otto E. Aufranc Award: the role of labral lesions to development of early degenerative hip disease. Clin Orthop 2001;393:25–37.</ref><ref>O’Leary JA, Berend K, Vail TP. The relationship between diagnosis and outcome in arthroscopy of the hip. Arthroscopy 2001;17:181–188.</ref><ref name="Byrd">Byrd JW. Labral lesions: an elusive source of hip pain case reports and literature review. Arthroscopy 1996;12:603–612.</ref><ref name="Binningsley">Binningsley D. Tear of the acetabular labrum in an elite athlete. Br J Sports Med 2003;37:84–88.</ref><ref name="Hase">Hase T, Ueo T. Acetabularlabral tear: arthroscopic diagnosis and treatment. Arthroscopy 1999;15:138 –141.</ref><ref name="Klaue">Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome: a clinical presentation of dysplasia of the hip. J Bone Joint Surg Br 1991;73:423– 429.</ref> They frequently occur in individuals in European countries and the United States. | ||
|- | |- | ||
|Posterior | |Posterior | ||
|Are situated in the lateral region or deep in the posterior buttocks. They occur less frequently in individuals in European countries and the United States | |Are situated in the lateral region or deep in the posterior buttocks. They occur less frequently in individuals in European countries and the United States but are more common in individuals from Japan.<ref name="McCarthy" /><ref name="Byrd" /><ref name="Hase" /> | ||
|- | |- | ||
|Superior/lateral | |Superior/lateral | ||
| | |occurs rarely | ||
|} | |} | ||
*Morphology: | *Morphology: | ||
{| class="wikitable" | {| class="wikitable" | ||
|Radial flap | |Radial flap | ||
|most common, disruption of free margin of the labrum | |most common, disruption of the free margin of the labrum | ||
|- | |- | ||
|Radial fibrillated | |Radial fibrillated | ||
| | | Fraying of the free margin, associated with degenerative joint disease | ||
|- | |- | ||
|Longitudinal peripheral | |Longitudinal peripheral | ||
| Line 79: | Line 79: | ||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
There is some variation in the presentation of hip labral tears. Patients frequently present with anterior hip and groin pain, although less common areas of pain include anterior thigh pain, lateral thigh pain, buttock pain and radiating knee pain.<ref name="LHJ" /><ref name="comp" /> The majority of patients (90%) diagnosed with acetabular labral tears have had complaints of pain in the anterior hip or groin. <ref name="comp" /><ref name=" | There is some variation in the presentation of hip labral tears. Patients frequently present with anterior hip and groin pain, although less common areas of pain include anterior thigh pain, lateral thigh pain, buttock pain and radiating knee pain.<ref name="LHJ" /><ref name="comp" /> The majority of patients (90%) diagnosed with acetabular labral tears have had complaints of pain in the anterior hip or groin. <ref name="comp" /><ref name=":4" /><ref name="comp" />This can be an indication of an anterior labral tear, whereas buttock pain is more consistent with posterior tears and less common.<ref name="comp" /> | ||
Mechanical symptoms associated with a tear are clicking, locking, popping, giving way, catching and stiffness. The significance of these signs is questionable.<ref name=" | Mechanical symptoms associated with a tear are clicking, locking, popping, giving way, catching and stiffness. The significance of these signs is questionable.<ref name="LHJ" /> Patients often describe a dull ache which increases with activities such as running, brisk walking, twisting movements of the hip or climbing stairs.<ref name=":4" /><ref name="comp" /> These specific manoeuvres may cause pain in the groin; 1) Flexion, adduction, and internal rotation of the hip joint are related to anterior superior tears and 2) Passive hyperextension, abduction, and external rotation are related to posterior tears.<ref>Narvani AA, Tsiridis E, Tai CC, Thomas P. Acetabular labrum and its tears. Br J Sports Med 2003;37:207-211.</ref> Functional limitations may include prolonged sitting, walking, climbing stairs, running, and twisting/pivoting.<ref name=":4" /><ref name="LHJ" /><ref name="comp" /> The symptoms can have a long duration, with an average of greater than two years.<ref name="Farjo">Farjo LA, Glick JM, Sampson TG. Hip arthroscopy for acetabular labral tears. Arthroscopy 1999;15:132–137.</ref> | ||
The patient may report experiencing an audible pop or a sensation of subluxation at the time of the trauma | The patient may report experiencing an audible pop or a sensation of subluxation at the time of the trauma if there was a specific traumatic onset.<ref name=":1" /> | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
Schmerl et al (2005) provide a thorough list for differential diagnosis of labral injury causing hip pain;<ref name="SPH" / | Schmerl et al (2005) provide a thorough list for differential diagnosis of labral injury causing hip pain;<ref name="SPH" /> | ||
*Contusion (especially over bony prominences) | *Contusion (especially over bony prominences) | ||
*Strains | *Strains | ||
*[[Pubalgia|Athletic pubalgia]] | *[[Pubalgia|Athletic pubalgia]] | ||
*Osteitis pubis | *[[Osteitis Pubis|Osteitis pubis]] | ||
*Inflammatory | *Inflammatory arthritis | ||
*[[Piriformis Syndrome|Piriformis syndrome]] | *[[Piriformis Syndrome|Piriformis syndrome]] | ||
*[[Snapping Hip Syndrome|Snapping hip syndrome]] | *[[Snapping Hip Syndrome|Snapping hip syndrome]] | ||
*[[Bursitis]] (trochanteric, ischiogluteal, iliopsoas) | *[[Bursitis]] (trochanteric, ischiogluteal, iliopsoas) | ||
*Osteoarthritis of femoral head | *[[Osteoarthritis]] of femoral head | ||
*[[Avascular | *[[Avascular Necrosis Femoral Head|Avascular necrosis of femoral head]] | ||
*[[Septic (Infectious) Arthritis|Septic arthritis]] | *[[Septic (Infectious) Arthritis|Septic arthritis]] | ||
*Fracture or dislocation | *Fracture or dislocation | ||
| Line 109: | Line 109: | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
According to Heerey et al (2018), hip pain is poorly correlated with intra-articular hip joint pathology seen on diagnostic imaging.<ref name=":2">Heerey JJ, Kemp JL, Mosler AB, Jones DM, Pizzari T, Souza RB et al | According to Heerey et al (2018), hip pain is poorly correlated with intra-articular hip joint pathology seen on diagnostic imaging.<ref name=":2">Heerey JJ, Kemp JL, Mosler AB, Jones DM, Pizzari T, Souza RB et al. What is the prevalence of imaging-defined intra-articular hip pathologies in people with and without pain? A systematic review and meta-analysis. Br J Sports Med. 2018;52(9):581-593. | ||
</ref> In their systematic review, they found that the prevalence of cartilage pathology, bone marrow lesions, | </ref> In their systematic review, they found that the prevalence of cartilage pathology, bone marrow lesions, [[Ligamentum Teres]] tears was higher in symptomatic individuals than in asymptomatic individuals, whereas the prevalence of labral pathology, para labral cysts and herniation pits was similar in both groups.<ref name=":2" /> | ||
When diagnostic imaging is | When diagnostic imaging is utilised, MR arthrogram has typically been preferred over MRI because it has shown greater accuracy in identifying defects in the labrum and cartilage.<ref name=":13">Chopra A, Grainger AJ, Dube B, Evans R, Hodgson R, Conroy J et al. Comparative reliability and diagnostic performance of conventional 3T magnetic resonance imaging and 1.5T magnetic resonance arthrography for the evaluation of internal derangement of the hip. Eur Radiol. 2018 Mar;28(3):963-971.</ref> However, more recent research suggests that 3T MRI is at least equivalent to 1.5T MRA for detecting these types of defects.<ref name=":13" /> | ||
== Examination == | == Examination == | ||
Diagnosis | Diagnosis is aided by a physical examination of a patient. In some cases the first signs can be spotted while observing the patient; during a brief walk, the ipsilateral knee may be used to absorb the shocks created by ground reaction forces; thus presenting with a flexed knee gait. Additionally related to gait, the step length of the affected leg may also be shortened, again; to reduce the nociceptive input caused by walking. Aside from simple observation there are several provocative tests that can be performed. Because each test stresses a particular part of the acetabular labrum, they can also indicate where the tear is located.<ref name="comp" /> | ||
Labral tears can be difficult to differentiate from FAI and the two conditions can be present simultaneously.<ref name=":1" /> Pain from an isolated labral tear may be associated with hip extension (compared to hip flexion for FAI) as well as signs of laxity.<ref name=":1" /> Tightness in ilio[[Psoas Major|psoas]] or pain with resistance testing of [[Iliacus|ilio]]<nowiki/>psoas may indicate iliopsoas impingement with is associated with labral tearing but not FAI.<ref name=":1" /> However,even if differentiating the two conditions remains difficult following physical examination, Heiderscheit and McClinton (2016) note that initial management of the two is the same.<ref name=":1" /> | Labral tears can be difficult to differentiate from FAI and the two conditions can be present simultaneously.<ref name=":1" /> Pain from an isolated labral tear may be associated with hip extension (compared to hip flexion for FAI) as well as signs of laxity.<ref name=":1" /> Tightness in ilio[[Psoas Major|psoas]] or pain with resistance testing of [[Iliacus|ilio]]<nowiki/>psoas may indicate iliopsoas impingement with is associated with labral tearing but not FAI.<ref name=":1" /> However, even if differentiating the two conditions remains difficult following physical examination, Heiderscheit and McClinton (2016) note that initial management of the two is the same.<ref name=":1" /> | ||
=== Provocative Tests === | === Provocative Tests === | ||
Strong evidence in support of provocative clinical tests for diagnosing hip labral disorders is lacking. Reiman et al (2015) conducted a systematic review to evaluate the clinical accuracy of | Strong evidence in support of provocative clinical tests for diagnosing hip labral disorders is lacking. Reiman et al (2015) conducted a systematic review to evaluate the clinical accuracy of several provocative tests. They found that most of the tests were predominantly sensitive but not specific and that none was capable of significantly shifting the post-test probability of a diagnosis of acetabular labral tear.<ref name=":3">Reiman MP, Goode AP, Cook CE, Hölmich P, Thorborg K. Diagnostic accuracy of clinical tests for the diagnosis of hip femoroacetabular impingement/labral tear: a systematic review with meta-analysis. Br J Sports Med. 2015;49(12):811. | ||
</ref> In addition, the studies that were investigated in the review were of low quality and were at risk of bias.<ref name=":3" /> The authors noted the need for better quality studies in patients with and without hip pathology to evaluate the true clinical utility of these tests.<ref name=":3" /> According to a 2008 study by Martin et al, symptoms of groin pain, catching, pinching pain with sitting, FABER test, flexion-internal rotation, adduction impingement test and trochanteric tenderness were found to have low sensitivities (.6-.78) and low specificities (.10-.56) in identifying patients with intra-articular pain.<ref>Martin RL, Irrgang J, Sekiya J. The Diagnostic Accuracy of a Clinical Examination in Determining Intra-articular Hip Pain for Potential Hip Arthroscopy Candidates. The Journal of Arthroscopic and Related Surgery. 2008;(52225):1-6</ref> Other tests found to have high specificities but lacking high-quality study designs and supportive literature include the Flexion-Adduction-Axial Compression test and palpation to the greater trochanter. Flexion-Internal Rotation-Axial Compression test, Thomas test, Maximum Flexion-External Rotation Test and Maximum Flexion-Internal Rotation Tests were found to have poor diagnostic measures.<ref name="LHJ" /> | </ref> In addition, the studies that were investigated in the review were of low quality and were at risk of bias.<ref name=":3" /> The authors noted the need for better quality studies in patients with and without hip pathology to evaluate the true clinical utility of these tests.<ref name=":3" /> According to a 2008 study by Martin et al, symptoms of groin pain, catching, pinching pain with sitting, [[FABER Test|FABER]] test, flexion-internal rotation, adduction impingement test and trochanteric tenderness were found to have low sensitivities (.6-.78) and low specificities (.10-.56) in identifying patients with intra-articular pain.<ref>Martin RL, Irrgang J, Sekiya J. The Diagnostic Accuracy of a Clinical Examination in Determining Intra-articular Hip Pain for Potential Hip Arthroscopy Candidates. The Journal of Arthroscopic and Related Surgery. 2008;(52225):1-6</ref> Other tests found to have high specificities but lacking high-quality study designs and supportive literature include the Flexion-Adduction-Axial Compression test and palpation to the greater trochanter. Flexion-Internal Rotation-Axial Compression test, [[Thomas Test|Thomas test]], Maximum Flexion-External Rotation Test and Maximum Flexion-Internal Rotation Tests were found to have poor diagnostic measures.<ref name="LHJ" /> | ||
The following provocative tests have been indicated as useful in diagnosing hip labral disorders but because of low clinical accuracy (especially specificity), their results should be evaluated within the context of patient presentation and examination; | The following provocative tests have been indicated as useful in diagnosing hip labral disorders but because of low clinical accuracy (especially specificity), their results should be evaluated within the context of patient presentation and examination; | ||
*'''[[McCarthy test]]''', The affected hip needs to be brought into extension. If this movement reproduces a painful click, the patient is suffering from a labral tear.<ref name="McCarty et al">McCarthy JC, Noble P, Schuck M, Alusio FV, Wright J, Lee J. “Acetabular and labral pathology.” In: McCarthy JC, editor. Early hip disorders. New York7 Springer Verlag; 2003. p. 113-33.</ref> | *'''[[McCarthy test]]''', The affected hip needs to be brought into extension. If this movement reproduces a painful click, the patient is suffering from a labral tear.<ref name="McCarty et al">McCarthy JC, Noble P, Schuck M, Alusio FV, Wright J, Lee J. “Acetabular and labral pathology.” In: McCarthy JC, editor. Early hip disorders. New York7 Springer Verlag; 2003. p. 113-33.</ref> | ||
*'''[[FABER Test]]''', flexion-abduction-external rotation test elicits 88% of the patient with an articular pathology. However this test is non-specific and should be considered a general test for hip articular surfaces<ref name=" | *'''[[FABER Test]]''', flexion-abduction-external rotation test elicits 88% of the patient with an articular pathology. However, this test is non-specific and should be considered a general test for hip articular surfaces<ref name="SPH" /> | ||
*[https://www.youtube.com/watch?v=wmK_PhkUbaM '''Anterior labral tear'''] | *[https://www.youtube.com/watch?v=wmK_PhkUbaM '''Anterior labral tear'''] - The anterior [[Labral Tear|labral tear]] is the test in which the patient's leg has to be brought into full flexion, lateral rotation and full abduction. Then the leg has to be extended with medial rotation and adduction. Patients with an anterior labral tear will experience sharp catching pain and in some cases, there might be a "clicking" of the hip<ref name=":4" />. | ||
*'''[https://www.youtube.com/watch?v=TWhJpSt1lZg Posterior Labral tear] | *'''[https://www.youtube.com/watch?v=TWhJpSt1lZg Posterior Labral tear] - '''The posterior labral tear is identified by bringing the patient's leg into extension, abduction and lateral rotation followed by an extension with medial rotation and adduction of the leg. Sharp catching pain with or without a "click" will be an indication of a posterior labral tear. | ||
*'''Impingement Test '''(Flexion-Adduction-Internal Rotation Test/FADIR), the patient is placed in supine and the examiner passively flexes the hip to 90 degrees while performing adduction and internal rotation. | *'''Impingement Test '''([[FADIR (Flexion, Adduction, Internal Rotation) Test|Flexion-Adduction-Internal Rotation Test/FADIR]]), the patient is placed in supine and the examiner passively flexes the hip to 90 degrees while performing adduction and internal rotation. Similar to the FABER test, this should be considered a generalised test additionally, test positions and definitions of a positive test vary in literature. The Impingement test [[FADIR (Flexion, Adduction, Internal Rotation) Test|(Flexion-Adduction-Internal Rotation Test)]] has a sensitivity of .75.<ref name="BRW" /> | ||
*'''[[Fitzgerald Test]]'''. The Fitzgerald test utilizes two different test positions to determine if the patient has an anterior or posterior labral tear. To test for | *'''[[Fitzgerald Test]]'''. The Fitzgerald test utilizes two different test positions to determine if the patient has an anterior or posterior labral tear. To test for an anterior labral tear, the patient lies supine, then the physical therapist (PT) performs flexion, external rotation, and full abduction of the hip, followed by extending the hip, internal rotation, and adduction. To test for a posterior labral tear, the PT performs passive extension, abduction, external rotation, from the position of full hip flexion, internal rotation, and adduction while the patient is supine. Tests are considered to be positive with pain reproduction with or without an audible click<ref name="LHJ" /><ref name=":4" />. The Fitzgerald test has a sensitivity of .98<ref name="LHJ" /><ref name="BRW" />. | ||
*Resisted SLR | *Resisted SLR | ||
*Anterior hip impingement test | *Anterior hip impingement test | ||
| Line 140: | Line 140: | ||
== Medical Management == | == Medical Management == | ||
The most common treatment and usually the first step on the treatment ladder is conservative treatment and | The most common treatment and usually the first step on the treatment ladder is conservative treatment and medication (NSAIDs). When conservative treatment does not resolve symptoms, surgical intervention may be appropriate. | ||
The most common procedure is | * The most common procedure is excision or debridement of the torn tissue by joint arthroscopy. However, studies have demonstrated mixed post-surgical results. Fargo et al found a significant correlation between outcomes and the presence of arthritis on radiography. Only 21% of patients with detectable arthritis had good results from surgery, compared with 75% of patients without arthritis. Arthroscopic detection of chondromalacia was an even stronger indicator of poor long-term prognosis.<ref name=":4" /> | ||
* For a simple tear, surgery involves a bioabsorbable suture anchor being placed over the tear to stabilize the fibrocartilaginous tissue back onto the rim of the acetabulum when the labrum has detached from the bone. | |||
For a simple tear, surgery involves a bioabsorbable suture anchor being placed over the tear to stabilize the fibrocartilaginous tissue back onto the rim of the acetabulum when the labrum has detached from the bone. | * If the pathology is caused by a malalignment (e.g. [[Legg-Calve-Perthes Disease|Perthes]] or hip dysplasia), femoral or pelvic [[Osteotomy|osteotomies]] are considered. A femoral osteotomy is a surgical treatment where the femur is cut and angled differently in an attempt to improve the mechanics of the leg. | ||
* Surgical treatment has been shown to have a short-term improvement in patient-reported outcomes and functional scores post-operatively, however, the long-term outcomes remain unknown. <ref name=":4" /><ref>Ayeni, O. R., Alradwan, H., de Sa, D., & Philippon, M. J. (2014). The hip labrum reconstruction: indications and outcomes—a systematic review. ''Knee Surgery, Sports Traumatology, Arthroscopy'', ''22''(4), 737-743.</ref> | |||
If the pathology is caused | * Repair of the acetabular labral lesion can be performed in either the supine or lateral position. In the supine position, a stand fracture table is used with an oversized personal post to apply traction. The affected hip is placed into slight extension/adduction to allow an approach to the joint. During traction, it is important that there is a minimized pressure in the perineal area to avoid neurologic complications. The procedure is under the guidance of fluoroscopy. If the distraction is obtained a 14 or 16 gauge spinal needle is inserted into the joint to break the vacuum seal and allow further distraction. Three portals are used (the anterolateral, anterior and the distal lateral accessory). | ||
* For repair of a detached labrum, the edges of the tear are delineated and suture anchors are placed on top of the acetabular rim in the area of detachment. If the tear in the labrum has a secure outer rim and is still attached to the acetabulum, a suture in the mid substance of the tear can be used to secure it.<ref name="GOS" /> | |||
Surgical treatment has been shown to have short-term improvement in patient reported outcomes and functional scores post-operatively, however the long-term outcomes remain unknown. <ref name=" | |||
Repair of the acetabular labral lesion can be | |||
{{#ev:youtube|MJc7JHjfz1Q|300}} | {{#ev:youtube|MJc7JHjfz1Q|300}} | ||
| Line 162: | Line 159: | ||
=== Post-surgical Rehabilitation === | === Post-surgical Rehabilitation === | ||
Movements that cause stress in the area need to be avoided. The rehabilitation protocol following acetabular labral debridement or repair | Movements that cause stress in the area need to be avoided. The rehabilitation protocol following acetabular labral debridement or repair is divided into four phases. | ||
=== Phase 1. Initial exercise (week 1-4) === | === Phase 1. Initial exercise (week 1-4) === | ||
The primary goals following | The primary goals following an acetabulolabral debridement or repair are to minimize pain and inflammation, and initiate early motion exercises. This phase initially consists of isometric contraction exercises for the hip adductors, abductors, transverse abdominals and extensor muscles. Following a labral debridement, closed-chain activities such as low-level leg press or shuttle can begin with limited resistance. | ||
<br>Weight bearing protocol following a debridement is 50% for 7 to 10 days, and non-weight bearing or toe-touch weight bearing for 3 to 6 weeks in case of a labral repair. Unnecessary hypomobility will limit progress in future phases, thus it is important to ensure that the patient maintains adequate mobility and range during this phase. | <br>Weight bearing protocol following a debridement is 50% for 7 to 10 days, and non-weight bearing or toe-touch weight bearing for 3 to 6 weeks in case of a labral repair. Unnecessary hypomobility will limit progress in future phases, thus it is important to ensure that the patient maintains adequate mobility and range during this phase. | ||
| Line 172: | Line 169: | ||
<br>'''Treatment modalities:''' | <br>'''Treatment modalities:''' | ||
*[[Aquatherapy|Aquatic therapy]] is a suitable treatment approach - movement in the water allows for improvement in [[Gait Cycle|gait]] by allowing appropriate loads to be placed on the joint without causing unnecessary stress to the healing tissue. For example, the patient may perform | *[[Aquatherapy|Aquatic therapy]] is a suitable treatment approach - movement in the water allows for improvement in [[Gait Cycle|gait]] by allowing appropriate loads to be placed on the joint without causing unnecessary stress to the healing tissue. For example, the patient may perform jogging in the water using a flotation device. It is important to know the patient's range of motion precautions, as these may vary in debridement or repair. | ||
*Manual therapy for pain reduction and improvement in joint mobility and proprioception. Considerations include gentle hip joint mobilizations contract-relax stretching for internal and external rotation, long axis distraction, and assessment of lumbo-sacral mobility. | *Manual therapy for pain reduction and improvement in joint mobility and proprioception. Considerations include gentle hip joint mobilizations contract-relax stretching for internal and external rotation, long-axis distraction, and assessment of lumbo-sacral mobility. | ||
*[[Cryotherapy|Cryotherapy]] | *[[Cryotherapy|Cryotherapy]] | ||
*Appropriate pain management through medication. | *Appropriate pain management through medication. | ||
*Gentle stretching of hip muscle groups including piriformis, psoas, quadriceps, hamstring muscles with passive range of motion. | *Gentle stretching of hip muscle groups including [[piriformis]], psoas, [[Quadriceps Muscle|quadriceps]], [[Hamstrings|hamstring]] muscles with passive range of motion. | ||
*Stationary bike without resistance, with seat height that limits the hip to less than 90° | *Stationary bike without resistance, with seat height that limits the hip to less than 90° | ||
*Exercises such as | *Exercises such as water walking, piriformis stretch, and ankle pumps. | ||
To progress to phase 2, ROM has to be greater or equal to 75%. | To progress to phase 2, ROM has to be greater or equal to 75%. | ||
| Line 184: | Line 181: | ||
=== Phase 2. Intermediate exercise (week 5-7) === | === Phase 2. Intermediate exercise (week 5-7) === | ||
The goal of this phase is to continue | The goal of this phase is to continue improving ROM and soft tissue flexibility. Manual therapy should continue with more aggressive mobilization, passive ROM exercises should become more aggressive as needed, for external- and internal rotation. | ||
*Flexibility exercises involving the piriformis, adductor group, psoas/rectus femoris should continue | *Flexibility exercises involving the piriformis, adductor group, psoas/rectus femoris should continue | ||
| Line 193: | Line 190: | ||
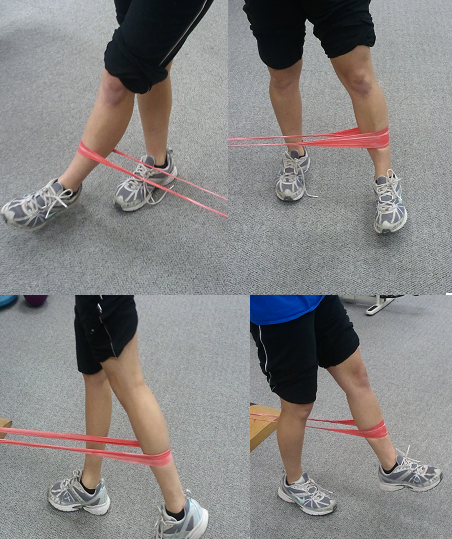
*Exercises such as wall sits with abductor band, two leg bridging<br> | *Exercises such as wall sits with abductor band, two leg bridging<br> | ||
To progress to the third phase | To progress to the third phase the patient must have a [[Gait Cycle|normal gait pattern]] with no [[Trendelenburg Sign|Trendelenburg]] sign. The patient should have symmetrical and passive ROM measurements with minimal complaints of pain. | ||
=== Phase 3. Advanced Exercise (week 8-12) === | === Phase 3. Advanced Exercise (week 8-12) === | ||
| Line 199: | Line 196: | ||
*Manual therapy should be performed as needed | *Manual therapy should be performed as needed | ||
*Flexibility and passive ROM interventions should become slightly more aggressive if the limitations persist (if the patient has reached his full ROM or flexibility, terminal stretches should be initiated) | *Flexibility and passive ROM interventions should become slightly more aggressive if the limitations persist (if the patient has reached his full ROM or flexibility, terminal stretches should be initiated) | ||
*Strengthening exercises: walking lunges, lunges with trunk rotations, | *Strengthening exercises: walking lunges, lunges with trunk rotations, resistant sportcord, walking forward/backwards, plyometric bounding in the water. | ||
*Exercises such as core ball stabilization, golf progression, lunges | *Exercises such as core ball stabilization, golf progression, lunges | ||
To progress to the | To progress to the fourth phase, there must be symmetrical ROM and flexibility of the psoas and piriformis. | ||
=== Phase 4. Sport-specific training (12-*) === | |||
Exercises such as | * In this phase, it is important to return safely and effectively back to competition or previous activity level. | ||
* Manual therapy, flexibility, and ROM exercises can continue as appropriate. | |||
* It is important that the patient has good muscular endurance, good eccentric muscle control, and the ability to generate power. | |||
* The patient can be given sport-specific exercises and has to have the ability to demonstrate good neuromuscular control of the lower extremity during the activities. | |||
* Exercises such as sport-specific drills, functional testing | |||
The goal during physical therapy of an acetabular labral tear is to optimize the alignment of the hip joint and the precision of joint motion <ref name=" | The goal during physical therapy of an acetabular labral tear is to optimize the alignment of the hip joint and the precision of joint motion <ref name=":4" />. This can be done by: | ||
#Reducing anteriorly directed forces on the hip by addressing the patterns of recruitment of muscles that control hip motion and by correcting movement patterns during exercises such as hip extension and | #Reducing anteriorly directed forces on the hip by addressing the patterns of recruitment of muscles that control hip motion and by correcting movement patterns during exercises such as hip extension and gait <ref name=":4" />. | ||
#Instructing patients to avoid pivoting motions, especially under load, since the acetabulum rotates on a loaded femur, thus increasing force across the labrum <ref name="comp" /><ref name=" | #Instructing patients to avoid pivoting motions, especially under load, since the acetabulum rotates on a loaded femur, thus increasing force across the labrum <ref name="comp" /><ref name=":4" /> | ||
So far there has been no research on the efficacy of hip mobilization or manipulation in the treatment of labral disorders. Although it is suggested that the therapy should focus on optimizing the alignment of the hip joint and the precision of joint motion, avoiding pivoting motions and correcting gait patterns. | So far there has been no research on the efficacy of hip mobilization or manipulation in the treatment of labral disorders. Although it is suggested that the therapy should focus on optimizing the alignment of the hip joint and the precision of joint motion, avoiding pivoting motions and correcting gait patterns.<ref name="SPH" /> | ||
As these patients have abnormal recruitment patterns of the hip muscles due to the | As these patients have abnormal recruitment patterns of the hip muscles due to the biomechanics of the pathology, treatment should optimize control of these muscles, specifically the hip adductors, deep external rotators, m. [[Gluteus Maximus|gluteus maximus]], and m. iliopsoas muscles <ref name=":4" /><ref name="YOMF">Yazbek PM, Ovanessian V, Martin RL, Fukuda TY. Nonsurgical treatment of acetabular labrum tears: a case series. J of Ortho Sports PT. 2011 May; 41(5): 346-353</ref>. Additionally, if m. quadriceps femoris and hamstring muscles dominate, this should be corrected, as decreased force contribution from the m. iliopsoas during hip flexion and from the gluteal muscles during active hip extension results in greater anterior hip forces.<ref name="LSM">Lewis CL, Sahrmann SA, Moran DW. Effect of hip angle on anterior hip force during gait. Gait Posture. 2010 Oct; 32(4): 603-607</ref> | ||
Through gait and foot motion analysis, any abnormalities such as knee hyperextension causing hip hyperextension, walking with an externally rotated hip, or stiffness in the subtalar joint can be analysed and can be corrected through taping, orthotics or strengthening <ref name=" | Through gait and foot motion analysis, any abnormalities such as knee hyperextension causing hip hyperextension, walking with an externally rotated hip, or stiffness in the [[Subtalar Joint|subtalar]] joint can be analysed and can be corrected through taping, orthotics or strengthening <ref name=":4" />. Gait analysis may also uncover decreased hip abduction during both the stance and swing phase, and decreased hip extension during the swing phase -- characteristics that may be part of a hip joint stabilization strategy used by patients to compensate for deficient hip musculature functionality.<ref>Kennedy MJ, Lamontagne M, Beaule PE. Femoroacetabular impingement alters hip and pelvic biomechanics during gait. Gait Posture. 30(2009) 41-44</ref> | ||
Additionally, patients need to be educated regarding modification of functional activities to avoid any positions that cause pain, such as sitting with knees lower than hips or with legs crossed, getting up from a chair by rotating the pelvis on a loaded femur, hyperextending the hip while walking on a treadmill, etc. | Additionally, patients need to be educated regarding modification of functional activities to avoid any positions that cause pain, such as sitting with knees lower than hips or with legs crossed, getting up from a chair by rotating the pelvis on a loaded femur, hyperextending the hip while walking on a treadmill, etc. | ||
After addressing abnormal movement patterns, focused muscle strengthening work and recovery of normal range of motion, patients eventually need to | After addressing abnormal movement patterns, focused muscle strengthening work and recovery of a normal range of motion, patients eventually need to progress to advanced sensory-motor training and functional exercises, sport-specific if applicable.<ref name="YOMF" /> | ||
The first six weeks post-surgery are usually NWB or TTWB after surgery. Active and active assisted exercises are appropriate in gravity-minimized positions to maintain the motion of the hip. A stationary bike, not a recumbent bicycle, is appropriate; end-range hip flexion should be done passively rather than actively. Currently, rehabilitation protocols are based on surgeon and PT experience and can follow either labral debridement or repair guidelines, depending on the procedure performed, and move through 4 basic phases. The four basic phases follow the general progression of initial exercises, intermediate exercises, advanced exercises and sports-specific training. <ref name="GOS">Garrison JC, Osler MT, Singleton SB. Rehabilitation after arthroscopy of an acetabular labral tear. N Amer J of Sports PT. 2007 Nov; 2(4): 241-249</ref> | |||
[[Image:Hip Theraband.png|Phase I: Hip Resisted AROM Exercises]][[Image:Trampoline-squat.jpg|300x400px|Phase 2: Hip Neuromuscular Re-education]]<br>{{#ev:youtube|inUc9FBx_ac}} | [[Image:Hip Theraband.png|Phase I: Hip Resisted AROM Exercises]][[Image:Trampoline-squat.jpg|300x400px|Phase 2: Hip Neuromuscular Re-education]]<br>{{#ev:youtube|inUc9FBx_ac}} | ||
| Line 235: | Line 230: | ||
== Outcome Measures == | == Outcome Measures == | ||
* [[International Hip Outcome Tool (iHOT)|International Hip Outcome Tool]] (iHOT) | * [[International Hip Outcome Tool (iHOT)|International Hip Outcome Tool]] (iHOT) | ||
* Hip and Groin Outcome Score (HAGOS) | * [[The Copenhagen Hip and Groin Outcome Score (HAGOS)|Hip and Groin Outcome Score (HAGOS)]] | ||
* Hip Outcome Score (HOS) | * [[Hip Outcome Score|Hip Outcome Score (HOS)]] | ||
* [[Harris Hip Score]] (HHS) | * [[Harris Hip Score]] (HHS) | ||
* | * [[Nonarthritic Hip Score]] | ||
* [[Lower Extremity Functional Scale (LEFS)|Lower Extremity Functional Scale]] (LEFS) | * [[Lower Extremity Functional Scale (LEFS)|Lower Extremity Functional Scale]] (LEFS) | ||
* Lequesne Hip Score | * [[Lequesne Hip Score]] | ||
{{#ev:youtube|EtoOycWxQBo}} | {{#ev:youtube|EtoOycWxQBo}} | ||
Latest revision as of 13:44, 18 March 2024
Original Editor - Karolyn Conolty, Kenny Bosmans, Juliana Doyle,Alisha Lopez, Bilitis Crokaert as part of the Vrije Universiteit Brussel Project.
Top Contributors - Laura Ritchie, Scott Buxton, Kenny Bosmans, Admin, Daan Vandebriel, Kim Jackson, Rachael Lowe, Vidya Acharya, Bram Van Steenbergen, Uchechukwu Chukwuemeka, Naomi O'Reilly, Tomer Yona, Kai A. Sigel, WikiSysop, Wanda van Niekerk, Eric Robertson, Kirenga Bamurange Liliane, Karolyn Conolty, Shreya Pavaskar, Tim Noteboom and Trista Chan
Introduction[edit | edit source]
Disorders of the hip labrum is an umbrella term that includes any issues involving that labrum such as femoroacetabular impingement (aka FAI) and acetabular labral tear (ALT). This mechanically induced pathology is thought to result from excessive forces at the hip joint. For example, a tear could decrease the acetabular contact area and increase stress, resulting in articular damage and destabilising the hip joint.[1] Amber and Mohan (2018) proposed that the term "fissure" is a better alternative to labral tears, at least in patients over the age of 40, to prevent overdiagnosis and unnecessary medical intervention.[2]
Clinically Relevant Anatomy[edit | edit source]
The hip (acetabulofemoral joint) is a synovial joint formed between the femur and acetabulum of the pelvis. The head of the femur is covered by Type II collagen (hyaline cartilage) and proteoglycan. The acetabulum is the concave portion of the ball and socket joint. The acetabulum has a ring of fibrocartilage called the labrum that deepens the acetabulum and improves the stability of the hip joint. For a more detailed review of the anatomy of the hip, please see the Hip Anatomy article.
Epidemiology/Aetiology[edit | edit source]
The labrum of the hip is susceptible to traumatic injury from the shearing forces that occur with twisting, pivoting and falling. Direct trauma (e.g. motor vehicle collision) is a known cause of acetabular labral tearing.[1]Additional causes include acetabular impingement, joint degeneration and childhood disorders such as Legg-Calve-Perthes disease, congenital hip dysplasia and slipped capital femoral epiphysis.[3][4][5][6] While most tears occur in the anterosuperior quadrant, a higher than normal incidence of posterosuperior tears appear in the Asian population due to a higher tendency toward hyperflexion or squatting motions.[3]The most common mechanism is an external rotation force in a hyperextended position. Microtrauma is believed to be responsible for labral lesions in cases where pain develops gradually.
According to a systematic review by Leiboid et al (2008),[7]
- Hip labral tears commonly occur between 8 to 72 years of age and on average during the fourth decade of life
- Women are more likely to suffer than men
- 22-55% of patients with hip or groin pain symptoms are found to have an acetabular labral tear[8]
- Up to 74.1% of hip labral tears cannot be attributed to a specific event or cause[8]
- Hyperabduction, twisting, falling or a direct blow from a car accident were common mechanisms of injury in patients who identified a specific mechanism of injury[7]
- Women, runners, professional athletes, and participants in sports that require frequent external rotation and hyperextension are at increased risk of a hip labral tear.
- Those attending the gym three times a week have an increased risk of developing a hip labral tear[7]
Orbell and Smith (2011) note that the incidence of labral tears differs depending on the specific aetiology.[9]
Mechanism of Injury[edit | edit source]
Five common mechanisms of labral tears are widely recognized:[9]
- Femoroacetabular impingement (FAI)
- Trauma: This can occur due to a shearing force associated with twisting or falling, misstepping on uneven ground or colliding with bicycles or vehicles. Repetitive hip hyperextension and external rotation (e.g. in running during terminal stance) can create stress at the chondrolabral junction (typically the 10-12 o'clock position) resulting in microtrauma and eventual labral injury.[10] It may also be associated with iliopsoas impingement resulting in labral injury at the 3 o'clock position.[10]
- Capsular Laxity: This is thought to occur in one of two ways; cartilage disorders (e.g. Ehlers-Danlos syndrome) or rotational laxity resulting from excessive external rotation. These forces are often seen in certain sports including ballet, hockey and gymnastics.
- Hip Dysplasia: Certain abnormalities of the femur. acetabulum or both (e.g. shallow acetabulum, femoral or acetabular anteversion, decreased head offset or perpendicular distance from the centre of the femoral head to the axis of the femoral shaft) can lead to inadequate containment of the femoral head within the acetabulum, placing increased stress into the anterior portion of the hip joint resulting in impingement and possible tears over time.
- Degeneration of the joint or surrounding tissues
Classification[edit | edit source]
Labral tears can be classified in different ways.[8]
- Etiology
- Location:
| Anterior tear | The pain will generally be more consistent and is situated on the anterior hip (anterosuperior quadrant) or at the groin.[11][12][13][14][15][16] They frequently occur in individuals in European countries and the United States. |
| Posterior | Are situated in the lateral region or deep in the posterior buttocks. They occur less frequently in individuals in European countries and the United States but are more common in individuals from Japan.[11][13][15] |
| Superior/lateral | occurs rarely |
- Morphology:
| Radial flap | most common, disruption of the free margin of the labrum |
| Radial fibrillated | Fraying of the free margin, associated with degenerative joint disease |
| Longitudinal peripheral | least common |
| Unstable / Abnormally mobile | can result from a detached labrum |
Characteristics/Clinical Presentation[edit | edit source]
There is some variation in the presentation of hip labral tears. Patients frequently present with anterior hip and groin pain, although less common areas of pain include anterior thigh pain, lateral thigh pain, buttock pain and radiating knee pain.[7][8] The majority of patients (90%) diagnosed with acetabular labral tears have had complaints of pain in the anterior hip or groin. [8][1][8]This can be an indication of an anterior labral tear, whereas buttock pain is more consistent with posterior tears and less common.[8]
Mechanical symptoms associated with a tear are clicking, locking, popping, giving way, catching and stiffness. The significance of these signs is questionable.[7] Patients often describe a dull ache which increases with activities such as running, brisk walking, twisting movements of the hip or climbing stairs.[1][8] These specific manoeuvres may cause pain in the groin; 1) Flexion, adduction, and internal rotation of the hip joint are related to anterior superior tears and 2) Passive hyperextension, abduction, and external rotation are related to posterior tears.[17] Functional limitations may include prolonged sitting, walking, climbing stairs, running, and twisting/pivoting.[1][7][8] The symptoms can have a long duration, with an average of greater than two years.[18]
The patient may report experiencing an audible pop or a sensation of subluxation at the time of the trauma if there was a specific traumatic onset.[10]
Differential Diagnosis[edit | edit source]
Schmerl et al (2005) provide a thorough list for differential diagnosis of labral injury causing hip pain;[3]
- Contusion (especially over bony prominences)
- Strains
- Athletic pubalgia
- Osteitis pubis
- Inflammatory arthritis
- Piriformis syndrome
- Snapping hip syndrome
- Bursitis (trochanteric, ischiogluteal, iliopsoas)
- Osteoarthritis of femoral head
- Avascular necrosis of femoral head
- Septic arthritis
- Fracture or dislocation
- Tumors (malignant and benign)
- Hernia (inguinal or femoral)
- Slipped capital femoral epiphysis
- Legg-Calve-Perthes disease
- Referred pain from lumbosacral or sacroiliac regions
Diagnostic Procedures[edit | edit source]
According to Heerey et al (2018), hip pain is poorly correlated with intra-articular hip joint pathology seen on diagnostic imaging.[19] In their systematic review, they found that the prevalence of cartilage pathology, bone marrow lesions, Ligamentum Teres tears was higher in symptomatic individuals than in asymptomatic individuals, whereas the prevalence of labral pathology, para labral cysts and herniation pits was similar in both groups.[19]
When diagnostic imaging is utilised, MR arthrogram has typically been preferred over MRI because it has shown greater accuracy in identifying defects in the labrum and cartilage.[20] However, more recent research suggests that 3T MRI is at least equivalent to 1.5T MRA for detecting these types of defects.[20]
Examination[edit | edit source]
Diagnosis is aided by a physical examination of a patient. In some cases the first signs can be spotted while observing the patient; during a brief walk, the ipsilateral knee may be used to absorb the shocks created by ground reaction forces; thus presenting with a flexed knee gait. Additionally related to gait, the step length of the affected leg may also be shortened, again; to reduce the nociceptive input caused by walking. Aside from simple observation there are several provocative tests that can be performed. Because each test stresses a particular part of the acetabular labrum, they can also indicate where the tear is located.[8]
Labral tears can be difficult to differentiate from FAI and the two conditions can be present simultaneously.[10] Pain from an isolated labral tear may be associated with hip extension (compared to hip flexion for FAI) as well as signs of laxity.[10] Tightness in iliopsoas or pain with resistance testing of iliopsoas may indicate iliopsoas impingement with is associated with labral tearing but not FAI.[10] However, even if differentiating the two conditions remains difficult following physical examination, Heiderscheit and McClinton (2016) note that initial management of the two is the same.[10]
Provocative Tests[edit | edit source]
Strong evidence in support of provocative clinical tests for diagnosing hip labral disorders is lacking. Reiman et al (2015) conducted a systematic review to evaluate the clinical accuracy of several provocative tests. They found that most of the tests were predominantly sensitive but not specific and that none was capable of significantly shifting the post-test probability of a diagnosis of acetabular labral tear.[21] In addition, the studies that were investigated in the review were of low quality and were at risk of bias.[21] The authors noted the need for better quality studies in patients with and without hip pathology to evaluate the true clinical utility of these tests.[21] According to a 2008 study by Martin et al, symptoms of groin pain, catching, pinching pain with sitting, FABER test, flexion-internal rotation, adduction impingement test and trochanteric tenderness were found to have low sensitivities (.6-.78) and low specificities (.10-.56) in identifying patients with intra-articular pain.[22] Other tests found to have high specificities but lacking high-quality study designs and supportive literature include the Flexion-Adduction-Axial Compression test and palpation to the greater trochanter. Flexion-Internal Rotation-Axial Compression test, Thomas test, Maximum Flexion-External Rotation Test and Maximum Flexion-Internal Rotation Tests were found to have poor diagnostic measures.[7]
The following provocative tests have been indicated as useful in diagnosing hip labral disorders but because of low clinical accuracy (especially specificity), their results should be evaluated within the context of patient presentation and examination;
- McCarthy test, The affected hip needs to be brought into extension. If this movement reproduces a painful click, the patient is suffering from a labral tear.[23]
- FABER Test, flexion-abduction-external rotation test elicits 88% of the patient with an articular pathology. However, this test is non-specific and should be considered a general test for hip articular surfaces[3]
- Anterior labral tear - The anterior labral tear is the test in which the patient's leg has to be brought into full flexion, lateral rotation and full abduction. Then the leg has to be extended with medial rotation and adduction. Patients with an anterior labral tear will experience sharp catching pain and in some cases, there might be a "clicking" of the hip[1].
- Posterior Labral tear - The posterior labral tear is identified by bringing the patient's leg into extension, abduction and lateral rotation followed by an extension with medial rotation and adduction of the leg. Sharp catching pain with or without a "click" will be an indication of a posterior labral tear.
- Impingement Test (Flexion-Adduction-Internal Rotation Test/FADIR), the patient is placed in supine and the examiner passively flexes the hip to 90 degrees while performing adduction and internal rotation. Similar to the FABER test, this should be considered a generalised test additionally, test positions and definitions of a positive test vary in literature. The Impingement test (Flexion-Adduction-Internal Rotation Test) has a sensitivity of .75.[4]
- Fitzgerald Test. The Fitzgerald test utilizes two different test positions to determine if the patient has an anterior or posterior labral tear. To test for an anterior labral tear, the patient lies supine, then the physical therapist (PT) performs flexion, external rotation, and full abduction of the hip, followed by extending the hip, internal rotation, and adduction. To test for a posterior labral tear, the PT performs passive extension, abduction, external rotation, from the position of full hip flexion, internal rotation, and adduction while the patient is supine. Tests are considered to be positive with pain reproduction with or without an audible click[7][1]. The Fitzgerald test has a sensitivity of .98[7][4].
- Resisted SLR
- Anterior hip impingement test
Medical Management[edit | edit source]
The most common treatment and usually the first step on the treatment ladder is conservative treatment and medication (NSAIDs). When conservative treatment does not resolve symptoms, surgical intervention may be appropriate.
- The most common procedure is excision or debridement of the torn tissue by joint arthroscopy. However, studies have demonstrated mixed post-surgical results. Fargo et al found a significant correlation between outcomes and the presence of arthritis on radiography. Only 21% of patients with detectable arthritis had good results from surgery, compared with 75% of patients without arthritis. Arthroscopic detection of chondromalacia was an even stronger indicator of poor long-term prognosis.[1]
- For a simple tear, surgery involves a bioabsorbable suture anchor being placed over the tear to stabilize the fibrocartilaginous tissue back onto the rim of the acetabulum when the labrum has detached from the bone.
- If the pathology is caused by a malalignment (e.g. Perthes or hip dysplasia), femoral or pelvic osteotomies are considered. A femoral osteotomy is a surgical treatment where the femur is cut and angled differently in an attempt to improve the mechanics of the leg.
- Surgical treatment has been shown to have a short-term improvement in patient-reported outcomes and functional scores post-operatively, however, the long-term outcomes remain unknown. [1][24]
- Repair of the acetabular labral lesion can be performed in either the supine or lateral position. In the supine position, a stand fracture table is used with an oversized personal post to apply traction. The affected hip is placed into slight extension/adduction to allow an approach to the joint. During traction, it is important that there is a minimized pressure in the perineal area to avoid neurologic complications. The procedure is under the guidance of fluoroscopy. If the distraction is obtained a 14 or 16 gauge spinal needle is inserted into the joint to break the vacuum seal and allow further distraction. Three portals are used (the anterolateral, anterior and the distal lateral accessory).
- For repair of a detached labrum, the edges of the tear are delineated and suture anchors are placed on top of the acetabular rim in the area of detachment. If the tear in the labrum has a secure outer rim and is still attached to the acetabulum, a suture in the mid substance of the tear can be used to secure it.[5]
Physical Therapy Management[edit | edit source]
Conservative Rehabilitation[edit | edit source]
When conservative management is unable to control the patient’s symptoms, surgical intervention may be considered.[25]
Post-surgical Rehabilitation[edit | edit source]
Movements that cause stress in the area need to be avoided. The rehabilitation protocol following acetabular labral debridement or repair is divided into four phases.
Phase 1. Initial exercise (week 1-4)[edit | edit source]
The primary goals following an acetabulolabral debridement or repair are to minimize pain and inflammation, and initiate early motion exercises. This phase initially consists of isometric contraction exercises for the hip adductors, abductors, transverse abdominals and extensor muscles. Following a labral debridement, closed-chain activities such as low-level leg press or shuttle can begin with limited resistance.
Weight bearing protocol following a debridement is 50% for 7 to 10 days, and non-weight bearing or toe-touch weight bearing for 3 to 6 weeks in case of a labral repair. Unnecessary hypomobility will limit progress in future phases, thus it is important to ensure that the patient maintains adequate mobility and range during this phase.
Treatment modalities:
- Aquatic therapy is a suitable treatment approach - movement in the water allows for improvement in gait by allowing appropriate loads to be placed on the joint without causing unnecessary stress to the healing tissue. For example, the patient may perform jogging in the water using a flotation device. It is important to know the patient's range of motion precautions, as these may vary in debridement or repair.
- Manual therapy for pain reduction and improvement in joint mobility and proprioception. Considerations include gentle hip joint mobilizations contract-relax stretching for internal and external rotation, long-axis distraction, and assessment of lumbo-sacral mobility.
- Cryotherapy
- Appropriate pain management through medication.
- Gentle stretching of hip muscle groups including piriformis, psoas, quadriceps, hamstring muscles with passive range of motion.
- Stationary bike without resistance, with seat height that limits the hip to less than 90°
- Exercises such as water walking, piriformis stretch, and ankle pumps.
To progress to phase 2, ROM has to be greater or equal to 75%.
Phase 2. Intermediate exercise (week 5-7)[edit | edit source]
The goal of this phase is to continue improving ROM and soft tissue flexibility. Manual therapy should continue with more aggressive mobilization, passive ROM exercises should become more aggressive as needed, for external- and internal rotation.
- Flexibility exercises involving the piriformis, adductor group, psoas/rectus femoris should continue
- Stationary bike with resistance
- Sidestepping with an abductor band for resistance
- Core strengthening such as bridging
- Non-competitive swimming
- Exercises such as wall sits with abductor band, two leg bridging
To progress to the third phase the patient must have a normal gait pattern with no Trendelenburg sign. The patient should have symmetrical and passive ROM measurements with minimal complaints of pain.
Phase 3. Advanced Exercise (week 8-12)[edit | edit source]
- Manual therapy should be performed as needed
- Flexibility and passive ROM interventions should become slightly more aggressive if the limitations persist (if the patient has reached his full ROM or flexibility, terminal stretches should be initiated)
- Strengthening exercises: walking lunges, lunges with trunk rotations, resistant sportcord, walking forward/backwards, plyometric bounding in the water.
- Exercises such as core ball stabilization, golf progression, lunges
To progress to the fourth phase, there must be symmetrical ROM and flexibility of the psoas and piriformis.
Phase 4. Sport-specific training (12-*)[edit | edit source]
- In this phase, it is important to return safely and effectively back to competition or previous activity level.
- Manual therapy, flexibility, and ROM exercises can continue as appropriate.
- It is important that the patient has good muscular endurance, good eccentric muscle control, and the ability to generate power.
- The patient can be given sport-specific exercises and has to have the ability to demonstrate good neuromuscular control of the lower extremity during the activities.
- Exercises such as sport-specific drills, functional testing
The goal during physical therapy of an acetabular labral tear is to optimize the alignment of the hip joint and the precision of joint motion [1]. This can be done by:
- Reducing anteriorly directed forces on the hip by addressing the patterns of recruitment of muscles that control hip motion and by correcting movement patterns during exercises such as hip extension and gait [1].
- Instructing patients to avoid pivoting motions, especially under load, since the acetabulum rotates on a loaded femur, thus increasing force across the labrum [8][1]
So far there has been no research on the efficacy of hip mobilization or manipulation in the treatment of labral disorders. Although it is suggested that the therapy should focus on optimizing the alignment of the hip joint and the precision of joint motion, avoiding pivoting motions and correcting gait patterns.[3]
As these patients have abnormal recruitment patterns of the hip muscles due to the biomechanics of the pathology, treatment should optimize control of these muscles, specifically the hip adductors, deep external rotators, m. gluteus maximus, and m. iliopsoas muscles [1][26]. Additionally, if m. quadriceps femoris and hamstring muscles dominate, this should be corrected, as decreased force contribution from the m. iliopsoas during hip flexion and from the gluteal muscles during active hip extension results in greater anterior hip forces.[27]
Through gait and foot motion analysis, any abnormalities such as knee hyperextension causing hip hyperextension, walking with an externally rotated hip, or stiffness in the subtalar joint can be analysed and can be corrected through taping, orthotics or strengthening [1]. Gait analysis may also uncover decreased hip abduction during both the stance and swing phase, and decreased hip extension during the swing phase -- characteristics that may be part of a hip joint stabilization strategy used by patients to compensate for deficient hip musculature functionality.[28]
Additionally, patients need to be educated regarding modification of functional activities to avoid any positions that cause pain, such as sitting with knees lower than hips or with legs crossed, getting up from a chair by rotating the pelvis on a loaded femur, hyperextending the hip while walking on a treadmill, etc.
After addressing abnormal movement patterns, focused muscle strengthening work and recovery of a normal range of motion, patients eventually need to progress to advanced sensory-motor training and functional exercises, sport-specific if applicable.[26]
The first six weeks post-surgery are usually NWB or TTWB after surgery. Active and active assisted exercises are appropriate in gravity-minimized positions to maintain the motion of the hip. A stationary bike, not a recumbent bicycle, is appropriate; end-range hip flexion should be done passively rather than actively. Currently, rehabilitation protocols are based on surgeon and PT experience and can follow either labral debridement or repair guidelines, depending on the procedure performed, and move through 4 basic phases. The four basic phases follow the general progression of initial exercises, intermediate exercises, advanced exercises and sports-specific training. [5]
Outcome Measures[edit | edit source]
- International Hip Outcome Tool (iHOT)
- Hip and Groin Outcome Score (HAGOS)
- Hip Outcome Score (HOS)
- Harris Hip Score (HHS)
- Nonarthritic Hip Score
- Lower Extremity Functional Scale (LEFS)
- Lequesne Hip Score
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 Lewis C, Sahrmann S. Acetabular labral tears. Physical Therapy. 2006;86(1):110-121.
- ↑ Amber I, Mohan S. Preventing Overdiagnosis of Acetabular Labral "Tears" in 40-Plus-year-old Patients: Shouldn't these be called Labral "Fissures" Instead? Acad Radiol. 2018;25(3):387-390.
- ↑ 3.0 3.1 3.2 3.3 3.4 Schmerl M, Pollard H, Hoskins W. Labral Injuries of the hip: a review of diagnosis and management. J Manipulative Physiol Ther. 2005;28(8):632
- ↑ 4.0 4.1 4.2 Burgess RM, Rushton A, Wright C, Daborn C. The validity and accuracy of clinical diagnostic tests used to detect labral pathology of the hip: A systematic review. Manual Therapy 16 (2011) 318 – 326.
- ↑ 5.0 5.1 5.2 Garrison JC, Osler MT, Singleton SB. Rehabilitation after arthroscopy of an acetabular labral tear. N Amer J of Sports PT. 2007 Nov; 2(4): 241-249
- ↑ Burnett SJ, Della Rocca GJ, Prather H, et al. Clinical Presentation of Patients with tears of the Acetabular Labrum. The Journal of Bone Surgery: Volume 88-A · Number 7 · July 2006 pg 1448 - 1456
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 7.8 Leiboid M, Huijbregts P, Jensen R. Concurrent Criterion-Related Validity of Physical Examination Tests for Hip Labral Lesions: A Systematic Review. The Journal of Manual Manipulative Therapy. [online]. 2008;16(2):E24-41.
- ↑ 8.00 8.01 8.02 8.03 8.04 8.05 8.06 8.07 8.08 8.09 8.10 Groh MM, Herrera J. A comprehensive review of hip labral tears. Current reviews in musculoskeletal medicine. 2009 Jun 1;2(2):105-17.
- ↑ 9.0 9.1 Orbell S, Smith TO. The physiotherapeutic treatment of acetabular labral tears. A systematic review. Adv Physiother. 2011; 13: 153-161.
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 10.6 Heiderscheit B, McClinton S. Evaluation and Management of Hip and Pelvis Injuries. Phys Med Rehabil Clin N Am. 2016;27(1):1-29.
- ↑ 11.0 11.1 McCarthy JC, Noble PC, Schuck MR, et al. The Otto E. Aufranc Award: the role of labral lesions to development of early degenerative hip disease. Clin Orthop 2001;393:25–37.
- ↑ O’Leary JA, Berend K, Vail TP. The relationship between diagnosis and outcome in arthroscopy of the hip. Arthroscopy 2001;17:181–188.
- ↑ 13.0 13.1 Byrd JW. Labral lesions: an elusive source of hip pain case reports and literature review. Arthroscopy 1996;12:603–612.
- ↑ Binningsley D. Tear of the acetabular labrum in an elite athlete. Br J Sports Med 2003;37:84–88.
- ↑ 15.0 15.1 Hase T, Ueo T. Acetabularlabral tear: arthroscopic diagnosis and treatment. Arthroscopy 1999;15:138 –141.
- ↑ Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome: a clinical presentation of dysplasia of the hip. J Bone Joint Surg Br 1991;73:423– 429.
- ↑ Narvani AA, Tsiridis E, Tai CC, Thomas P. Acetabular labrum and its tears. Br J Sports Med 2003;37:207-211.
- ↑ Farjo LA, Glick JM, Sampson TG. Hip arthroscopy for acetabular labral tears. Arthroscopy 1999;15:132–137.
- ↑ 19.0 19.1 Heerey JJ, Kemp JL, Mosler AB, Jones DM, Pizzari T, Souza RB et al. What is the prevalence of imaging-defined intra-articular hip pathologies in people with and without pain? A systematic review and meta-analysis. Br J Sports Med. 2018;52(9):581-593.
- ↑ 20.0 20.1 Chopra A, Grainger AJ, Dube B, Evans R, Hodgson R, Conroy J et al. Comparative reliability and diagnostic performance of conventional 3T magnetic resonance imaging and 1.5T magnetic resonance arthrography for the evaluation of internal derangement of the hip. Eur Radiol. 2018 Mar;28(3):963-971.
- ↑ 21.0 21.1 21.2 Reiman MP, Goode AP, Cook CE, Hölmich P, Thorborg K. Diagnostic accuracy of clinical tests for the diagnosis of hip femoroacetabular impingement/labral tear: a systematic review with meta-analysis. Br J Sports Med. 2015;49(12):811.
- ↑ Martin RL, Irrgang J, Sekiya J. The Diagnostic Accuracy of a Clinical Examination in Determining Intra-articular Hip Pain for Potential Hip Arthroscopy Candidates. The Journal of Arthroscopic and Related Surgery. 2008;(52225):1-6
- ↑ McCarthy JC, Noble P, Schuck M, Alusio FV, Wright J, Lee J. “Acetabular and labral pathology.” In: McCarthy JC, editor. Early hip disorders. New York7 Springer Verlag; 2003. p. 113-33.
- ↑ Ayeni, O. R., Alradwan, H., de Sa, D., & Philippon, M. J. (2014). The hip labrum reconstruction: indications and outcomes—a systematic review. Knee Surgery, Sports Traumatology, Arthroscopy, 22(4), 737-743.
- ↑ Troelsen A, Mechlenburg I, Gelineck J, Bolvig L, Jacobsen S, Søballe K. What is the role of clinical tests and ultrasound in acetabular labral tear diagnostics? Acta Orthop 2009 Jun;80(3):314-8.
- ↑ 26.0 26.1 Yazbek PM, Ovanessian V, Martin RL, Fukuda TY. Nonsurgical treatment of acetabular labrum tears: a case series. J of Ortho Sports PT. 2011 May; 41(5): 346-353
- ↑ Lewis CL, Sahrmann SA, Moran DW. Effect of hip angle on anterior hip force during gait. Gait Posture. 2010 Oct; 32(4): 603-607
- ↑ Kennedy MJ, Lamontagne M, Beaule PE. Femoroacetabular impingement alters hip and pelvic biomechanics during gait. Gait Posture. 30(2009) 41-44