Gluteal Considerations for Patellofemoral Pain: Difference between revisions
(Add columns for Gluteus maximus images) |
(added blurps to images of exercise examples) |
||
| (32 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Jacquie Kieck|Jacquie Kieck]] based on the course by [https://members.physio-pedia.com/course_tutor/claire-robertson/ Claire Robertson]<br> | <div class="editorbox"> '''Original Editor '''- [[User:Jacquie Kieck|Jacquie Kieck]] based on the course by [https://members.physio-pedia.com/course_tutor/claire-robertson/ Claire Robertson]<br> | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== Introduction == | == Introduction == | ||
Patella malalignment is influenced not only by the patella, but also by the position of the [[femur]] and trochlear. The position of the femur and trochlear is altered by the gluteal muscles, | Patella malalignment is influenced not only by the patella, but also by the position of the [[femur]] and trochlear. The position of the femur and trochlear is altered by the gluteal muscles. Thus, it is necessary to assess the gluteal muscles when considering [[Patellofemoral Pain Syndrome|patellofemoral pain]].<ref>Ireland ML, Willson JD, Ballantyne BT, Davis IM. [https://www.jospt.org/doi/epdf/10.2519/jospt.2003.33.11.671 Hip strength in females with and without patellofemoral pain]. Journal of orthopaedic & sports physical therapy. 2003 Nov;33(11):671-6</ref><ref name=":2">Sadler S, Cassidy S, Peterson B, Spink M, Chuter V. [https://link.springer.com/article/10.1186/s12891-019-2833-4 Gluteus medius muscle function in people with and without low back pain: a systematic review]. BMC musculoskeletal disorders. 2019 Dec;20(1):1-7</ref> The clinician should be cognisant that the assessment of the gluteal muscles in patellofemoral pain is not performed in isolation. Patellofemoral pain should be assessed holistically and consider various factors, including local factors around the knee, the whole limb assessment and [[Psychological Basis of Pain|psychosocial factors]],<ref>Crossley KM, van Middelkoop M, Barton CJ, Culvenor AG. Rethinking patellofemoral pain: prevention, management and long-term consequences. Best Practice & Research Clinical Rheumatology. 2019 Feb 1;33(1):48-65.</ref> such as [[Fear Avoidance Model|fear of movement]] and pain catastrophisation.<ref>Uritani D, Kasza J, Campbell PK, Metcalf B, Egerton T. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7183118/pdf/12891_2020_Article_3305.pdf The association between psychological characteristics and physical activity levels in people with knee osteoarthritis: a cross-sectional analysis.] BMC musculoskeletal disorders. 2020 Dec;21(1):1-7</ref> | ||
== Why Do We Need to Consider Each Muscle? == | == Why Do We Need to Consider Each Muscle? == | ||
Understanding the gluteal | Understanding the gluteal muscles' function in each [[Cardinal Planes and Axes of Movement|plane of movement]] is imperative for accurately assessing the performance of this muscle group and its influence on patellofemoral pain. When the clinician can specifically identify the plane of movement in which the dysfunction occurs, as well as isolate the problematic structure, targeted rehabilitation exercises can be prescribed. | ||
== Functional Role of the Gluteal Muscles == | == Functional Role of the Gluteal Muscles == | ||
==== Gluteus Medius as an Abductor in the Frontal Plane ==== | ==== Gluteus Medius as an Abductor in the Frontal Plane ==== | ||
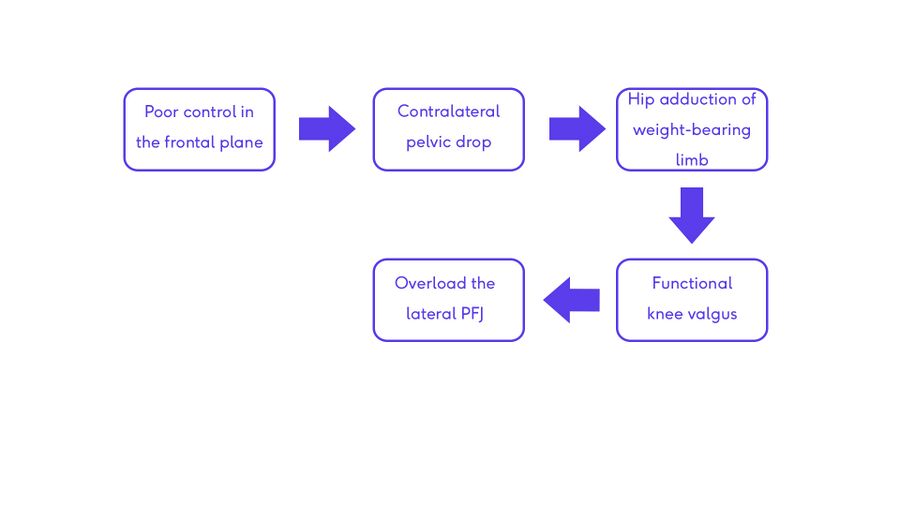
[[Gluteus Medius|Gluteus medius]] acts as an abductor of the hip in the frontal plane. Poor hip abduction control in a single-stance, weight-bearing position | [[Gluteus Medius|Gluteus medius]] acts as an abductor of the hip in the frontal plane. Poor hip abduction control in a single-stance, weight-bearing position leads to contralateral pelvis drop. In this scenario, the weight-bearing limb essentially falls into adduction, causing a functional [[Valgus Knee|valgus]] at the knee. This in turn creates greater load on the lateral patellofemoral joint (PFJ).<ref>Lee TQ, Anzel SH, Bennett KA, Pang D, Kim WC. The influence of fixed rotational deformities of the femur on the patellofemoral contact pressures in human cadaver knees. Clinical orthopaedics and related research. 1994 May 1(302):69-74</ref> | ||
[[File:Flow_chart_of_hip_control_in_the_frontal_plane.jpg|alt=|center|900x900px|thumb|Chart illustrating the impact of poor gluteus medius control on patellofemoral pain.]] | |||
Gluteus medius is assessed in the frontal plane by performing hip abduction against resistance. During the test, it is recommended that resistance against hip abduction is maintained for 10 seconds. By sustaining the resistance applied to the muscle, the tonic performance of the muscle can be assessed rather than the phasic performance (phasic performance is tested in the first couple of seconds of holding a position against resistance). This is important because gluteus medius should act as a postural endurance muscle to stabilise the pelvis. To recap [[Muscle Fibre Types|muscle fibre types]]; type 1 muscle fibres produce low power contractions over longer periods and are slow to fatigue (tonic muscle performance), type 2 muscle fibres have fast contractions and can fatigue more quickly (phasic muscle performance). | |||
Gluteus | Gluteus medius can also be assessed in a weight-bearing position. The assessor looks at the ability of the client to control their pelvis as they perform a contralateral hip drop when standing on a step. This position allows for the concentric and eccentric assessment of the gluteus medius. This position is also effective for strengthening this muscle.<ref>Moore D, Semciw AI, Pizzari T. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7727410/ A systematic review and meta-analysis of common therapeutic exercises that generate highest muscle activity in the gluteus medius and gluteus minimus segments]. International Journal of Sports Physical Therapy. 2020 Dec;15(6):856.</ref> | ||
==== Gluteus Medius as an External Rotator in the Horizontal Plane ==== | ==== Gluteus Medius as an External Rotator in the Horizontal Plane ==== | ||
The posterior fibres of gluteus medius are active as the primary external rotator of the hip at 0º to 20º of hip flexion. From 20º to 50º of hip flexion, the posterior fibres of gluteus medius are still active. Above 50º of hip flexion | The posterior fibres of gluteus medius are active as the primary external rotator of the hip at 0º to 20º of hip flexion. From 20º to 50º of hip flexion, the posterior fibres of gluteus medius are still active. Above 50º of hip flexion, [[Gluteus Maximus|gluteus maximus]] is the primary external rotator. To test gluteus medius, resistance must be given against hip external rotation when the hip is in 0º to 20º of flexion. | ||
{| class="wikitable" | {| class="wikitable" | ||
|'''Hip Flexion''' | |'''Hip Flexion''' | ||
| Line 35: | Line 29: | ||
|- | |- | ||
|'''Primary external rotator of the hip''' | |'''Primary external rotator of the hip''' | ||
|Gluteus | |Gluteus medius | ||
|Gluteus | |Gluteus medius is still active | ||
|Gluteus | |Gluteus maximus | ||
|} | |} | ||
==== Gluteus Maximus as an External Rotator in the Horizontal Plane ==== | ==== Gluteus Maximus as an External Rotator in the Horizontal Plane ==== | ||
Gluteus maximus externally rotates the hip when the hip is flexed. Testing of the gluteus maximus should be performed by providing resistance against external rotation of the hip when | Gluteus maximus externally rotates the hip when the hip is flexed. Testing of the gluteus maximus should be performed by providing resistance against external rotation of the hip when it is flexed. It is recommended to sustain the hold against external rotation in this position for ten seconds to test the tonic action of the muscle. | ||
== Rehabilitation Exercises == | == Rehabilitation Exercises == | ||
=== Gluteus Medius in the Frontal Plane (Hip Abduction) === | === Gluteus Medius in the Frontal Plane (Hip Abduction) === | ||
< | Below are some examples of hip abduction rehabilitation exercises:<gallery widths="250px" heights="350px"> | ||
File: Screenshot 2022-05-26 at 20.24.31.png|Hip Abduction in Standing | |||
File: Screenshot 2022-05-26 at 20.21.45.png|Hip Abduction Against Resistance in Standing | |||
File: Screenshot 2022-05-26 at 20.31.27.png|Hip Abduction in Sidelying </gallery> | |||
=== Gluteus Medius in the Horizontal Plane (Hip Lateral Rotation at <20º of Hip Flexion) === | === Gluteus Medius in the Horizontal Plane (Hip Lateral Rotation at <20º of Hip Flexion) === | ||
<gallery widths=" | See below examples of hip lateral rotation at <20° of hip flexion rehabilitation exercises:<gallery widths="250px" heights="350px"> | ||
File: External hip rotation in standing - Claire's own image.jpg|External Rotation of the Hip in Standing | |||
File: Hip External Rotation in Shallow hip flexion.png|External Rotation of the Hip in Shallow Hip Flexion | |||
</gallery> | </gallery> | ||
=== Gluteus Maximus in the Horizontal Plane (Hip | === Gluteus Maximus in the Horizontal Plane (Hip External Rotation at >50º of Hip Flexion) === | ||
< | See the examples below for hip external rotation at >50° of hip flexion:<gallery widths="250px" heights="350px"> | ||
File: Clam with band in deep hip flexion - Claire's own image.jpg|External Rotation of the Hip in 90º Hip Flexion | |||
File: External Hip Rotation Eccentric Control in Sitting - Claire's Own Image.jpg|External Rotation of the Hip in 90º Hip Flexion/Sitting | |||
</gallery> | |||
=== Consider the Bridge Exercise === | === Consider the Bridge Exercise === | ||
| Line 71: | Line 62: | ||
At the beginning of the bridge exercise, the hip is in deep hip flexion. This means that the gluteus maximus is most active as an external rotator of the hip. As the hip moves out of hip flexion into a more neutral position, gluteus maximus continues to work as a hip extensor, but the posterior fibres of gluteus medius become more prominent as a rotator. | At the beginning of the bridge exercise, the hip is in deep hip flexion. This means that the gluteus maximus is most active as an external rotator of the hip. As the hip moves out of hip flexion into a more neutral position, gluteus maximus continues to work as a hip extensor, but the posterior fibres of gluteus medius become more prominent as a rotator. | ||
Progressions of the bridge exercise to make it more challenging, include lifting the unaffected leg (i.e. perform a one-legged bridge) and adding a weight placed on the person's abdomen. | |||
=== Functional Role with Different Activities === | === Functional Role with Different Activities === | ||
==== Gait ==== | ==== Gait ==== | ||
During gait, gluteus maximus works eccentrically to control rotation<ref>Preece SJ, Graham-Smith P, Nester CJ, Howard D, Hermens H, Herrington L, Bowker P. The influence of gluteus maximus on transverse plane tibial rotation. Gait & posture. 2008 May 1;27(4):616-21.</ref> | During [[gait]], gluteus maximus works eccentrically to control rotation at the hip.<ref>Preece SJ, Graham-Smith P, Nester CJ, Howard D, Hermens H, Herrington L, Bowker P. The influence of gluteus maximus on transverse plane tibial rotation. Gait & posture. 2008 May 1;27(4):616-21.</ref> After heel strike, to around 24% into weight bearing, the femur and the tibia internally rotate. This is an expected movement. However, this internal rotation should only occur for a short period. Excessive internal rotation ultimately results in excessive loading of the lateral patellofemoral joint. Mirror gait retraining<ref>Richard W. Willy, John P. Scholz, Irene S. Davis. | ||
Mirror gait retraining for the treatment of patellofemoral pain in female runners. Clinical Biomechanics 2012; 27: 1045-1051.</ref> can increase patient awareness of this movement and facilitate correction of faulty biomechanics. | |||
=== Running === | === Running === | ||
Increased running speed is associated with increased movement in the frontal plane i.e. contralateral | Increased running speed is associated with increased movement in the frontal plane i.e. contralateral pelvis drop with corresponding hip adduction and resultant knee valgus. This increases the load on the lateral patellofemoral joint.<ref name=":0">Robertson, C. [https://members.physio-pedia.com/learn/patellofemoral-joint-programme/ Gluteal Considerations in the Management of Patellofemoral Pain]. Course. Plus. 2022.</ref> Bramah et al.<ref name=":3">Bramah C, Preece SJ, Gill N, Herrington L. [https://journals.sagepub.com/doi/full/10.1177/0363546518793657 Is there a pathological gait associated with common soft tissue running injuries?]. The American journal of sports medicine. 2018 Oct;46(12):3023-31.</ref> demonstrated that for every 1° increase in pelvic drop during running, there was an 80% increase in the likelihood of being classified as injured. The same study by Bramah et al.<ref name=":3" /> showed that contralateral pelvis drop appeared to be the most strongly related variable to common running-related injuries, including patellofemoral pain. | ||
'''Video: Excessive hip adduction''' | |||
{{#ev:youtube|QTC9hEu0pQQ}} | |||
<ref>Enhance RunningEnhance running: excessive hip adduction & internal rotation. Available from https://www.youtube.com/watch?v=QTC9hEu0pQQ&t=2s Accessed on 05/06/2022</ref> | |||
When rehabilitating a patient with patellofemoral pain where lack of control in the frontal plane is a contributing factor, it is useful to consider running speed. The clinician can suggest reducing running speed to offload / reduce load on the patellofemoral joint as an alternative to stopping sport altogether. In team sports, a change of position on the court / field to a position where the patient will not be required to run as fast can be helpful.<ref name=":0" /> | |||
=== Landing From a Jump === | === Landing From a Jump === | ||
It has been shown that jump-landing kinematics are affected by lower limb injuries, including patellofemoral pain.<ref name=":1">De Bleecker C, Vermeulen S, De Blaiser C, Willems T, De Ridder R, Roosen P. Relationship between jump-landing kinematics and lower extremity overuse injuries in physically active populations: a systematic review and meta-analysis. Sports Medicine. 2020 Aug;50(8):1515-32.</ref> They are also affected by gluteal muscle strength, which influences dynamic knee valgus.<ref>Neamatallah Z, Herrington L, Jones R. An investigation into the role of gluteal muscle strength and EMG activity in controlling HIP and knee motion during landing tasks. Physical Therapy in Sport. 2020 May 1;43:230-5.</ref> Similarly, a systematic review and meta-analysis by DeBleecker et al.<ref name=":1" /> showed some evidence for the association of impaired jump-landing kinematics and lower extremity overuse injuries. This indicates that '''patellofemoral pain influences jump-landing kinematics, ''and'' that jump-landing kinematics is influenced by patellofemoral pain'''. Hence, it is important to assess jump-landing kinematics as a prevention strategy for lower extremity injuries, and to assess jump-landing kinematics in a person experiencing a lower extremity injury. For clients with patellofemoral pain who participate in sports that require jumping, it is important to assess the jump-landing kinematics to identify poor gluteal control as a possible contributing factor. Psychosocial factors such as [[kinesiophobia]] should also be considered when assessing landing from a jump. | |||
== Muscle Inhibition == | == Muscle Inhibition == | ||
A history of low back pain<ref>Bullock-Saxton JE, Janda V, Bullock MI. Reflex activation of gluteal muscles in walking. An approach to restoration of muscle function for patients with low-back pain. Spine. 1993 May 1;18(6):704-8 | A history of low back pain<ref name=":2" /><ref>Bullock-Saxton JE, Janda V, Bullock MI. Reflex activation of gluteal muscles in walking. An approach to restoration of muscle function for patients with low-back pain. Spine. 1993 May 1;18(6):704-8.</ref> or ankle injuries<ref>Beckman SM, Buchanan TS. Ankle inversion injury and hypermobility: effect on hip and ankle muscle electromyography onset latency. Archives of physical medicine and rehabilitation. 1995 Dec 1;76(12):1138-43.</ref> have been shown to influence gluteal function. Low back pain can inhibit gluteus maximus, and ankle inversion injuries are related to gluteus medius inhibition. Because the relevance of the gluteal muscles in patellofemoral joint pain has been clearly established, it is important to establish if the patient presenting with patellofemoral pain has a history of low back pain or ankle injury. | ||
== References | == References == | ||
<references /> | <references /> | ||
[[Category:Knee - Assessment and Examination]] | |||
[[Category:Knee - Conditions]] | |||
[[Category:Musculoskeletal/Orthopaedics]] | |||
[[Category:Course Pages]] | |||
[[Category:Plus Content]] | |||
Latest revision as of 11:16, 23 October 2023
Top Contributors - Jacquie Kieck, Wanda van Niekerk, Jess Bell, Kim Jackson and Tarina van der Stockt
Introduction[edit | edit source]
Patella malalignment is influenced not only by the patella, but also by the position of the femur and trochlear. The position of the femur and trochlear is altered by the gluteal muscles. Thus, it is necessary to assess the gluteal muscles when considering patellofemoral pain.[1][2] The clinician should be cognisant that the assessment of the gluteal muscles in patellofemoral pain is not performed in isolation. Patellofemoral pain should be assessed holistically and consider various factors, including local factors around the knee, the whole limb assessment and psychosocial factors,[3] such as fear of movement and pain catastrophisation.[4]
Why Do We Need to Consider Each Muscle?[edit | edit source]
Understanding the gluteal muscles' function in each plane of movement is imperative for accurately assessing the performance of this muscle group and its influence on patellofemoral pain. When the clinician can specifically identify the plane of movement in which the dysfunction occurs, as well as isolate the problematic structure, targeted rehabilitation exercises can be prescribed.
Functional Role of the Gluteal Muscles[edit | edit source]
Gluteus Medius as an Abductor in the Frontal Plane[edit | edit source]
Gluteus medius acts as an abductor of the hip in the frontal plane. Poor hip abduction control in a single-stance, weight-bearing position leads to contralateral pelvis drop. In this scenario, the weight-bearing limb essentially falls into adduction, causing a functional valgus at the knee. This in turn creates greater load on the lateral patellofemoral joint (PFJ).[5]
Gluteus medius is assessed in the frontal plane by performing hip abduction against resistance. During the test, it is recommended that resistance against hip abduction is maintained for 10 seconds. By sustaining the resistance applied to the muscle, the tonic performance of the muscle can be assessed rather than the phasic performance (phasic performance is tested in the first couple of seconds of holding a position against resistance). This is important because gluteus medius should act as a postural endurance muscle to stabilise the pelvis. To recap muscle fibre types; type 1 muscle fibres produce low power contractions over longer periods and are slow to fatigue (tonic muscle performance), type 2 muscle fibres have fast contractions and can fatigue more quickly (phasic muscle performance).
Gluteus medius can also be assessed in a weight-bearing position. The assessor looks at the ability of the client to control their pelvis as they perform a contralateral hip drop when standing on a step. This position allows for the concentric and eccentric assessment of the gluteus medius. This position is also effective for strengthening this muscle.[6]
Gluteus Medius as an External Rotator in the Horizontal Plane[edit | edit source]
The posterior fibres of gluteus medius are active as the primary external rotator of the hip at 0º to 20º of hip flexion. From 20º to 50º of hip flexion, the posterior fibres of gluteus medius are still active. Above 50º of hip flexion, gluteus maximus is the primary external rotator. To test gluteus medius, resistance must be given against hip external rotation when the hip is in 0º to 20º of flexion.
| Hip Flexion | 0º - 20º | 20º - 50º | >50º |
| Primary external rotator of the hip | Gluteus medius | Gluteus medius is still active | Gluteus maximus |
Gluteus Maximus as an External Rotator in the Horizontal Plane[edit | edit source]
Gluteus maximus externally rotates the hip when the hip is flexed. Testing of the gluteus maximus should be performed by providing resistance against external rotation of the hip when it is flexed. It is recommended to sustain the hold against external rotation in this position for ten seconds to test the tonic action of the muscle.
Rehabilitation Exercises[edit | edit source]
Gluteus Medius in the Frontal Plane (Hip Abduction)[edit | edit source]
Below are some examples of hip abduction rehabilitation exercises:
Gluteus Medius in the Horizontal Plane (Hip Lateral Rotation at <20º of Hip Flexion)[edit | edit source]
See below examples of hip lateral rotation at <20° of hip flexion rehabilitation exercises:
Gluteus Maximus in the Horizontal Plane (Hip External Rotation at >50º of Hip Flexion)[edit | edit source]
See the examples below for hip external rotation at >50° of hip flexion:
Consider the Bridge Exercise[edit | edit source]
At the beginning of the bridge exercise, the hip is in deep hip flexion. This means that the gluteus maximus is most active as an external rotator of the hip. As the hip moves out of hip flexion into a more neutral position, gluteus maximus continues to work as a hip extensor, but the posterior fibres of gluteus medius become more prominent as a rotator.
Progressions of the bridge exercise to make it more challenging, include lifting the unaffected leg (i.e. perform a one-legged bridge) and adding a weight placed on the person's abdomen.
Functional Role with Different Activities[edit | edit source]
Gait[edit | edit source]
During gait, gluteus maximus works eccentrically to control rotation at the hip.[7] After heel strike, to around 24% into weight bearing, the femur and the tibia internally rotate. This is an expected movement. However, this internal rotation should only occur for a short period. Excessive internal rotation ultimately results in excessive loading of the lateral patellofemoral joint. Mirror gait retraining[8] can increase patient awareness of this movement and facilitate correction of faulty biomechanics.
Running[edit | edit source]
Increased running speed is associated with increased movement in the frontal plane i.e. contralateral pelvis drop with corresponding hip adduction and resultant knee valgus. This increases the load on the lateral patellofemoral joint.[9] Bramah et al.[10] demonstrated that for every 1° increase in pelvic drop during running, there was an 80% increase in the likelihood of being classified as injured. The same study by Bramah et al.[10] showed that contralateral pelvis drop appeared to be the most strongly related variable to common running-related injuries, including patellofemoral pain.
Video: Excessive hip adduction
When rehabilitating a patient with patellofemoral pain where lack of control in the frontal plane is a contributing factor, it is useful to consider running speed. The clinician can suggest reducing running speed to offload / reduce load on the patellofemoral joint as an alternative to stopping sport altogether. In team sports, a change of position on the court / field to a position where the patient will not be required to run as fast can be helpful.[9]
Landing From a Jump[edit | edit source]
It has been shown that jump-landing kinematics are affected by lower limb injuries, including patellofemoral pain.[12] They are also affected by gluteal muscle strength, which influences dynamic knee valgus.[13] Similarly, a systematic review and meta-analysis by DeBleecker et al.[12] showed some evidence for the association of impaired jump-landing kinematics and lower extremity overuse injuries. This indicates that patellofemoral pain influences jump-landing kinematics, and that jump-landing kinematics is influenced by patellofemoral pain. Hence, it is important to assess jump-landing kinematics as a prevention strategy for lower extremity injuries, and to assess jump-landing kinematics in a person experiencing a lower extremity injury. For clients with patellofemoral pain who participate in sports that require jumping, it is important to assess the jump-landing kinematics to identify poor gluteal control as a possible contributing factor. Psychosocial factors such as kinesiophobia should also be considered when assessing landing from a jump.
Muscle Inhibition[edit | edit source]
A history of low back pain[2][14] or ankle injuries[15] have been shown to influence gluteal function. Low back pain can inhibit gluteus maximus, and ankle inversion injuries are related to gluteus medius inhibition. Because the relevance of the gluteal muscles in patellofemoral joint pain has been clearly established, it is important to establish if the patient presenting with patellofemoral pain has a history of low back pain or ankle injury.
References[edit | edit source]
- ↑ Ireland ML, Willson JD, Ballantyne BT, Davis IM. Hip strength in females with and without patellofemoral pain. Journal of orthopaedic & sports physical therapy. 2003 Nov;33(11):671-6
- ↑ 2.0 2.1 Sadler S, Cassidy S, Peterson B, Spink M, Chuter V. Gluteus medius muscle function in people with and without low back pain: a systematic review. BMC musculoskeletal disorders. 2019 Dec;20(1):1-7
- ↑ Crossley KM, van Middelkoop M, Barton CJ, Culvenor AG. Rethinking patellofemoral pain: prevention, management and long-term consequences. Best Practice & Research Clinical Rheumatology. 2019 Feb 1;33(1):48-65.
- ↑ Uritani D, Kasza J, Campbell PK, Metcalf B, Egerton T. The association between psychological characteristics and physical activity levels in people with knee osteoarthritis: a cross-sectional analysis. BMC musculoskeletal disorders. 2020 Dec;21(1):1-7
- ↑ Lee TQ, Anzel SH, Bennett KA, Pang D, Kim WC. The influence of fixed rotational deformities of the femur on the patellofemoral contact pressures in human cadaver knees. Clinical orthopaedics and related research. 1994 May 1(302):69-74
- ↑ Moore D, Semciw AI, Pizzari T. A systematic review and meta-analysis of common therapeutic exercises that generate highest muscle activity in the gluteus medius and gluteus minimus segments. International Journal of Sports Physical Therapy. 2020 Dec;15(6):856.
- ↑ Preece SJ, Graham-Smith P, Nester CJ, Howard D, Hermens H, Herrington L, Bowker P. The influence of gluteus maximus on transverse plane tibial rotation. Gait & posture. 2008 May 1;27(4):616-21.
- ↑ Richard W. Willy, John P. Scholz, Irene S. Davis. Mirror gait retraining for the treatment of patellofemoral pain in female runners. Clinical Biomechanics 2012; 27: 1045-1051.
- ↑ 9.0 9.1 Robertson, C. Gluteal Considerations in the Management of Patellofemoral Pain. Course. Plus. 2022.
- ↑ 10.0 10.1 Bramah C, Preece SJ, Gill N, Herrington L. Is there a pathological gait associated with common soft tissue running injuries?. The American journal of sports medicine. 2018 Oct;46(12):3023-31.
- ↑ Enhance RunningEnhance running: excessive hip adduction & internal rotation. Available from https://www.youtube.com/watch?v=QTC9hEu0pQQ&t=2s Accessed on 05/06/2022
- ↑ 12.0 12.1 De Bleecker C, Vermeulen S, De Blaiser C, Willems T, De Ridder R, Roosen P. Relationship between jump-landing kinematics and lower extremity overuse injuries in physically active populations: a systematic review and meta-analysis. Sports Medicine. 2020 Aug;50(8):1515-32.
- ↑ Neamatallah Z, Herrington L, Jones R. An investigation into the role of gluteal muscle strength and EMG activity in controlling HIP and knee motion during landing tasks. Physical Therapy in Sport. 2020 May 1;43:230-5.
- ↑ Bullock-Saxton JE, Janda V, Bullock MI. Reflex activation of gluteal muscles in walking. An approach to restoration of muscle function for patients with low-back pain. Spine. 1993 May 1;18(6):704-8.
- ↑ Beckman SM, Buchanan TS. Ankle inversion injury and hypermobility: effect on hip and ankle muscle electromyography onset latency. Archives of physical medicine and rehabilitation. 1995 Dec 1;76(12):1138-43.