Functional Reach Test (FRT): Difference between revisions
No edit summary |
No edit summary |
||
| (29 intermediate revisions by 7 users not shown) | |||
| Line 5: | Line 5: | ||
</div> | </div> | ||
== Objective | == Objective == | ||
Functional Reach Test (FRT) is a clinical outcome measure and assessment tool for ascertaining dynamic [[balance]] in in simple task. | |||
Functional Reach Test (FRT) is a clinical outcome measure and assessment tool for ascertaining dynamic [[balance]] in | * In standing, measures the distance between the length of an outstretched arm in a maximal forward reach, while maintaining a fixed [[Base of Support|base of support.]] | ||
* This information is correlated with [[Falls|risk of falling]] | |||
* A number of factors exert a major influence on this evaluation: Research revealed that movement strategy and reduced spinal flexibility both affect reach distance.<ref>Schenkman M, Morey M, Kuchibhatla M. Spinal flexibility and balance control among community-dwelling adults with and without Parkinson's. J Gerontol A Biol Sci Med Sci. 2000;55(8):M441-445. | |||
</ref> | |||
== Development == | |||
In 1990, Pamela Duncan and colleagues first developed the Functional Reach test. It is a quick, single-task, dynamic test that is used to predicting falls in older adults. This test measures the margin of stability along with the ability to measure balance during a functional task. | |||
== Intended Population == | == Intended Population == | ||
* FRT was made to predict fall risk in the [[Older People - An Introduction|elderly]] and [[Frail Elderly: The Physiotherapist's Role in Preventing Hospital Admission|Frail]] adult<ref name=":0">Duncan PW, Weiner DK, Chandler J, Studenski S. Functional reach: a new clinical measure of balance.J Gerontol. 1990;45(6):M192-197.</ref><ref name=":1">Weiner DK, Duncan PW, Chandler J, Studenski SA. Functional reach: a marker of physical frailty. J Am Geriatr Soc. 1992;40(3):203-207.</ref> | |||
* It is one of the 4 tests used in the [[The Balance Outcome Measure for Elder Rehabilitation (BOOMER)]] | |||
== Set up == | |||
== | |||
* A yardstick and duck tap will be needed for the assessment. The yardstick should be fixed to the wall at the level of the patient’s acromion. | |||
== Method of Use == | |||
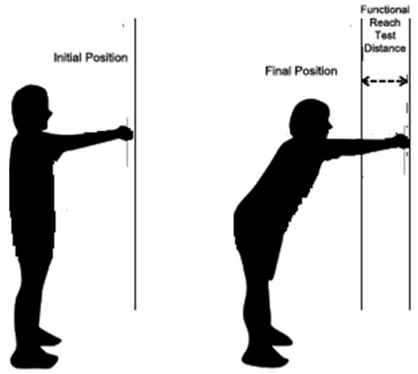
* The patient is instructed to stand next to, but not touching, a wall and position the arm that is closer to the wall at 90 degrees of shoulder flexion with a closed fist. | |||
* The assessor records the starting position at the 3rd metacarpal head on the yardstick. | |||
* Instruct the patient to “Reach as far as you can forward without taking a step.” | |||
* The location of the 3rd metacarpal is recorded. | |||
* Scores are determined by assessing the difference between the start and end position is the reach distance, usually measured in inches. | |||
* Three trials are done and the average of the last two is noted<ref>[https://www.sralab.org/sites/default/files/2017-06/5Hgjkv-Functional%20Reach%20Test.pdf FRT] Available from:https://www.sralab.org/sites/default/files/2017-06/5Hgjkv-Functional%20Reach%20Test.pdf (last accessed 16.10.2020)</ref> | |||
[[File:FRT .webp|thumb|418x418px|Functional Reach Test <ref>Ivan Miguel Pires, Garcia NM, Eftim Zdravevski. Measurement of Results of Functional Reach Test with Sensors: A Systematic Review. Electronics [Internet]. 2020 Jun 30 [cited 2024 Feb 6];9(7):1078–8. Available from: <nowiki>https://www.mdpi.com/2079-9292/9/7/1078</nowiki> | |||
</ref> |center]] | |||
{{#ev:youtube|https://youtu.be/_aJqJzt-U2s?si=5T4RRqUhHCiuljQk}} | |||
== '''Criteria to stop the test''' == | |||
The patient’s feet lifted up from the floor or they fell forward. Most patients fall forward with this test. The therapist should guard from the front as that is the direction that you reach forward. | The patient’s feet lifted up from the floor or they fell forward. Most patients fall forward with this test. The therapist should guard from the front as that is the direction that you reach forward. | ||
Reduced ability to reach has shown increases in future [[Falls and Traumatic Brain Injury|falls]] with odds ratios of 8.2 if unable to reach at all and 4 if able to reach < 15.2cm<ref name=":2">Duncan PW, Studenski S, Chandler J, Prescott B. Functional reach: predictive validity in a sample of elderly male veterans. Gerontol. 1992;47(3):M93-98.</ref> | Reduced ability to reach has shown increases in future [[Falls and Traumatic Brain Injury|falls]] with odds ratios of 8.2 if unable to reach at all and 4 if able to reach < 15.2cm<ref name=":2">Duncan PW, Studenski S, Chandler J, Prescott B. Functional reach: predictive validity in a sample of elderly male veterans. Gerontol. 1992;47(3):M93-98.</ref> | ||
=== | == Measurement Interpretation: == | ||
* '''10”/25 cm or greater:''' Low risk of falls; | |||
* '''6”/15cm to 10”/25cm''' Risk of falling is 2x greater than normal; | |||
* '''6”/15cm or less''' Risk of falling is 4x greater than normal; | |||
* '''Unwilling to reach:''' Risk of falling is 8x greater than normal<ref>[http://functionalpathways.com/intranet-files/Standardized_Test_Reference_Card_Template.pdf Standardized_Test_Reference_Card_Template] Available from:http://functionalpathways.com/intranet-files/Standardized_Test_Reference_Card_Template.pdf (last accessed 16.10.2020)</ref><ref name=":0" /> | |||
== Functional Reach Norm == | |||
{| class="wikitable" | |||
|+'''Functional Reach Norms''' | |||
!Age | |||
!Men | |||
!Women | |||
|- | |||
|20-40 | |||
|16.73 inches | |||
|14.64 inches | |||
|- | |||
|41-69 | |||
|14.98 inches | |||
|13.81 inches | |||
|- | |||
|70-87 | |||
|13.15 inches | |||
|10.47 inches | |||
|} | |||
Intra-class correlations for the other tests ranged from 0.93 to 0.99. All the tests showed significant correlations with the appropriate comparator tests (r=0.32-0.74 p≤0.05) | == Evidence == | ||
'''Reliability'''<ref name=":0" /><ref name=":2" /> | |||
Test-retest reliability r = 0.89 | * The ordinal level tests (supported sitting and standing balance and static tandem standing tests) showed 100% agreement in all aspects of reliability. | ||
* Intra-class correlations for the other tests ranged from 0.93 to 0.99. All the tests showed significant correlations with the appropriate comparator tests (r=0.32-0.74 p≤0.05) | |||
Inter-rater agreement on reach measurement = 0.98 | * Test-retest reliability r = 0.89 | ||
* Inter-rater agreement on reach measurement = 0.98 | |||
'''Validity''' | |||
Eagle et al.<ref name=":3">Eagle JD, Salama S, Whitman D, Evans LA, Ho E, Olde J. Comparison of three instruments in predicting accidental falls in selected inpatients in a general teaching hospital. Journal of Gerontology Nursing. 1999; 25(7): 40-45.</ref> found out the following: | Eagle et al.<ref name=":3">Eagle JD, Salama S, Whitman D, Evans LA, Ho E, Olde J. Comparison of three instruments in predicting accidental falls in selected inpatients in a general teaching hospital. Journal of Gerontology Nursing. 1999; 25(7): 40-45.</ref> found out the following: | ||
* Sensitivity | * Sensitivity = 76% | ||
* Accuracy | * Accuracy = 46% | ||
* | * Specificity = 34% | ||
* Positive Predictive Value = 33% | |||
* Negative Predictive Value = 77% | |||
* Positive Predictive Value | |||
* Negative Predictive Value | |||
Some research found that decreased spinal flexibility and the movement strategy affects the distance reached and also question the ability of FRT to differentiate elderly non-fallers and fallers<ref>Wernick-Robinson M, Krebs DE, Giorgetti MM. Functional reach: Does it really measure dynamic balance? Archives of Physical Medicine and Rehabilitation. 1999; 80(3): 262 - 269 | Some research found that decreased spinal flexibility and the movement strategy affects the distance reached and also question the ability of FRT to differentiate elderly non-fallers and fallers<ref>Wernick-Robinson M, Krebs DE, Giorgetti MM. Functional reach: Does it really measure dynamic balance? Archives of Physical Medicine and Rehabilitation. 1999; 80(3): 262 - 269 | ||
</ref><ref>Wallmann HW. Comparison of elderly nonfallers and fallers on performance measures of functional reach, sensory organization, and limits of stability.J Gerontol A Biol Sci Med Sci. 2001;56(9):M580-583.</ref>. | </ref><ref>Wallmann HW. Comparison of elderly nonfallers and fallers on performance measures of functional reach, sensory organization, and limits of stability.J Gerontol A Biol Sci Med Sci. 2001;56(9):M580-583.</ref>.Rresearch also noted that trunk mobility has a greater contribution to the test than the cenere of pressure displacement. <ref>Jonsson E, Henriksson M, Hirschfeld H. Does the functional reach test reflect stability limits in elderly people? J Rehabil Med. 2003;35(1):26-30. | ||
</ref> | </ref> | ||
'''Responsiveness''' | |||
FRT increased to 28 cm from 18 cm in 22 community-dwelling adults with knee [[osteoarthritis]] following a 10weeks [[Aquatherapy|aquatic exercise program]] under physiotherapist | |||
FRT increased to 28 cm from 18 cm in 22 community-dwelling adults with knee [[osteoarthritis]] following a 10weeks [[Aquatherapy|aquatic exercise program]] under the guidance of a physiotherapist.<ref>Lau MC, Lam JK, Siu E, Fung CS, Li KT, Lam MW. Physiotherapist-designed aquatic exercise programme for community-dwelling elders with osteoarthritis of the knee: a Hong Kong pilot study. Hong Kong Med J. 2014;20(1):16-23. | |||
</ref> | </ref> | ||
| Line 76: | Line 102: | ||
[[Category:Balance]] | [[Category:Balance]] | ||
[[Category:Falls]] | [[Category:Falls]] | ||
[[Category: | [[Category:Neurological - Outcome Measures]] | ||
[[Category:Older People/Geriatrics]] | [[Category:Older People/Geriatrics]] | ||
[[Category:Older People/Geriatrics - Outcome Measures]] | |||
[[Category:Balance - Special Tests]] | |||
Latest revision as of 08:32, 6 February 2024
Original Editor - Evan Thomas
Top Contributors - Tolulope Adeniji, Uchechukwu Chukwuemeka, Kim Jackson, Lucinda hampton, Momina Khalid, Admin, Rachael Lowe, Evan Thomas and Lauren Lopez
Objective[edit | edit source]
Functional Reach Test (FRT) is a clinical outcome measure and assessment tool for ascertaining dynamic balance in in simple task.
- In standing, measures the distance between the length of an outstretched arm in a maximal forward reach, while maintaining a fixed base of support.
- This information is correlated with risk of falling
- A number of factors exert a major influence on this evaluation: Research revealed that movement strategy and reduced spinal flexibility both affect reach distance.[1]
Development[edit | edit source]
In 1990, Pamela Duncan and colleagues first developed the Functional Reach test. It is a quick, single-task, dynamic test that is used to predicting falls in older adults. This test measures the margin of stability along with the ability to measure balance during a functional task.
Intended Population[edit | edit source]
- FRT was made to predict fall risk in the elderly and Frail adult[2][3]
- It is one of the 4 tests used in the The Balance Outcome Measure for Elder Rehabilitation (BOOMER)
Set up[edit | edit source]
- A yardstick and duck tap will be needed for the assessment. The yardstick should be fixed to the wall at the level of the patient’s acromion.
Method of Use[edit | edit source]
- The patient is instructed to stand next to, but not touching, a wall and position the arm that is closer to the wall at 90 degrees of shoulder flexion with a closed fist.
- The assessor records the starting position at the 3rd metacarpal head on the yardstick.
- Instruct the patient to “Reach as far as you can forward without taking a step.”
- The location of the 3rd metacarpal is recorded.
- Scores are determined by assessing the difference between the start and end position is the reach distance, usually measured in inches.
- Three trials are done and the average of the last two is noted[4]
Criteria to stop the test[edit | edit source]
The patient’s feet lifted up from the floor or they fell forward. Most patients fall forward with this test. The therapist should guard from the front as that is the direction that you reach forward.
Reduced ability to reach has shown increases in future falls with odds ratios of 8.2 if unable to reach at all and 4 if able to reach < 15.2cm[6]
Measurement Interpretation:[edit | edit source]
- 10”/25 cm or greater: Low risk of falls;
- 6”/15cm to 10”/25cm Risk of falling is 2x greater than normal;
- 6”/15cm or less Risk of falling is 4x greater than normal;
- Unwilling to reach: Risk of falling is 8x greater than normal[7][2]
Functional Reach Norm[edit | edit source]
| Age | Men | Women |
|---|---|---|
| 20-40 | 16.73 inches | 14.64 inches |
| 41-69 | 14.98 inches | 13.81 inches |
| 70-87 | 13.15 inches | 10.47 inches |
Evidence[edit | edit source]
- The ordinal level tests (supported sitting and standing balance and static tandem standing tests) showed 100% agreement in all aspects of reliability.
- Intra-class correlations for the other tests ranged from 0.93 to 0.99. All the tests showed significant correlations with the appropriate comparator tests (r=0.32-0.74 p≤0.05)
- Test-retest reliability r = 0.89
- Inter-rater agreement on reach measurement = 0.98
Validity
Eagle et al.[8] found out the following:
- Sensitivity = 76%
- Accuracy = 46%
- Specificity = 34%
- Positive Predictive Value = 33%
- Negative Predictive Value = 77%
Some research found that decreased spinal flexibility and the movement strategy affects the distance reached and also question the ability of FRT to differentiate elderly non-fallers and fallers[9][10].Rresearch also noted that trunk mobility has a greater contribution to the test than the cenere of pressure displacement. [11]
Responsiveness
FRT increased to 28 cm from 18 cm in 22 community-dwelling adults with knee osteoarthritis following a 10weeks aquatic exercise program under the guidance of a physiotherapist.[12]
Resources[edit | edit source]
References[edit | edit source]
- ↑ Schenkman M, Morey M, Kuchibhatla M. Spinal flexibility and balance control among community-dwelling adults with and without Parkinson's. J Gerontol A Biol Sci Med Sci. 2000;55(8):M441-445.
- ↑ 2.0 2.1 2.2 Duncan PW, Weiner DK, Chandler J, Studenski S. Functional reach: a new clinical measure of balance.J Gerontol. 1990;45(6):M192-197.
- ↑ Weiner DK, Duncan PW, Chandler J, Studenski SA. Functional reach: a marker of physical frailty. J Am Geriatr Soc. 1992;40(3):203-207.
- ↑ FRT Available from:https://www.sralab.org/sites/default/files/2017-06/5Hgjkv-Functional%20Reach%20Test.pdf (last accessed 16.10.2020)
- ↑ Ivan Miguel Pires, Garcia NM, Eftim Zdravevski. Measurement of Results of Functional Reach Test with Sensors: A Systematic Review. Electronics [Internet]. 2020 Jun 30 [cited 2024 Feb 6];9(7):1078–8. Available from: https://www.mdpi.com/2079-9292/9/7/1078
- ↑ 6.0 6.1 Duncan PW, Studenski S, Chandler J, Prescott B. Functional reach: predictive validity in a sample of elderly male veterans. Gerontol. 1992;47(3):M93-98.
- ↑ Standardized_Test_Reference_Card_Template Available from:http://functionalpathways.com/intranet-files/Standardized_Test_Reference_Card_Template.pdf (last accessed 16.10.2020)
- ↑ Eagle JD, Salama S, Whitman D, Evans LA, Ho E, Olde J. Comparison of three instruments in predicting accidental falls in selected inpatients in a general teaching hospital. Journal of Gerontology Nursing. 1999; 25(7): 40-45.
- ↑ Wernick-Robinson M, Krebs DE, Giorgetti MM. Functional reach: Does it really measure dynamic balance? Archives of Physical Medicine and Rehabilitation. 1999; 80(3): 262 - 269
- ↑ Wallmann HW. Comparison of elderly nonfallers and fallers on performance measures of functional reach, sensory organization, and limits of stability.J Gerontol A Biol Sci Med Sci. 2001;56(9):M580-583.
- ↑ Jonsson E, Henriksson M, Hirschfeld H. Does the functional reach test reflect stability limits in elderly people? J Rehabil Med. 2003;35(1):26-30.
- ↑ Lau MC, Lam JK, Siu E, Fung CS, Li KT, Lam MW. Physiotherapist-designed aquatic exercise programme for community-dwelling elders with osteoarthritis of the knee: a Hong Kong pilot study. Hong Kong Med J. 2014;20(1):16-23.






