Foot Orthotics Assessment: Difference between revisions
Carin Hunter (talk | contribs) No edit summary |
Carin Hunter (talk | contribs) No edit summary |
||
| Line 221: | Line 221: | ||
Watch this video if you want to learn more:{{#ev:youtube|rDcG224Zqi4}}<ref>Many Inaccuracies in Root Biomechanics Theory. Available from: https://www.youtube.com/watch?v=rDcG224Zqi4</ref> | Watch this video if you want to learn more:{{#ev:youtube|rDcG224Zqi4}}<ref>Many Inaccuracies in Root Biomechanics Theory. Available from: https://www.youtube.com/watch?v=rDcG224Zqi4</ref> | ||
What is Root Theory? There has been much discussion recently on the biomechanics theories and measurements proposed by Dr. Merton Root due to a recent paper by Jarvis et al. | |||
<nowiki>https://jfootankleres.biomedcentral.com/.../s13047-017</nowiki>... | |||
Dr. Kirby knew Dr. Root and personally attended many of his lectures, in addition to working closely with his colleague, Dr. John Weed during his podiatry student years and during his year as a Biomechanics Fellow at the California College of Podiatric Medicine (CCPM). Here is a sampling of the ideas taught at CCPM during the years from 1979-1985 while Dr. Kirby was a student and teaching biomechanics at CCPM and some commentary regarding the ideas proposed by Root et al. | |||
# The foot orthosis should be balanced with the heel vertical at all times unless the patient has a peroneal spastic flatfoot, a partially compensated rearfoot varus deformity where the maximally pronated position of the subtalar joint (STJ) has the calcaneus inverted or has a rearfoot valgus deformity. | |||
## Dr. Kirby was taught that to balance the heel of the orthosis even 2-3 degrees inverted would cause the patient to have adverse affects from the foot orthosis, which seems odd since the range of error of calcaneal bisections among CCPM Biomechanics Professors during the mid-1980s was about +/- 3 degrees. | |||
# The foot orthosis should be made of a rigid thermoplastic material but not be made of a shank-dependent material such as cork and leather or Plastazote since these shank dependent materials are not "rigid" enough to control abnormal "compensations" in foot. | |||
## Cork and leather orthoses and other shank dependent orthoses were not favored by the Root Theory advocates since they were thought to be only "acccommodative" orthoses and, since they were not made of "rigid plastic", couldn't possibly cause improved gait function. There was never any discussion by Dr. Root or his followers at CCPM that possibly these shank dependent devices could just as well improve gait function and reduce pathology for patients as well, if not better, than a vertically balanced Rohadur orthosis with a dental acrylic 4/4 degree rearfoot post that ended at the metatarsal necks. | |||
# The foot orthosis should end at the metatarsal necks and doesn't need forefoot extensions added to it. | |||
## In fact, addition of forefoot extensions to accommodate painful metatarsals was thought to be "chiropody", according to Dr. John Weed at one of the Root Lab Seminars, when Dr. Kirby asked Dr. Weed why a plantarflexed 3rd metatarsal head couldn't just be simply accommodated with 1/8" Korex to the sulcus to relieve the plantar 3rd metatarsal head pain. Dr. Weed had replied that a plantarflexed 3rd metatarsal "couldn't be treated" with a "functional foot orthosis" and would require surgery for treatment. Dr. Kirby disagreed with them at this seminar soon after his CCPM Biomechanics Fellowship in 1985 since he had been already successfully treating these conditions with forefoot accommodations to the sulcus during his Biomechanics Fellowship at CCPM. | |||
# The calcaneus must be in the vertical position while in relaxed calcaneal stance position (RCSP) in order for the foot to function normally during gait. | |||
## Root Theory, time and again, taught that the vertical heel position was "normal" and somehow functionally more "stable". Dr. Kirby asked John Weed in about 1983 why a maximally pronated STJ foot that had the heel vertical in relaxed bipedal stance, or what Drs. Root and Weed called a "fully compensated rearfoot varus", should be treated at their maximally pronated position with a vertically balanced orthosis. Dr. Weed didn't have a good explanation for this aspect of Root Theory. | |||
# Each foot has only one correct heel bisection. | |||
## Dr. Kirby suggested to an audience, in front of about 30 other podiatrists at one of the Root seminars in about 1985, that the calcaneal bisection line was highly variable depending on the clinician drawing the calcaneal bisection line and, as such, created a problem with the whole Root measurement system. Dr. Root said that "Even a monkey can be taught to draw an accurate calcaneal bisection line! I don't understand why the podiatrists teaching biomechanics at CCPM can't teach such a simple concept to their students!" | |||
# If a calcaneus is everted by more than two degrees then it will continue pronating until the maximally pronated position of the STJ is reached. | |||
## This odd idea was actually formulated into a list of incontrovertible "laws" of foot function by Dr. Bill Orien, one of the coauthors of the books by Root and Weed.. | |||
# A functional foot orthosis made from a cast of the foot held in the STJ neutral position will position the STJ in its neutral position while in stance and/or in gait. | |||
## This concept was taught at CCPM but when Dr. Kirby questioned John Weed on how this didn't make any sense he couldn't really explain how this concept could work. The students at CCPM called it "Biomagic". There was never given a good mechanical explanation by any professors of biomechanics at CCPM, including Drs. Root and Weed, as to how a foot orthosis that was taken in the STJ neutral position could somehow make a foot function in the STJ neutral position even though the foot orthosis was being balanced where the STJ was maximally pronated or very close to maximally pronated. The only explanation Dr. Kirby and his classmates got when they asked how orthoses actually worked was that "they locked the midtarsal joint" and "prevented compensations for forefoot and rearfoot deformities".. | |||
# The standard biomechanical examination (Root examination techniques) yields sufficient information to predict how that particular individual's lower extremity will function during gait. | |||
## That was something that Dr. Kirby saw as being erroneous during his CCPM Biomechanics Fellowship from 1984-1985. However, after speaking to John Weed one day in 1984 during my Biomechanics Fellowship about his "pushing on calcaneus technique" to determine how much "pronation control" features he needed to put into his patients' orthoses, Dr. Kirby eventually developed Dr. Weed's technique further to discover the significance of STJ axis location and how this one measurement parameter was probably as important, if not more important, at predicting gait function and pathology than any of the other Root measurements combined (Kirby KA: Methods for determination of positional variations in the subtalar joint axis. JAPMA, 77: 228-234, 1987). | |||
# Frontal plane forefoot deformities are congenital disorders, except "forefoot supinatus" deformities or traumatic deformities of the forefoot. | |||
## It is rather more likely that the frontal plane forefoot to rearfoot relationship is an indicator of the differential loading of the medial and lateral columns during weightbearing activities rather than an inherited, unchanging structural deformity which in itself determines the function of the foot. | |||
# If a patient stands in relaxed calcaneal stance position (RCSP) with their calcaneus inverted then there must be some abnormality causing the calcaneus to not be vertical (i.e. an inverted calcaneus is always abnormal). | |||
## Of course, if one clinician drew an inverted heel bisection relative to another clinician who drew a more everted heel bisection, depending on the clinician, the patient could go from having an abnormal inverted heel foot to a normal vertical heel foot, all by simply having another clinician draw on what they felt was the "correct" heel bisection. This common reality is one of the biggest "daggers in the heart" of Root biomechanics. Without a standardized, reproducible calcaneal bisection that examiners can agree upon, the whole Root measurement system falls apart since accurate determination of "rearfoot varus", "rearfoot valgus", "forefoot varus", "forefoot valgus", "neutral calcaneal stance position", "relaxed calcaneal stance position" and orthosis balancing position all are based on an this idea that there is only true calcaneal bisection. LaPointe et al showed the calcaneal bisection to have a range of error of 3-6 degrees (LaPointe SJ, Peebles C, Nakra A, Hillstrom H. The reliability of clinical and caliper-based calcaneal bisection measurements. J Am Podiatr Med Assoc. 2001; 91(3):121-126). | |||
# A foot with an everted forefoot to rearfoot relationship should be treated with an orthosis which is balanced with the heel vertical. | |||
## We again get back to the erroneous assumption proclaimed by the Root theory advocates that the heel vertical position is the most desirable position for the foot to function in and the orthosis to control the foot in. To place all patients which have a plantarflexed first ray deformity or forefoot valgus deformity in foot orthoses which have been balanced with the heel vertical is much too simplistic of an approach to guarantee optimum orthosis results for all patients. | |||
All this being said, Dr. Kirby fully acknowledges the wonderful contributions that Dr. Root and his colleagues did make to our progression of knowledge in developing better techniques for treating our patients with foot and lower extremity mechanically-based pathologies. It is time now to move forward, and not stagnate by glorifying the memories of those who have come before us. Thank you, Dr. Root, Dr. Weed and colleagues, for your contributions to our knowledge of foot and lower extremity biomechanics and the treatment of mechanically-based pathologies with foot orthoses | |||
For more information, you can follow Dr Kirby on his [https://www.facebook.com/kevinakirbydpm/ Facebook] page or his [http://www.kirbypodiatry.com/?fbclid=IwAR0piOHJZlrXkZVHvbLu94nw8XnguPgqtNClbZ1FxMsrM45bIxUF7_qbI1g website]. | |||
Deviated M, Axis ST, Positioned N, Deviated L. The Evolution of Foot Orthoses in Sports Part 2. | |||
Kirby KA, Spooner SK, Scherer PR, Schuberth JM. Foot orthoses. Foot & Ankle Specialist. 2012 Oct;5(5):334-43. | |||
==== 7. [[Leg Length Discrepancy]] (LLD) ==== | ==== 7. [[Leg Length Discrepancy]] (LLD) ==== | ||
Revision as of 20:30, 26 February 2022
Top Contributors - Carin Hunter, Jess Bell, Kim Jackson, Lucinda hampton, Ewa Jaraczewska and Tarina van der Stockt
Introduction[edit | edit source]
Orthotics is a branch of medicine that deals with the making and fitting of orthotic devices. There are many interchangeable terms for this, a few being foot orthotic/orthosis/insole/shoe insert. Before an orthosis can be prescribed, a comprehensive assessment needs to be conducted to correctly select a device that will meet all the requirements. Selecting an orthotic device can be complicated as there are many aspects that need to be considered aside from biomechanical factors, including comfort and aesthetics to enhance patient compliance.
Three Main Types of Foot Orthoses[edit | edit source]
- Off the shelf (OTS) insoles
- Functional foot orthoses (FFO)
- Custom moulded total contact insoles (TCI)
Purpose of Foot Orthoses[edit | edit source]
A foot orthosis is generally referred to as an "externally applied apparatus that can be inserted in a shoe to help support or improve the function of the foot and/or ankle."[1] The two main goals of an orthotic device are to reduce pressure across an area or to accommodate congenital or acquired deformities. The ultimate aim is to achieve / maintain near-neutral subtalar joint alignment during the gait cycle or the individual's highest functional level.[1]
- Support
- Correct, if mobile
- Accommodate if not
- Shock absorption
- Re-distribute pressure
Basic Foot Anatomy[edit | edit source]
For a detailed discussion of foot and ankle anatomy, please click the links.
- 28 bones
- 33 joints
- Ligaments
- Tendons
- Muscles
- Plantar fascia
Plantar Fascia[edit | edit source]
- The plantar fascia is a strong, fibrous tissue. Because it is stiff and largely impermeable, it is able to help protect the muscles of the sole of the foot.[2][3]
- Its origins are deep within the plantar surface of the calcaneus and it fans out across the metatarsal heads. It divides and attaches to the base of the phalanges of each toe.[3]
- During walking, as the toes dorsiflex at push off, the plantar fascia wraps around the metatarsal heads and tightens.[3] This pulls the calcaneus towards the metatarsal heads and in turn maintains the shape of the longitudinal arch and supports the foot to enable propulsion. This is a phenomenon known as the windlass mechanism.[4]
Windlass Mechanism[edit | edit source]
The windlass mechanism was first described by JH Hicks in 1954. Essentially it is: "a one-to-one coupling between metatarsal joint dorsiflexion and medial longitudinal arch rise."[5] Based on an engineering concept of lifting weights via a pulley system, Hicks noted that during dorsiflexion of the toes, the plantar aponeurosis tightens. This draws the metatarsal heads towards the calcaneus, which increases the height of the longitudinal arch.[5] This action occurs naturally at push off in gait cycle as toes dorsiflex and the foot becomes stiffer to aid propulsion. During loading and mid stance, the arch will stretch. The human foot is flexible due to its many articulations. However, it needs to be both flexible and rigid to promote normal gait.[6] It is important to remember that the plantar fascia will stretch and recoil at different stages of the gait cycle.[5]
Important Joints to Consider for Foot Orthosis[edit | edit source]
- Hindfoot
- Talocrural joint
- Sub talar joint
- Mid Foot
- Tarsometatarsal joint
- Calcaneocuboid joint
- Talonavicular joint
- Fore Foot
- 1st metatarsal phalangeal joint
More information on foot and ankle joints is available here.
Terminology used in Orthotics[edit | edit source]
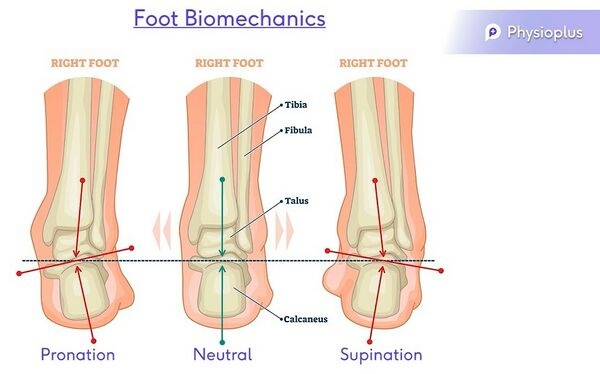
Neutral
Varus –inverted
Pronation – eversion, abduction, dorsiflexion and medially rotated subtalar joint
Supination – inversion, adduction, plantarflexion and laterally rotated subtalar joint
Purpose of the Human Foot[edit | edit source]
“[The human foot] enables propulsion through space, adaptation to uneven terrain, absorption of shock, and support of body weight.”[7] However, its structure, function and position leave it exposed to injury. To understand the foot, it is necessary to assess it in non-weight-bearing and weight-bearing positions, and during gait.[8]
Orthotic Foot Ankle Assessment[edit | edit source]
During a foot and ankle assessment for orthotics selection, you will need to look at:[8]
- Patient history
- Range of motion
- Muscle power
- Sensation / pain
- Proprioception
- Biomechanical analysis
- Leg length
1. Patient History[edit | edit source]
- Gait pattern and biomechanical analysis on entrance
- History of underlying conditions, foot problems and the primary problem affecting the individual on consultation.
2. Range of Motion[edit | edit source]
When considering foot orthosis design, the following range of motion tests should be carried out:
- Active
- Passive
- Weight-bearing
- Non-weight-bearing
Active and passive movements of the foot and ankle[10]
- Dorsiflexion/ plantarflexion = a quick test for the ankle joint
- Pronation/ supination = a quick test for the subtalar joint
- Eversion/ inversion
- Abduction / adduction
- Toe flexion/ extension = a quick test for the metatarsal phalangeal joints
Non-weight-bearing assessment[10]
- Windlass Test - can be effective for examining dysfunction of the plantar fascia although its specificity has not been proved.
- Passively extend hallux at the MTP joint
- The plantar aponeurosis should tighten and reduce the distance between the calcaneus and metatarsals
- Please note that the angle of extension to initiate the arch can vary
- Increases medial longitudinal arch
- Positive Test: a test is considered positive if passive extension continues to end range or until the patient's plantar fasciitis pain is reproduced
- Passively extend hallux at the MTP joint
- Pain in medial calcaneus and plantar fascia on palpation[8]
- Hallux limitus/rigidus[8]
- Both affect the windlass mechanism, gait pattern and normal functioning of the foot.[8]
- Hallux Rigidus[11]
- Very limited dorsiflexion mobility or no movement. There is crepitation with joint mobilisation and pain associated with any movement of the first MTP joint.
- Hallux Limitus[12] (FnHL)
- Reduced dorsiflexion movement, resulting in decreased range of dorsiflexion at the first MTP joint.
- In gait, there is a loss of MTP joint extension during the second half of the single-support phase, when the weightbearing foot is in maximal dorsiflexion.[8]
- Hallux Rigidus[11]
3. Muscles of the Foot and Ankle[edit | edit source]
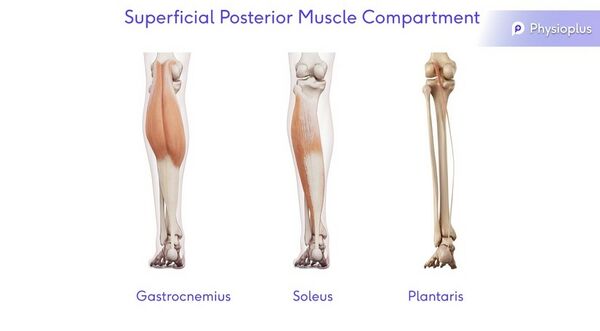
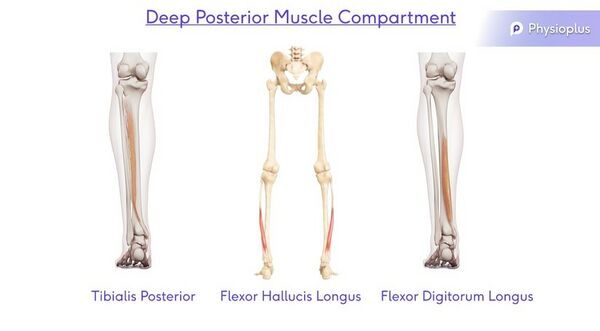
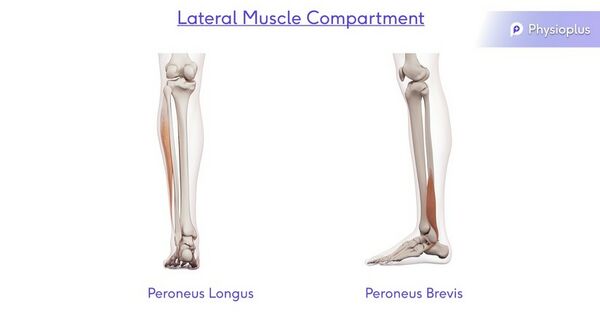
There are four muscle compartments in the lower leg. The gold standard test for assessing these muscles is the standardised Oxford Scale.
Superficial Posterior Muscle Compartment
Action: Plantarflexion
Muscles: Gastrocnemius, Soleus and Plantaris
Deep Posterior Muscle Compartment
Action: Plantarflexion, Adduction and Inversion
Muscles: Tibialis Posterior, Flexor Hallicus Longus and Flexor Digitorum Longus
Lateral Muscle Compartment
Action: Dorsiflexion, Abduction and Eversion
Muscles: Peroneus Longus and Peroneus Brevis
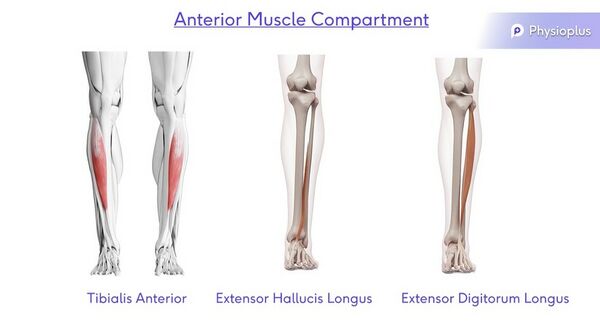
Anterior Muscle Compartment
Action: Dorsiflexion, Abduction and Inversion
Muscles: Tibialis Anterior, Extensor Hallicus Longus and Extensor Digitorum Longus
See the following pages for more information on the muscle testing of:
4. Sensation/Pain[edit | edit source]
Please see page on Sensation, Sensory Examination
5. Proprioception[edit | edit source]
Please see page on Proprioception, Assessing Proprioception
6. Biomechanical Analysis[edit | edit source]
It is important to assess the foot both statically and dynamically. This is because the foot is not static during the gait cycle, and most foot problems occur during the gait cycle.[8] It is important to consider the whole kinetic chain, including knee and hip/pelvis position, as well as subtalar alignment.
Static
- Too many toes/ too few toes - useful for distinguishing between a pronated and supinated foot
- Jack's Test
- Windlass test
- Rear foot and forefoot alignment
- Normal/ideal foot alignment occurs when:[8]
- Distal 1/3 of leg is vertical
- Calcaneus is vertical to the supporting surface
- Plantar forefoot is parallel to the plantar rearfoot
- Variations from this “normal’ foot alignment (‘intrinsic foot deformities’) lead to abnormal foot function
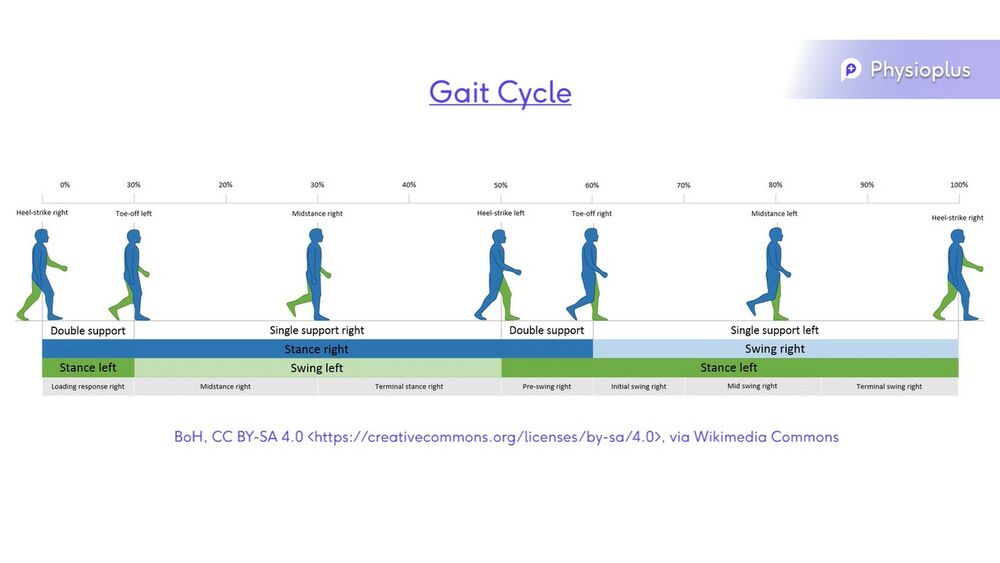
Dynamic Normal Walking[10]
- Phases of Normal Walking
- Heel strike
- Mid stance
- Terminal stance
- Pre swing
- Swing phase
- Ground clearance is important in swing phase
- Proprioception and balance are important for approximately 40% of the gait pattern where an individual is standing on one leg.[8]
The Supination Resistance Test[edit | edit source]
The supination resistance test [13]may be clinically useful in the prescription of foot orthoses, but more work is needed to determine its validity and its relationship to clinical outcomes.[14]
A high supination resistance score indicates the use of a HIGH arch orthotic.
A moderate supination resistance score indicates the use of a MODERATE arch orthotic.
A low supination resistance score indicates the use of a LOW arch orthotic.
Root Theory[edit | edit source]
The root theory was originally developed by Dr.Merton L. Root during the late 1950s through early 1960s. It is also known as “the foot morphology theory,” “the subtalar joint neutral theory,” or simply “Rootian theory”[15]. Simply the root theory is based on a series of static measurements that is believed by the author to predict kinematic function. In order for the foot to be normal, the subtalar joint (STJ) should be in neutral position with the midtarsal joint fully locked[16], this occurs between mid-stance and heel-off during walking[17]. Any deviations from the stated STJ alignment is considered to be abnormal and should, therefore, exhibit mechanical dysfunction.
Despite receiving clinical popularity and being utilized in most podiatry and orthopedic literature, the root theory is questioned with regards to its reliability, validity and practicality.[17][15] In the 1950s and 60s advanced measuring equipment wasn't available. In addition, most of the research done using this method has been conducted with techniques different from those proposed by Dr. Root. It is also worth to note that Dr. Root has prescribed orthotics in his practice, but the exact methods weren't published or documented, therefore, interpretations of such methods cannot be reliable.[15]
A 2017 study by Jarvis et al [18]was conducted to investigate foot kinematics between normal and abnormal feet classified according to Root et al, determine if the degree of structural deformity is associated with the degree of compensations and finally to measure subtalar joint position during gait in pain free feet. The results of the kinematic analysis of this study reported no association between the deformities proposed by Root et al. and the differences in foot kinematics during gait. STJ inversion in neutral calcaneal standing position (NCSP ) has no relation to rearfoot kinematics, this means that the clinical use of “subtalar joint neutral” might not provide clinicians with realistic information. Jarvis et al also found the first MPJ dorsiflexion during gait propulsion much less than 65°as proposed by Root. It is evident that not all feet with structural deformities should exhibit symptoms and their function will be affected, therefore the root's classification seems to be invalid and believed to be no longer suitable for professional practice. A simple explanation of why static assessment doesn't necessary reflect kinematic characteristics is that it is taken in non-weight bearing position which may not mimic the applied external and muscular force in weight bearing.
Watch this video if you want to learn more:
What is Root Theory? There has been much discussion recently on the biomechanics theories and measurements proposed by Dr. Merton Root due to a recent paper by Jarvis et al.
https://jfootankleres.biomedcentral.com/.../s13047-017...
Dr. Kirby knew Dr. Root and personally attended many of his lectures, in addition to working closely with his colleague, Dr. John Weed during his podiatry student years and during his year as a Biomechanics Fellow at the California College of Podiatric Medicine (CCPM). Here is a sampling of the ideas taught at CCPM during the years from 1979-1985 while Dr. Kirby was a student and teaching biomechanics at CCPM and some commentary regarding the ideas proposed by Root et al.
- The foot orthosis should be balanced with the heel vertical at all times unless the patient has a peroneal spastic flatfoot, a partially compensated rearfoot varus deformity where the maximally pronated position of the subtalar joint (STJ) has the calcaneus inverted or has a rearfoot valgus deformity.
- Dr. Kirby was taught that to balance the heel of the orthosis even 2-3 degrees inverted would cause the patient to have adverse affects from the foot orthosis, which seems odd since the range of error of calcaneal bisections among CCPM Biomechanics Professors during the mid-1980s was about +/- 3 degrees.
- The foot orthosis should be made of a rigid thermoplastic material but not be made of a shank-dependent material such as cork and leather or Plastazote since these shank dependent materials are not "rigid" enough to control abnormal "compensations" in foot.
- Cork and leather orthoses and other shank dependent orthoses were not favored by the Root Theory advocates since they were thought to be only "acccommodative" orthoses and, since they were not made of "rigid plastic", couldn't possibly cause improved gait function. There was never any discussion by Dr. Root or his followers at CCPM that possibly these shank dependent devices could just as well improve gait function and reduce pathology for patients as well, if not better, than a vertically balanced Rohadur orthosis with a dental acrylic 4/4 degree rearfoot post that ended at the metatarsal necks.
- The foot orthosis should end at the metatarsal necks and doesn't need forefoot extensions added to it.
- In fact, addition of forefoot extensions to accommodate painful metatarsals was thought to be "chiropody", according to Dr. John Weed at one of the Root Lab Seminars, when Dr. Kirby asked Dr. Weed why a plantarflexed 3rd metatarsal head couldn't just be simply accommodated with 1/8" Korex to the sulcus to relieve the plantar 3rd metatarsal head pain. Dr. Weed had replied that a plantarflexed 3rd metatarsal "couldn't be treated" with a "functional foot orthosis" and would require surgery for treatment. Dr. Kirby disagreed with them at this seminar soon after his CCPM Biomechanics Fellowship in 1985 since he had been already successfully treating these conditions with forefoot accommodations to the sulcus during his Biomechanics Fellowship at CCPM.
- The calcaneus must be in the vertical position while in relaxed calcaneal stance position (RCSP) in order for the foot to function normally during gait.
- Root Theory, time and again, taught that the vertical heel position was "normal" and somehow functionally more "stable". Dr. Kirby asked John Weed in about 1983 why a maximally pronated STJ foot that had the heel vertical in relaxed bipedal stance, or what Drs. Root and Weed called a "fully compensated rearfoot varus", should be treated at their maximally pronated position with a vertically balanced orthosis. Dr. Weed didn't have a good explanation for this aspect of Root Theory.
- Each foot has only one correct heel bisection.
- Dr. Kirby suggested to an audience, in front of about 30 other podiatrists at one of the Root seminars in about 1985, that the calcaneal bisection line was highly variable depending on the clinician drawing the calcaneal bisection line and, as such, created a problem with the whole Root measurement system. Dr. Root said that "Even a monkey can be taught to draw an accurate calcaneal bisection line! I don't understand why the podiatrists teaching biomechanics at CCPM can't teach such a simple concept to their students!"
- If a calcaneus is everted by more than two degrees then it will continue pronating until the maximally pronated position of the STJ is reached.
- This odd idea was actually formulated into a list of incontrovertible "laws" of foot function by Dr. Bill Orien, one of the coauthors of the books by Root and Weed..
- A functional foot orthosis made from a cast of the foot held in the STJ neutral position will position the STJ in its neutral position while in stance and/or in gait.
- This concept was taught at CCPM but when Dr. Kirby questioned John Weed on how this didn't make any sense he couldn't really explain how this concept could work. The students at CCPM called it "Biomagic". There was never given a good mechanical explanation by any professors of biomechanics at CCPM, including Drs. Root and Weed, as to how a foot orthosis that was taken in the STJ neutral position could somehow make a foot function in the STJ neutral position even though the foot orthosis was being balanced where the STJ was maximally pronated or very close to maximally pronated. The only explanation Dr. Kirby and his classmates got when they asked how orthoses actually worked was that "they locked the midtarsal joint" and "prevented compensations for forefoot and rearfoot deformities"..
- The standard biomechanical examination (Root examination techniques) yields sufficient information to predict how that particular individual's lower extremity will function during gait.
- That was something that Dr. Kirby saw as being erroneous during his CCPM Biomechanics Fellowship from 1984-1985. However, after speaking to John Weed one day in 1984 during my Biomechanics Fellowship about his "pushing on calcaneus technique" to determine how much "pronation control" features he needed to put into his patients' orthoses, Dr. Kirby eventually developed Dr. Weed's technique further to discover the significance of STJ axis location and how this one measurement parameter was probably as important, if not more important, at predicting gait function and pathology than any of the other Root measurements combined (Kirby KA: Methods for determination of positional variations in the subtalar joint axis. JAPMA, 77: 228-234, 1987).
- Frontal plane forefoot deformities are congenital disorders, except "forefoot supinatus" deformities or traumatic deformities of the forefoot.
- It is rather more likely that the frontal plane forefoot to rearfoot relationship is an indicator of the differential loading of the medial and lateral columns during weightbearing activities rather than an inherited, unchanging structural deformity which in itself determines the function of the foot.
- If a patient stands in relaxed calcaneal stance position (RCSP) with their calcaneus inverted then there must be some abnormality causing the calcaneus to not be vertical (i.e. an inverted calcaneus is always abnormal).
- Of course, if one clinician drew an inverted heel bisection relative to another clinician who drew a more everted heel bisection, depending on the clinician, the patient could go from having an abnormal inverted heel foot to a normal vertical heel foot, all by simply having another clinician draw on what they felt was the "correct" heel bisection. This common reality is one of the biggest "daggers in the heart" of Root biomechanics. Without a standardized, reproducible calcaneal bisection that examiners can agree upon, the whole Root measurement system falls apart since accurate determination of "rearfoot varus", "rearfoot valgus", "forefoot varus", "forefoot valgus", "neutral calcaneal stance position", "relaxed calcaneal stance position" and orthosis balancing position all are based on an this idea that there is only true calcaneal bisection. LaPointe et al showed the calcaneal bisection to have a range of error of 3-6 degrees (LaPointe SJ, Peebles C, Nakra A, Hillstrom H. The reliability of clinical and caliper-based calcaneal bisection measurements. J Am Podiatr Med Assoc. 2001; 91(3):121-126).
- A foot with an everted forefoot to rearfoot relationship should be treated with an orthosis which is balanced with the heel vertical.
- We again get back to the erroneous assumption proclaimed by the Root theory advocates that the heel vertical position is the most desirable position for the foot to function in and the orthosis to control the foot in. To place all patients which have a plantarflexed first ray deformity or forefoot valgus deformity in foot orthoses which have been balanced with the heel vertical is much too simplistic of an approach to guarantee optimum orthosis results for all patients.
All this being said, Dr. Kirby fully acknowledges the wonderful contributions that Dr. Root and his colleagues did make to our progression of knowledge in developing better techniques for treating our patients with foot and lower extremity mechanically-based pathologies. It is time now to move forward, and not stagnate by glorifying the memories of those who have come before us. Thank you, Dr. Root, Dr. Weed and colleagues, for your contributions to our knowledge of foot and lower extremity biomechanics and the treatment of mechanically-based pathologies with foot orthoses
For more information, you can follow Dr Kirby on his Facebook page or his website.
Deviated M, Axis ST, Positioned N, Deviated L. The Evolution of Foot Orthoses in Sports Part 2.
Kirby KA, Spooner SK, Scherer PR, Schuberth JM. Foot orthoses. Foot & Ankle Specialist. 2012 Oct;5(5):334-43.
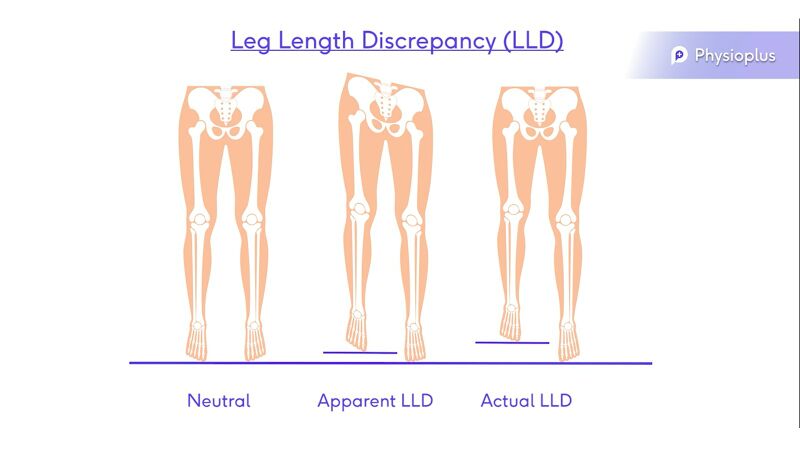
7. Leg Length Discrepancy (LLD)[edit | edit source]
- Dipping
- Pelvic obliquity
- Retraction
- Scoliosis
- Apparent leg length
- Actual leg length[20]
This video covers a biomechanical assessment
References[edit | edit source]
- ↑ 1.0 1.1 Elattar O, Smith T, Ferguson A, Farber D, Wapner K. Uses of braces and orthotics for conservative management of foot and ankle disorders. Foot & Ankle Orthopaedics. 2018 Aug 3;3(3):2473011418780700.
- ↑ Welte L, Kelly LA, Kessler SE, Lieberman DE, D'Andrea SE, Lichtwark GA, Rainbow MJ. The extensibility of the plantar fascia influences the windlass mechanism during human running. Proceedings of the Royal Society B. 2021 Jan 27;288(1943):20202095.
- ↑ 3.0 3.1 3.2 Orthopaedia.com. Anatomy of the foot and ankle. Available from: https://orthopaedia.com/page/Anatomy-of-the-Foot-Ankle (accessed 10/02/2022).
- ↑ Sichting F, Holowka NB, Ebrecht F, Lieberman DE. Evolutionary anatomy of the plantar aponeurosis in primates, including humans. Journal of anatomy. 2020 Jul;237(1):85-104.
- ↑ 5.0 5.1 5.2 Sichting F, Ebrecht F. The rise of the longitudinal arch when sitting, standing, and walking: Contributions of the windlass mechanism. PloS one. 2021 Apr 8;16(4):e0249965.
- ↑ Kelly LA, Lichtwark G, Cresswell AG. Active regulation of longitudinal arch compression and recoil during walking and running. J R Soc Interface. 2015;12(102):20141076.
- ↑ Bolgla LA, Malone TR. Plantar fasciitis and the windlass mechanism: a biomechanical link to clinical practice. Journal of athletic training. 2004 Jan;39(1):77.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 8.7 8.8 Fisher D. Introduction to Foot Orthotics Course. Physioplus, 2022.
- ↑ Gegen ME, Plummer T, Darr N. An Exploratory Study of The Perceptions of Footwear for Individuals who use Lower Limb Orthotics. Internet Journal of Allied Health Sciences and Practice. 2020;18(4):8.
- ↑ 10.0 10.1 10.2 Alazzawi S, Sukeik M, King D, Vemulapalli K. Foot and ankle history and clinical examination: A guide to everyday practice. World journal of orthopedics. 2017 Jan 18;8(1):21.
- ↑ Colò G, Fusini F, Samaila EM, Rava A, Felli L, Alessio-Mazzola M, Magnan B. The efficacy of shoe modifications and foot orthoses in treating patients with hallux rigidus: a comprehensive review of literature. Acta Bio Medica: Atenei Parmensis. 2020;91(Suppl 14).
- ↑ Graydon M. Hallux Limitus/Rigidus. Clinical Practice Guidelines. 2018:140.
- ↑ McBride S, Dixon P, Mokha M, Cheng MS. The relationship between supination resistance and the kinetics and kinematics of the foot and ankle during gait. Gait & Posture. 2019 Sep 1;73:239-45.
- ↑ Noakes H, Payne C. The reliability of the manual supination resistance test. Journal of the American Podiatric Medical Association. 2003 May;93(3):185-9.
- ↑ 15.0 15.1 15.2 Harradine P, Gates L, Bowen C. If it doesn't work, why do we still do it? The continuing use of subtalar joint neutral theory in the face of overpowering critical research. journal of orthopaedic & sports physical therapy. 2018 Mar;48(3):130-2.
- ↑ Root ML. Normal and abnormal function of the foot. Clinical biomechanics. 1977;2.
- ↑ 17.0 17.1 McPoil TG, Hunt GC. Evaluation and management of foot and ankle disorders: present problems and future directions. Journal of Orthopaedic & Sports Physical Therapy. 1995 Jun;21(6):381-8.
- ↑ Jarvis HL, Nester CJ, Bowden PD, Jones RK. Challenging the foundations of the clinical model of foot function: further evidence that the root model assessments fail to appropriately classify foot function. Journal of foot and ankle research. 2017 Dec;10(1):7.
- ↑ Many Inaccuracies in Root Biomechanics Theory. Available from: https://www.youtube.com/watch?v=rDcG224Zqi4
- ↑ Menez C, L'Hermette M, Coquart J. Orthotic insoles improve gait symmetry and reduce immediate pain in subjects with mild leg length discrepancy. Frontiers in sports and active living. 2020;2.