Exercise Induced Asthma: Difference between revisions
No edit summary |
No edit summary |
||
| Line 6: | Line 6: | ||
== Introduction == | == Introduction == | ||
[[File:Asthma inhaler use.png|right|frameless]] | |||
Exercise-induced bronchoconstriction (EIB) describes a transient and reversible contraction of bronchial smooth muscle after physical exertion that may or may not produce symptoms of [[Dyspnoea|dyspnea]], chest tightness, wheezing, and cough. (EIB, previously called Exercise-Induced Asthma)<ref name=":0">Gerow M, Bruner PJ. [https://www.ncbi.nlm.nih.gov/books/NBK557554/ Exercise Induced Asthma]. Treasure Island, FL: StatPearls. 2020.Available from: https://www.ncbi.nlm.nih.gov/books/NBK557554/ (accessed 6.4.2021)</ref>. | |||
* EIB occurs in 40% to 90% of people with [[asthma]] and up to 20% of those without asthma. | |||
* The benefits of regular [[Therapeutic Exercise|exercise]] for all people are well established, and activity is an integral part of a healthy lifestyle. People suffering from EIB may avoid exertion due to symptoms of breathlessness, cough, chest tightness, and wheezing. Exercise avoidance has been shown to increase social isolation in adolescents, and it can lead to obesity and poor health. | |||
* Exercise has paradoxically been shown to improve EIB severity, [[Pulmonary Function Test|pulmonary function]], and reduce airway [[Inflammation Acute and Chronic|inflammation]] in people with asthma and EIB. | |||
* Early detection, diagnosis confirmed by the change in lung function during exercise, and treatment can improve [[Quality of Life|quality of life]] and, when managed appropriately, allows patients to participate freely in exercise without limiting competition at the elite level.<ref name=":0" /> | |||
Exercise-induced bronchoconstriction | == Epidemiology == | ||
* Exercise-induced bronchoconstriction occurs in 40% to 90% of people with asthma and up to 20% of the general population without asthma. | |||
* Elite athletes have an increased prevalence of 30% to 70%. | |||
* Exercise-induced asthma is the most common medical problem among winter Olympic athletes, especially among cross-country skiers. Nearly 50% of these athletes suffer from the condition, closely followed by short-track speed skaters at 43%<ref>The Conversation Winter Olympics: why many athletes will be struggling with asthma Available from:https://theconversation.com/winter-olympics-why-many-athletes-will-be-struggling-with-asthma-90400 (accessed 6.4.2021)</ref>. | |||
* Approximately 400 million people are projected to have asthma in 2024, with a large percentage expected to have EIB. | |||
* Annually, 250,000 people die from asthma complications<ref name=":0" />. | |||
== | == Cause == | ||
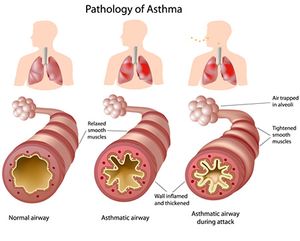
[[File:Pathology.jpg|right|frameless]] | |||
EIB is caused by an acute large increase in the amount of air entering the airways that require heating and humidifying. In susceptible individuals, this results in inflammatory, neuronal, and vascular changes ultimately resulting in contraction of the bronchial smooth muscle and symptoms of dyspnea, cough, chest tightness, mucus production, and wheezing.<ref name=":0" />.<ref>Asthma org. EIB Available from:https://asthma.org.au/about-asthma/triggers/exercise-induced-bronchoconstriction/ (accessed 6.4.2021)</ref> | |||
Asthma is the result of complex interactions between genetic predisposition and multiple environmental influences. The marked increase in asthma prevalence in the last 3 decades suggests environmental factors as a key contributor in the process of allergic sensitization. <ref name="Goodman">Goodman CC, Snyder TE. Differential Diagnosis for Physical Therapists, Screening for Referral. W B Saunders Company; 2012. 298</ref><br>Factors that can trigger or worsen exercise-induced asthma include: | |||
* Cold air | |||
* Dry air | |||
* Air pollution such as smoke or smog | |||
* High pollen counts | |||
* Having a respiratory infection such as a cold | |||
* Chemicals, such as chlorine in swimming pools | |||
No exercise in particular must be avoided if a patient has exercise induced asthma. It is important to note, however, activities that cause the patient to breathe harder are more likely to trigger symptoms.<ref name="Mayo">"Exercise-induced asthma." Mayo Clinic. N.p., n.d. Web. 25 Mar. 2014. &lt;http://www.mayoclinic.org/diseases-conditions/exercise-induced-asthma/basics/definition/con-20033156&gt;.</ref> | |||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
Symptoms of exercise-induced bronchoconstriction can include mild to moderate symptoms of chest tightness, wheezing, coughing, and dyspnea that occurs within 15 minutes after 5 to 8 minutes of high-intensity aerobic training. Reports of severe symptoms with respiratory failure and death occur rarely. | |||
Symptoms: | |||
* occur more often in specific environments with cold, dry air or high concentration of respiratory irritants. | |||
* usually resolve spontaneously within 30 to 90 minutes and induce a refractory period of 1 to 3 hours, where continued exercise does not produce bronchoconstriction. Patients may also be asymptomatic, and therefore EIB may be underdiagnosed. | |||
Risk factors include: | |||
* personal or family history of asthma | |||
* personal history of atopy or allergic rhinitis | |||
* exposure to cigarette smoke, | |||
* participating in high-risk sports. High-risk sports include episodes of exercise greater than 5 to 8 minutes in certain environments (eg cold, dry air or chlorinated pools) such as long-distance running, cycling, cross country or downhill skiing, ice hockey, ice skating, high altitude sports, swimming, water polo, and triathlons. | |||
* living and practicing in areas with high levels of pollution | |||
* female gender. <ref name=":0" /> | |||
== Associated Co-morbidities == | == Associated Co-morbidities == | ||
| Line 30: | Line 52: | ||
Adults with asthma are found to have significantly more comorbidities than the general population. These include respiratory infections and allergic rhinitis. High impact/high prevalence chronic conditions such as depression have also been found in one out of four adults with asthma. Children suffering from asthma were found to have fewer comorbidities than adults, but 12.6% had an associated chronic medical condition. The most prevalent co-morbidities found in adults with asthma are time-limited minor infections, while others with a high impact and/or high prevalence are depression, hypertension, diabetes, ischemic heart disease, degenerative joint disease, cardiac arrhythmia, cancer, congestive heart failure, cerebrovascular disease and COPD.<ref name="Boulay">Boulay, Marie-Ève, and Louis-Philippe Boulet. "Asthma-related Comorbidities." Informahealthcare.com. Centre De Recherche De L’Institut Universitaire De Cardiologie Et De Pneumologie De Québec, 2001. Web. 23 Mar. 2014. &lt;http%3A%2F%2Finformahealthcare.com%2Fdoi%2Fpdf%2F10.1586%2Fers.11.34%3FnoFrame%3Dtrue&gt;.</ref> | Adults with asthma are found to have significantly more comorbidities than the general population. These include respiratory infections and allergic rhinitis. High impact/high prevalence chronic conditions such as depression have also been found in one out of four adults with asthma. Children suffering from asthma were found to have fewer comorbidities than adults, but 12.6% had an associated chronic medical condition. The most prevalent co-morbidities found in adults with asthma are time-limited minor infections, while others with a high impact and/or high prevalence are depression, hypertension, diabetes, ischemic heart disease, degenerative joint disease, cardiac arrhythmia, cancer, congestive heart failure, cerebrovascular disease and COPD.<ref name="Boulay">Boulay, Marie-Ève, and Louis-Philippe Boulet. "Asthma-related Comorbidities." Informahealthcare.com. Centre De Recherche De L’Institut Universitaire De Cardiologie Et De Pneumologie De Québec, 2001. Web. 23 Mar. 2014. &lt;http%3A%2F%2Finformahealthcare.com%2Fdoi%2Fpdf%2F10.1586%2Fers.11.34%3FnoFrame%3Dtrue&gt;.</ref> | ||
== Systemic Involvement == | == Systemic Involvement == | ||
| Line 65: | Line 57: | ||
Asthma can affect the entire pulmonary system. Often times the lungs become hyperreactive resulting in an exaggerated response to allergens and other irritants. In response, the muscles of the airway constrict, making the ability to breathe more challenging. As this hyperactive response occurs, so also does the process of inflammation. This causes the air passages to become swollen and the cells lining the passages to produce excess mucus, further impairing breathing.<ref name="Goodman" /> | Asthma can affect the entire pulmonary system. Often times the lungs become hyperreactive resulting in an exaggerated response to allergens and other irritants. In response, the muscles of the airway constrict, making the ability to breathe more challenging. As this hyperactive response occurs, so also does the process of inflammation. This causes the air passages to become swollen and the cells lining the passages to produce excess mucus, further impairing breathing.<ref name="Goodman" /> | ||
== Medical Management | == Medical Management == | ||
<div> | <div> | ||
'''Prevention''':<br>American Academy of Allergy, Asthma, and Immunology (AAAAI) promotes utilization of self-management and prevention strategies for patients with asthma. A daily asthma management plan, as well as other information and resources, can be found on the AAAAI website.<ref name="Goodman" /> <ref name="AAAI">The American Academy of Allergy, Asthma and Immunology. Accessed March 25, 2014 at http://www.aaaai.org/home.aspx</ref>'''<br>'''<br> | '''Prevention''':<br>American Academy of Allergy, Asthma, and Immunology (AAAAI) promotes utilization of self-management and prevention strategies for patients with asthma. A daily asthma management plan, as well as other information and resources, can be found on the AAAAI website.<ref name="Goodman" /> <ref name="AAAI">The American Academy of Allergy, Asthma and Immunology. Accessed March 25, 2014 at http://www.aaaai.org/home.aspx</ref>'''<br>'''<br> | ||
| Line 92: | Line 84: | ||
'''4. Protection Against Cold''': Wearing a scarf over the mouth prior to/during activity may help to decrease cold-induced EIB <br><br> | '''4. Protection Against Cold''': Wearing a scarf over the mouth prior to/during activity may help to decrease cold-induced EIB <br><br> | ||
</div> | </div> | ||
== Physical Therapy Management | == Physical Therapy Management == | ||
'''Acute Management:'''<br>Because EIB is triggered by exercise, physical therapists may be the first to identify asthma symptoms in a patient with undiagnosed EIB. For this reason, physical therapists must be aware of the associated signs and symptoms of EIB, as well as any red flags that may indicate a need for medical referral and treatment. If a patient has an acute asthma attack during therapy, the physical therapist should assess the severity of the attack, then position the patient in high Fowler’s position for diaphragmatic and pursed-lip breathing, if appropriate. If the patient has an inhaler available, the physical therapist should provide assistance to allow the patient to self-administer the medication, while helping the patient to relax<ref name="Goodman 2">Goodman CC, Snyder TE. Differential Diagnosis for Physical Therapists, Screening for Referral. W B Saunders Company; 2012.772-774</ref>. | '''Acute Management:'''<br>Because EIB is triggered by exercise, physical therapists may be the first to identify asthma symptoms in a patient with undiagnosed EIB. For this reason, physical therapists must be aware of the associated signs and symptoms of EIB, as well as any red flags that may indicate a need for medical referral and treatment. If a patient has an acute asthma attack during therapy, the physical therapist should assess the severity of the attack, then position the patient in high Fowler’s position for diaphragmatic and pursed-lip breathing, if appropriate. If the patient has an inhaler available, the physical therapist should provide assistance to allow the patient to self-administer the medication, while helping the patient to relax<ref name="Goodman 2">Goodman CC, Snyder TE. Differential Diagnosis for Physical Therapists, Screening for Referral. W B Saunders Company; 2012.772-774</ref>. | ||
| Line 135: | Line 127: | ||
*Pectus Excavatum | *Pectus Excavatum | ||
*Diaphragmatic paralysis | *Diaphragmatic paralysis | ||
*Interstitial Fibrosis | *Interstitial Fibrosis<u></u> | ||
<u></u> | |||
== References == | == References == | ||
Revision as of 08:27, 6 April 2021
Original Editors - Kaitlyn Stahl & A.J. Walsh from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Kaitlyn Stahl, Lucinda hampton, Andrew Walsh, Kim Jackson, 127.0.0.1, Elaine Lonnemann, WikiSysop, Vidya Acharya, Kapil Narale, Laura Ritchie, Wendy Walker and Evan Thomas
Introduction[edit | edit source]
Exercise-induced bronchoconstriction (EIB) describes a transient and reversible contraction of bronchial smooth muscle after physical exertion that may or may not produce symptoms of dyspnea, chest tightness, wheezing, and cough. (EIB, previously called Exercise-Induced Asthma)[1].
- EIB occurs in 40% to 90% of people with asthma and up to 20% of those without asthma.
- The benefits of regular exercise for all people are well established, and activity is an integral part of a healthy lifestyle. People suffering from EIB may avoid exertion due to symptoms of breathlessness, cough, chest tightness, and wheezing. Exercise avoidance has been shown to increase social isolation in adolescents, and it can lead to obesity and poor health.
- Exercise has paradoxically been shown to improve EIB severity, pulmonary function, and reduce airway inflammation in people with asthma and EIB.
- Early detection, diagnosis confirmed by the change in lung function during exercise, and treatment can improve quality of life and, when managed appropriately, allows patients to participate freely in exercise without limiting competition at the elite level.[1]
Epidemiology[edit | edit source]
- Exercise-induced bronchoconstriction occurs in 40% to 90% of people with asthma and up to 20% of the general population without asthma.
- Elite athletes have an increased prevalence of 30% to 70%.
- Exercise-induced asthma is the most common medical problem among winter Olympic athletes, especially among cross-country skiers. Nearly 50% of these athletes suffer from the condition, closely followed by short-track speed skaters at 43%[2].
- Approximately 400 million people are projected to have asthma in 2024, with a large percentage expected to have EIB.
- Annually, 250,000 people die from asthma complications[1].
Cause[edit | edit source]
EIB is caused by an acute large increase in the amount of air entering the airways that require heating and humidifying. In susceptible individuals, this results in inflammatory, neuronal, and vascular changes ultimately resulting in contraction of the bronchial smooth muscle and symptoms of dyspnea, cough, chest tightness, mucus production, and wheezing.[1].[3]
Asthma is the result of complex interactions between genetic predisposition and multiple environmental influences. The marked increase in asthma prevalence in the last 3 decades suggests environmental factors as a key contributor in the process of allergic sensitization. [4]
Factors that can trigger or worsen exercise-induced asthma include:
- Cold air
- Dry air
- Air pollution such as smoke or smog
- High pollen counts
- Having a respiratory infection such as a cold
- Chemicals, such as chlorine in swimming pools
No exercise in particular must be avoided if a patient has exercise induced asthma. It is important to note, however, activities that cause the patient to breathe harder are more likely to trigger symptoms.[5]
Characteristics/Clinical Presentation[edit | edit source]
Symptoms of exercise-induced bronchoconstriction can include mild to moderate symptoms of chest tightness, wheezing, coughing, and dyspnea that occurs within 15 minutes after 5 to 8 minutes of high-intensity aerobic training. Reports of severe symptoms with respiratory failure and death occur rarely.
Symptoms:
- occur more often in specific environments with cold, dry air or high concentration of respiratory irritants.
- usually resolve spontaneously within 30 to 90 minutes and induce a refractory period of 1 to 3 hours, where continued exercise does not produce bronchoconstriction. Patients may also be asymptomatic, and therefore EIB may be underdiagnosed.
Risk factors include:
- personal or family history of asthma
- personal history of atopy or allergic rhinitis
- exposure to cigarette smoke,
- participating in high-risk sports. High-risk sports include episodes of exercise greater than 5 to 8 minutes in certain environments (eg cold, dry air or chlorinated pools) such as long-distance running, cycling, cross country or downhill skiing, ice hockey, ice skating, high altitude sports, swimming, water polo, and triathlons.
- living and practicing in areas with high levels of pollution
- female gender. [1]
Associated Co-morbidities[edit | edit source]
One co-morbidity of asthma is status asthmaticus. This is a severe, lifethreatening complication of asthma. With severe bronchospasm the workload of breathing increases five to ten times, leading to acute cor pulmonale. When air is trapped, a severe paradoxic pulse develops as venous return becomes obstructed. This condition can be recognized as a blood pressure drop of more than 10 mm Hg during inspiration. Additionally, pneumothorax can also develop. If status asthmaticus continues, hypoxemia worsens and acidosis begins. If the condition is untreated or not reversed, respiratory or cardiac arrest will occur. Needles to say, an acute asthma episode may lead to a medical emergency.[4]
Adults with asthma are found to have significantly more comorbidities than the general population. These include respiratory infections and allergic rhinitis. High impact/high prevalence chronic conditions such as depression have also been found in one out of four adults with asthma. Children suffering from asthma were found to have fewer comorbidities than adults, but 12.6% had an associated chronic medical condition. The most prevalent co-morbidities found in adults with asthma are time-limited minor infections, while others with a high impact and/or high prevalence are depression, hypertension, diabetes, ischemic heart disease, degenerative joint disease, cardiac arrhythmia, cancer, congestive heart failure, cerebrovascular disease and COPD.[6]
Systemic Involvement[edit | edit source]
Asthma can affect the entire pulmonary system. Often times the lungs become hyperreactive resulting in an exaggerated response to allergens and other irritants. In response, the muscles of the airway constrict, making the ability to breathe more challenging. As this hyperactive response occurs, so also does the process of inflammation. This causes the air passages to become swollen and the cells lining the passages to produce excess mucus, further impairing breathing.[4]
Medical Management[edit | edit source]
Prevention:
American Academy of Allergy, Asthma, and Immunology (AAAAI) promotes utilization of self-management and prevention strategies for patients with asthma. A daily asthma management plan, as well as other information and resources, can be found on the AAAAI website.[4] [7]
'Diagnosis:'
Exercise-Induced Bronchospasms (EIB) is often diagnosed based on the patient’s history of the following symptoms: cough, shortness of breath, chest pain or tightness, wheezing, or endurance problems during exercise. However, EIB has been shown to be misdiagnosed when based on patient history alone. Pulmonary function testing, involving a cardiovascular exercise challenge at 80% of heart rate maximum, is a primary diagnostic tool often used to augment clinical symptom findings. Diagnosis of EIB is indicated with 15-percent decrease in the patient’s PEF or FEV1[8].
Management:
If addressed and treated appropriately, exercise-induced asthma should not restrict one’s ability to fully participate in vigorous physical activity. Furthermore, adequate asthma control should allow for a patient to participate in any activity of choice without experiencing asthma symptoms[8]. Management of EIB should include identifying any allergens the patient may have, educating the patient on avoiding asthma triggers, and use of asthma medications, when necessary[4]. The EPR 3 Guidelines for Diagnosis and Management of Asthma recommend the following treatments for the medical management of EIA[8]:
Long-term Pharmacotherapy (if appropriate):
Anti-inflammatory medications, such as inhaled corticosteroids used to suppress airway inflammation, have been proven to decrease the frequency and severity of EIB when used on a daily basis for long-term control of asthma. Long-term control therapy is recommended for patients with poorly controlled symptoms, including frequent, severe episodes of EIB[8]
Treatments Prior to Exercise[8]:
1. Inhaled beta2-agonists:
- Short Acting Beta Agonists (SABA), often called ‘rescue inhalers’, are used acutely before exercise to control symptoms up to 2-3 hours
- Long Acting Beta Agonists (LABA) are used in conjunction with inhaled corticosteroids to provide additional protection from asthma symptoms for up to 12 hours. LABA are not indicated for daily use but should be used as a pretreatment to exercise.
2. Leukotriene Receptor Antagonists (LTRAs): are medications used for allergy treatment and to prevent asthma symptoms. LTRAs have a longer onset of action and may take hours to provide symptom relief.
3. Exercise Warm Up: A period of warming up before exercise may help to decrease symptoms associated with EIB
4. Protection Against Cold: Wearing a scarf over the mouth prior to/during activity may help to decrease cold-induced EIB
Physical Therapy Management[edit | edit source]
Acute Management:
Because EIB is triggered by exercise, physical therapists may be the first to identify asthma symptoms in a patient with undiagnosed EIB. For this reason, physical therapists must be aware of the associated signs and symptoms of EIB, as well as any red flags that may indicate a need for medical referral and treatment. If a patient has an acute asthma attack during therapy, the physical therapist should assess the severity of the attack, then position the patient in high Fowler’s position for diaphragmatic and pursed-lip breathing, if appropriate. If the patient has an inhaler available, the physical therapist should provide assistance to allow the patient to self-administer the medication, while helping the patient to relax[9].
Long-term Management
There are several factors that can deter patients with EIA from exercising, one being the belief that exercise is detrimental to their condition. Although there is insufficient evidence to support breathing exercises or inspiratory muscle training in patients with asthma, there is strong evidence to support the benefits of physical activity for cardiovascular training in this patient population[9]. Therefore, physical therapists can play a large role in the management of care by providing patient education and exercise prescription. A study protocol will provide the effectiveness of physiotherapy on the quality of life of children with asthma[10].
The Preferred Practice Patterns for this patient population[9], according to the Physical Therapy Guide to Practice[11], include:
- Pattern 6B: Impaired Aerobic Capacity/Endurance Associated With Deconditioning
- Pattern 6C: Impaired Ventilation, Respiration/Gas Exchange, and Aerobic Capacity/Endurance Associated With Airway Clearance Dysfunction
- Pattern 6E: Impaired Ventilation and Respiration/Gas Exchange Associated With Ventilatory Pump Dysfunction or Failure
- Pattern 6F: Impaired Ventilation and Respiration/Gas Exchange Associated With Respiratory Failure
Exercise and Medication:
Bronchodilators should be self-administered with a meter-dose inhaler (MDI) about 20-30 minutes prior before the patient participates in exercise. Mild stretching and a warm-up to exercise should also be performed during that time to help prevent the onset of asthma symptoms. Physical therapists must be aware of any adverse side effects or drug toxicity associated with asthma medications. Some symptoms that may suggest drug toxicity include nausea and vomiting, tremors, anxiety, tachycardia, arrhythmia, and hypotension. If the patient exhibits asthma symptoms during exercise that are not controlled with current medication, the physical therapist should notify the patient’s physician to alter the dosage[9].
Vital Signs:
It is important for the physical therapist to monitor the patient’s vital signs before, during and after exercise, to detect any abnormal changes in bronchopulmonary function. Auscultation of the lungs should be done routinely to detect any abnormal breath sounds, wheezing, or presence of rhonchi. Red flags that may indicate worsening asthma or drug toxicity can include tachypnea (increased respiratory rate above normative values), diarrhea, headache and vomiting. Asthma-related hypoxemia may be indicated with an abnormal rise in the patient’s blood pressure[9]
Other Considerations:
Decreased bone mass density has been associated with long-term use of inhaled corticosteroids in patients with moderate to severe asthma. This chronic corticosteroid use also has an associated increased risk of fracture, in particular asymptomatic vertebral fractures. Physical therapists should be aware of the patient’s medication history and take precautions when exercising patients who may be at risk for fractures. Physical therapy can enhance medical management and play important role in the care of patients with status asthmaticus. Physical therapists can teach the patient various coughing, breathing, and positioning techniques to help clear secretions, reduce hypoxemia and improve V/Q matching. Aggressive treatments, such as forceful percussion, should be avoided in this population to prevent triggering of bronchospasms[9]
Differential Diagnosis[edit | edit source]
The most common differential diagnoses of EIB include[12]:
- Vocal Cord Dysfunction
- Laryngeal/tracheal processes
- Respiratory tract infection
- Gastro-esophageal reflux
- Hyperventilation syndromes
EIB may also be associated with underlying conditions, such as[13]:
- COPD
- Obesity
- Pectus Excavatum
- Diaphragmatic paralysis
- Interstitial Fibrosis
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Gerow M, Bruner PJ. Exercise Induced Asthma. Treasure Island, FL: StatPearls. 2020.Available from: https://www.ncbi.nlm.nih.gov/books/NBK557554/ (accessed 6.4.2021)
- ↑ The Conversation Winter Olympics: why many athletes will be struggling with asthma Available from:https://theconversation.com/winter-olympics-why-many-athletes-will-be-struggling-with-asthma-90400 (accessed 6.4.2021)
- ↑ Asthma org. EIB Available from:https://asthma.org.au/about-asthma/triggers/exercise-induced-bronchoconstriction/ (accessed 6.4.2021)
- ↑ 4.0 4.1 4.2 4.3 4.4 Goodman CC, Snyder TE. Differential Diagnosis for Physical Therapists, Screening for Referral. W B Saunders Company; 2012. 298
- ↑ "Exercise-induced asthma." Mayo Clinic. N.p., n.d. Web. 25 Mar. 2014. <http://www.mayoclinic.org/diseases-conditions/exercise-induced-asthma/basics/definition/con-20033156>.
- ↑ Boulay, Marie-Ève, and Louis-Philippe Boulet. "Asthma-related Comorbidities." Informahealthcare.com. Centre De Recherche De L’Institut Universitaire De Cardiologie Et De Pneumologie De Québec, 2001. Web. 23 Mar. 2014. <http%3A%2F%2Finformahealthcare.com%2Fdoi%2Fpdf%2F10.1586%2Fers.11.34%3FnoFrame%3Dtrue>.
- ↑ The American Academy of Allergy, Asthma and Immunology. Accessed March 25, 2014 at http://www.aaaai.org/home.aspx
- ↑ 8.0 8.1 8.2 8.3 8.4 Expert Panel Report 3 (EPR3): Guidelines for the Diagnosis and Management of Asthma. SECTION 4, MANAGING ASTHMA LONG TERM—SPECIAL SITUATIONS. Accessed March 25, 2014 at http://www.nhlbi.nih.gov/guidelines/asthma.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 Goodman CC, Snyder TE. Differential Diagnosis for Physical Therapists, Screening for Referral. W B Saunders Company; 2012.772-774
- ↑ Zhang W, Liu L, Yang W, Liu H. Effectiveness of physiotherapy on quality of life in children with asthma: Study protocol for a systematic review and meta-analysis. Medicine. 2019 Jun;98(26).
- ↑ APTA Guide to Physical Therapist Practice-Online. Cardiovascular/Pulmonary Preferred Practice Patterns. http://guidetoptpractice.apta.org/content/current
- ↑ Schumacher Y, Pottgiesser T, Dickhuth H. Exercise-induced bronchoconstriction: Asthma in athletes. International Sportmed Journal [serial online]. December 2011;12(4):145-149. Available from: SPORTDiscus with Full Text, Ipswich, MA. Accessed March 25, 2014.
- ↑ Weiler JM, Anderson SD, Randolph C, et al. Pathogenesis, prevalence, diagnosis, and management of exercise-induced bronchoconstriction: a practice parameter. Ann. Allergy. Asthma Immunol. 2010;105(6 Suppl):S1–47. Available at: http://www.ncbi.nlm.nih.gov/pubmed/21167465. Accessed March 25, 2014.