Elbow Ligamentous Injuries: Difference between revisions
No edit summary |
No edit summary |
||
| (40 intermediate revisions by 12 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original Editor ''' [[User:Lydia Armacost|Lydia Armacost]] and [[User:Wendy Matson|Wendy Matson]] as part of the [[Temple University Evidence-Based Practice Project|Temple University EBP Project]] | |||
{ | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}
| ||
</div> | |||
== Introduction == | |||
Ulnar collateral ligament (UCL) injuries of the elbow joint have become common among overhead throwing athletes, particularly baseball pitchers<ref>Fleisig, Glenn S.; Andrews, James R. Prevention of elbow injuries in youth baseball pitchers. Sports health, 2012, 4.5: 419-424.</ref>. Recent studies reported the failure of nonoperative management of UCL injury in overhead athletes<ref>Rettig AC, Sherrill C, Snead DS, Mendler JC, Mieling P. Nonoperative treatment of ulnar collateral ligament injuries in throwing athletes. Am J Sports Med. 2001;29(1):15-17.</ref><ref>Ford GM, Genuario J, Kinkartz J, Githens T, Noonan T. Return-to-Play Outcomes in Professional Baseball Players After Medial Ulnar Collateral Ligament Injuries: Comparison of Operative Versus Nonoperative Treatment Based on Magnetic Resonance Imaging Findings. Am J Sports Med. 2016 Mar;44(3):723-8.</ref><ref>Frangiamore SJ, Lynch TS, Vaughn MD, Soloff L, Forney M, Styron JF, Schickendantz MS. Magnetic Resonance Imaging Predictors of Failure in the Nonoperative Management of Ulnar Collateral Ligament Injuries in Professional Baseball Pitchers. Am J Sports Med''.'' 2017 Jul;45(8):1783-1789.</ref>. On the contrary, UCL reconstructions in baseball players have been proven to be an effective procedure for return to play and performance<ref>Erickson BJ, Nwachukwu BU, Rosas S, Schairer WW, McCormick FM, Bach BR Jr, Bush-Joseph CA, Romeo AA. Trends in Medial Ulnar Collateral Ligament Reconstruction in the United States: A Retrospective Review of a Large Private-Payer Database From 2007 to 2011. Am J Sports Med. 2015 Jul;43(7):1770-4.</ref><ref>Osbahr DC, Cain EL Jr, Raines BT, Fortenbaugh D, Dugas JR, Andrews JR. Long-term Outcomes After Ulnar Collateral Ligament Reconstruction in Competitive Baseball Players: Minimum 10-Year Follow-up. Am J Sports Med. 2014 Jun;42(6):1333-42.</ref><ref name=":0">Hodgins JL, Vitale M, Arons RR, Ahmad CS. Epidemiology of Medial Ulnar Collateral Ligament Reconstruction: A 10-Year Study in New York State. Am J Sports Med. 2016 Mar;44(3):729-34.</ref>. However, the rapidly increasing number of reconstructions is reported in the amateur and adolescent athletes<ref name=":0" /><ref>Jones KJ, Dines JS, Rebolledo BJ, Weeks KD, Williams RJ, Dines DM, Altchek DW. Operative management of ulnar collateral ligament insufficiency in adolescent athletes. Am J Sports Med''.'' 2014 Jan;42(1):117-21.</ref>. The avoidance of unnecessary surgeries associated with long recovery period should be beneficial in specific clinical scenarios<ref>Rebolledo BJ, Dugas JR, Bedi A, Ciccotti MG, Altchek DW, Dines JS. Avoiding Tommy John Surgery: What Are the Alternatives? Am J Sports Med. 2017 Nov;45(13):3143-3148.</ref>. For the nonoperative management for the UCL injuries, such as the rehabilitation, the anatomic and biomechanical understanding of the medial elbow joint is necessary<ref>Hoshika S, Nimura A, Yamaguchi R, Nasu H, Yamaguchi K, Sugaya H, Akita K. Medial elbow anatomy: A paradigm shift for UCL injury prevention and management. Clin Anat. 2019 Apr;32(3):379-389.</ref>. | |||
== Clinically Relevant Anatomy. == | |||
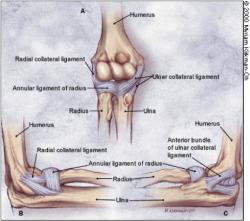
The [[Elbow|elbow joint]] is stabilized primarily by three ligaments: | |||
#[[Medial Collateral Ligament of the Elbow|Medial collateral ligament]] | |||
#Lateral collateral ligament | |||
#Annular ligament | |||
< | The medial and lateral collateral ligaments provide valgus and varus stability, and allow for rotation. The annular ligament encircles the head of the radius, stabilizing it in the radial notch. Each of these ligaments can be injured by elbow trauma or overuse.<ref name="Chumbley">Chumbley E. O'Connor F, Nirschl R. Evaluation of Overuse Elbow Injuries. American Family Physician. Feb 2000. Available at http://www.aafp.org/afp/20000201/691.html. Accessed March 2010.</ref> | ||
[[Image: | [[Image:Elbow Ligaments.png|250x250px|Elbow Ligaments.png]] | ||
The flexor-pronator muscles(FPMs) are secondary dynamic stabilizers and have beenconsidered to exert a protective effect against ulnar collateral ligament (UCL) injury. Anatomical studies indicate that the FPMs lie in a goodposition to protect the UCL. Biomechanical studiesreport that the flexor digitorum superficialis (FDS) muscleplays the greatest role among the FPMs as an activestabilizer against valgus stress.<ref>Hoshika S, Nimura A, Takahashi N, Sugaya H, Akita K. Valgus stability is enhanced by flexor digitorum superficialis muscle contraction of the index and middle fingers. J Orthop Surg Res. 2020 Mar 30;15(1):121.</ref><br> | |||
== Mechanism of Injury / Pathological Process == | |||
< | '''Lateral collateral ligamentous''' injuries are typically associated with fracture or [[Posterior Elbow Dislocation|dislocation]]<ref>Sevivas N, Ferreira N, Pereira H, da Silva MV, Monteiro A, Espregueira MJ. Complex Elbow Dislocations. In: Pederzini L, Eygendaal D, Denti M. (eds) Elbow and Sport. Berlin, Heidelberg, Springer, 2016</ref> (shown below). | ||
'''Medial collateral ligamentous''' injuries are typically caused by overuse<ref>Acosta Batlle J, Cerezal L, López Parra MD, Alba B, Resano S, Blázquez Sánchez J. The elbow: review of anatomy and common collateral ligament complex pathology using MRI. Insights Imaging. 2019 Apr 3;10(1):43.</ref>. Some common causes of elbow ligamentous injuries include: | |||
*Forced twisting of the arm | |||
*Falling on an outstretched arm | |||
*Repeated overhead movement (such as in pitching, volleyball, or tennis) | |||
== Clinical Presentation == | == Clinical Presentation == | ||
Although ligamentous injuries are rare, patients may present with varus or valgus laxity due to overuse or trauma. Lateral Collateral Ligament is often associated with trauma and forceful motion into varus | Although ligamentous injuries are rare, patients may present with varus or valgus laxity due to overuse or trauma. '''Lateral Collateral Ligament''' injury is often associated with trauma and forceful motion into varus. These injuries are commonly associated with a fracture or subluxation at the elbow joint. An '''Ulnar Collateral Ligament''' tear or sprain could occur with valgus overload or stress movement from pitching or throwing. Typically seen in younger male pitchers, a UCL tear or sprain could also be found in athletes involved in repetitive overhead activities like tennis or volleyball. Another common name for UCL tear is [[Little League Elbow|Little League Elbow Syndrome]]. | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
Varus Stress Test, tests for laxity of the Lateral Collateral Ligament. | *[[Elbow Varus Stress|Varus Stress Test]], tests for laxity of the Lateral Collateral Ligament (LCL). | ||
*[[Elbow Valgus Stress|Valgus Stress Test]], tests for laxity of the Ulnar Collateral Ligament (UCL). | |||
Valgus Stress Test, tests for laxity of the Ulnar Collateral Ligament (UCL). | *[[Moving Valgus Stress Test]], tests for chronic UCL sprain or tear from overuse (sensitivity: 100, specificity: 0.75).<ref>O'Driscoll, Shawn WM, Richard L. Lawton, and Adam M. Smith. "The “moving valgus stress test” for medial collateral ligament tears of the elbow." ''The American journal of sports medicine'' 33.2 (2005): 231-239.</ref> | ||
*Modified Milking Maneuver, tests for UCL sprain or tear from overuse. | |||
Moving Valgus Stress Test, | *[[Elbow Examination#Palpation|Palpation]], in order to manually exam the integrity of the ligaments. | ||
== Outcome Measures == | == Outcome Measures == | ||
Three common patient reported outcome measures used for elbow ligamentous injuries: | Three common patient reported outcome measures are used for elbow ligamentous injuries: | ||
#The [[DASH Outcome Measure|DASH]] is 30 questions scored from 0-100, 0 meaning no disability. The DASH is well studied and validated with a minimally clinical important difference or MCID of 15 point or MCD of 12.7 points. | |||
#The Quick DASH, commonly used in place of The DASH. The patient chooses the response that is the most true from 1-5 for each question. The scoring instructions are listed on the bottom of the form, however The Quick DASH has no known MCID unlike the DASH. | |||
#The Patient Specific Functional Scale is a scale where the patient chooses 5 activities that are difficult to perform and rates those tasks from 0-10, 0 being not able and 10 being able. The MCID for the average of the 5 activities is 2, while for 1 activity the MCID is 3. | |||
== Management / Interventions == | |||
Due to lack of high quality literature for these conditions, it is recommended that an impairment-based approach be used to guide management. | |||
*Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used for '''relief of pain and inflammation'''. If pain is severe, a mild narcotic or corticosteroid injections may be prescribed. | |||
*Common '''impairments''' to assess in examination could include decreased elbow or shoulder range of motion, [[Effusion tests|joint effusion]], and decreased strength of the upper extremity musculature. '''Glenohumeral internal rotation deficits''' are typically seen with pitchers and athletes performing repetitive overhead activities. Studies have shown a direct correlation with decreased internal rotation and excessive external rotation in baseball pitchers and UCL injuries.<ref name="Dines">Dines JS, Frank JB, Akerman M, Yocum LA. Glenohumeral Internal Rotation Deficits in Baseball Players with Ulnar Collateral Ligament Insufficiency. American Journal of Sports Medicine.2009 Mar;37(3):566-70</ref> | |||
*It is recommended that individuals with these conditions remain active, while '''protecting the ligament from stress'''. Activities that aggravate the symptoms should initially be minimized in order to allow for ligamentous healing. Activity level can thereafter be increased gradually. | |||
*Pain and swelling may be relieved through the intermittent '''application of [[Cryotherapy|ice]]''' during the acute stages. | |||
*'''Surgery''' for the '''UCL''' is indicated in complete tears and for athletes wanting to resume previous level of activity. The most common surgical procedure, Tommy John surgery, is when the UCL is replaced with a tendon from elsewhere in the body (often from forearm, hamstring, knee or foot of the same patient). This procedure is most common with athletes from several sports, most notably baseball. | |||
*'''Surgery''' to repair the '''LCL''' alone is rare and is typically associated with a fracture, dislocation, or subluxation of the elbow. Due to the decreased structural stability of the joint and ORIF may be considered at the discretion of the surgeon. | |||
== | == Differential Diagnosis == | ||
*[[Heterotopic Ossification]]: Considerable loss of passive range of motion without loss of strength | |||
*Malignancy: Severe progressive pain that is not affected by movement | |||
*Inflammatory Arthrithides: Abnormal systemic signs | |||
*Fracture: History of trauma, [[Elbow extension sign|Elbow Extension Test]] (specificity: 0.69, sensitivity: 0.97), marked limitations in range of motion and ecchymosis | |||
*[[Posterior Elbow Dislocation|Dislocation]]: Exaggerated boney prominence, effusion, or appearance of elongation of forearm and could affect neurovascular status. | |||
*Infection: Sudden swelling without trauma | |||
*Vascular Compromise: numbness, tingling, pulse abnormalities | |||
*[[Referred Pain|Referred Cervical Pain]] | |||
*[[Referred Pain|Referred Shoulder Pain]]<br> | |||
'''Lateral Elbow Differential Diagnosis''' | |||
*Radial Tunnel Syndrome | |||
*[[Lateral Epicondylitis|Lateral Epicondylalgia]]<br> | |||
'''Medial Elbow Differential Diagnosis''' | |||
*[[Cubital Tunnel Syndrome|Cubital Tunnel Syndrome]] | |||
*Medial Epicondylalgia | |||
== General Rehabilitation Guidelines == | |||
Rehabilitation following elbow injury or elbow surgery follows a sequential and progressive multiphased approach. The phases of the rehabilitation program should overlap to ensure proper progression. The ultimate goal of elbow rehabilitation is to return the athlete to his or her previous functional level as quickly and safely as possible<ref>Wilk KE, Macrina LC, Cain EL, Dugas JR, Andrews JR. Rehabilitation of the Overhead Athlete's Elbow. Sports Health. 2012 Sep;4(5):404-14.</ref>. | |||
* '''Phase 1: Immediate Motion''' The first phase of elbow rehabilitation is the immediate motion phase. The goals of this phase are to minimize the effects of immobilization, reestablish nonpainful range of motion (ROM), decrease pain and inflammation, and retard muscular atrophy. | |||
* '''Phase 2: Intermediate''' Phase 2, the intermediate phase, is initiated when the following are achieved: full throwing ROM (as it was prior to the injury), minimal pain and tenderness, and a good (≥ 4/5) manual muscle test of the elbow flexor and extensor musculature. The emphasis of this phase includes maintaining and enhancing elbow and upper extremity mobility, improving muscular strength and endurance, and reestablishing neuromuscular control of the elbow complex. | |||
* '''Phase 3: Advanced Strengthening''' The third phase involves a progression of activities to prepare the athlete for sport participation. The goals of this phase are to gradually increase strength, power, endurance, and neuromuscular control to prepare for a gradual return to sport. Specific criteria that must be met before entering this phase include full nonpainful external and internal rotation total ROM, no pain or tenderness, and strength that is 70% of the contralateral extremity. | |||
* '''Phase 4: Return to Activity''' The final phase of elbow rehabilitation, return to activity, allows the athlete to progressively return to full competition using an interval throwing program. Interval programs are used for the tennis player and golfer. | |||
== References | == References == | ||
<references /> | <references /> | ||
[[Category:Elbow]] | |||
[[Category:Conditions]] | |||
[[Category:Elbow - Conditions]] | |||
[[Category:Musculoskeletal/Orthopaedics]] | |||
[[Category:Temple_Student_Project]] | |||
[[Category:Sports_Injuries]] | |||
[[Category:Primary Contact]] | |||
[[Category:Sports Medicine]] | |||
Latest revision as of 17:54, 17 October 2020
Original Editor Lydia Armacost and Wendy Matson as part of the Temple University EBP Project
Top Contributors - Wataru Okuyama, Wendy Matson, Admin, Rachael Lowe, Kim Jackson, Scott A Burns, Daphne Jackson, Kai A. Sigel, WikiSysop, Lydia Armacost, Laura Ritchie, Naomi O'Reilly, Celine De Wolf, Claire Knott and Wanda van Niekerk
Introduction[edit | edit source]
Ulnar collateral ligament (UCL) injuries of the elbow joint have become common among overhead throwing athletes, particularly baseball pitchers[1]. Recent studies reported the failure of nonoperative management of UCL injury in overhead athletes[2][3][4]. On the contrary, UCL reconstructions in baseball players have been proven to be an effective procedure for return to play and performance[5][6][7]. However, the rapidly increasing number of reconstructions is reported in the amateur and adolescent athletes[7][8]. The avoidance of unnecessary surgeries associated with long recovery period should be beneficial in specific clinical scenarios[9]. For the nonoperative management for the UCL injuries, such as the rehabilitation, the anatomic and biomechanical understanding of the medial elbow joint is necessary[10].
Clinically Relevant Anatomy.[edit | edit source]
The elbow joint is stabilized primarily by three ligaments:
- Medial collateral ligament
- Lateral collateral ligament
- Annular ligament
The medial and lateral collateral ligaments provide valgus and varus stability, and allow for rotation. The annular ligament encircles the head of the radius, stabilizing it in the radial notch. Each of these ligaments can be injured by elbow trauma or overuse.[11]
The flexor-pronator muscles(FPMs) are secondary dynamic stabilizers and have beenconsidered to exert a protective effect against ulnar collateral ligament (UCL) injury. Anatomical studies indicate that the FPMs lie in a goodposition to protect the UCL. Biomechanical studiesreport that the flexor digitorum superficialis (FDS) muscleplays the greatest role among the FPMs as an activestabilizer against valgus stress.[12]
Mechanism of Injury / Pathological Process[edit | edit source]
Lateral collateral ligamentous injuries are typically associated with fracture or dislocation[13] (shown below).
Medial collateral ligamentous injuries are typically caused by overuse[14]. Some common causes of elbow ligamentous injuries include:
- Forced twisting of the arm
- Falling on an outstretched arm
- Repeated overhead movement (such as in pitching, volleyball, or tennis)
Clinical Presentation[edit | edit source]
Although ligamentous injuries are rare, patients may present with varus or valgus laxity due to overuse or trauma. Lateral Collateral Ligament injury is often associated with trauma and forceful motion into varus. These injuries are commonly associated with a fracture or subluxation at the elbow joint. An Ulnar Collateral Ligament tear or sprain could occur with valgus overload or stress movement from pitching or throwing. Typically seen in younger male pitchers, a UCL tear or sprain could also be found in athletes involved in repetitive overhead activities like tennis or volleyball. Another common name for UCL tear is Little League Elbow Syndrome.
Diagnostic Procedures[edit | edit source]
- Varus Stress Test, tests for laxity of the Lateral Collateral Ligament (LCL).
- Valgus Stress Test, tests for laxity of the Ulnar Collateral Ligament (UCL).
- Moving Valgus Stress Test, tests for chronic UCL sprain or tear from overuse (sensitivity: 100, specificity: 0.75).[15]
- Modified Milking Maneuver, tests for UCL sprain or tear from overuse.
- Palpation, in order to manually exam the integrity of the ligaments.
Outcome Measures[edit | edit source]
Three common patient reported outcome measures are used for elbow ligamentous injuries:
- The DASH is 30 questions scored from 0-100, 0 meaning no disability. The DASH is well studied and validated with a minimally clinical important difference or MCID of 15 point or MCD of 12.7 points.
- The Quick DASH, commonly used in place of The DASH. The patient chooses the response that is the most true from 1-5 for each question. The scoring instructions are listed on the bottom of the form, however The Quick DASH has no known MCID unlike the DASH.
- The Patient Specific Functional Scale is a scale where the patient chooses 5 activities that are difficult to perform and rates those tasks from 0-10, 0 being not able and 10 being able. The MCID for the average of the 5 activities is 2, while for 1 activity the MCID is 3.
Management / Interventions[edit | edit source]
Due to lack of high quality literature for these conditions, it is recommended that an impairment-based approach be used to guide management.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used for relief of pain and inflammation. If pain is severe, a mild narcotic or corticosteroid injections may be prescribed.
- Common impairments to assess in examination could include decreased elbow or shoulder range of motion, joint effusion, and decreased strength of the upper extremity musculature. Glenohumeral internal rotation deficits are typically seen with pitchers and athletes performing repetitive overhead activities. Studies have shown a direct correlation with decreased internal rotation and excessive external rotation in baseball pitchers and UCL injuries.[16]
- It is recommended that individuals with these conditions remain active, while protecting the ligament from stress. Activities that aggravate the symptoms should initially be minimized in order to allow for ligamentous healing. Activity level can thereafter be increased gradually.
- Pain and swelling may be relieved through the intermittent application of ice during the acute stages.
- Surgery for the UCL is indicated in complete tears and for athletes wanting to resume previous level of activity. The most common surgical procedure, Tommy John surgery, is when the UCL is replaced with a tendon from elsewhere in the body (often from forearm, hamstring, knee or foot of the same patient). This procedure is most common with athletes from several sports, most notably baseball.
- Surgery to repair the LCL alone is rare and is typically associated with a fracture, dislocation, or subluxation of the elbow. Due to the decreased structural stability of the joint and ORIF may be considered at the discretion of the surgeon.
Differential Diagnosis[edit | edit source]
- Heterotopic Ossification: Considerable loss of passive range of motion without loss of strength
- Malignancy: Severe progressive pain that is not affected by movement
- Inflammatory Arthrithides: Abnormal systemic signs
- Fracture: History of trauma, Elbow Extension Test (specificity: 0.69, sensitivity: 0.97), marked limitations in range of motion and ecchymosis
- Dislocation: Exaggerated boney prominence, effusion, or appearance of elongation of forearm and could affect neurovascular status.
- Infection: Sudden swelling without trauma
- Vascular Compromise: numbness, tingling, pulse abnormalities
- Referred Cervical Pain
- Referred Shoulder Pain
Lateral Elbow Differential Diagnosis
- Radial Tunnel Syndrome
- Lateral Epicondylalgia
Medial Elbow Differential Diagnosis
- Cubital Tunnel Syndrome
- Medial Epicondylalgia
General Rehabilitation Guidelines[edit | edit source]
Rehabilitation following elbow injury or elbow surgery follows a sequential and progressive multiphased approach. The phases of the rehabilitation program should overlap to ensure proper progression. The ultimate goal of elbow rehabilitation is to return the athlete to his or her previous functional level as quickly and safely as possible[17].
- Phase 1: Immediate Motion The first phase of elbow rehabilitation is the immediate motion phase. The goals of this phase are to minimize the effects of immobilization, reestablish nonpainful range of motion (ROM), decrease pain and inflammation, and retard muscular atrophy.
- Phase 2: Intermediate Phase 2, the intermediate phase, is initiated when the following are achieved: full throwing ROM (as it was prior to the injury), minimal pain and tenderness, and a good (≥ 4/5) manual muscle test of the elbow flexor and extensor musculature. The emphasis of this phase includes maintaining and enhancing elbow and upper extremity mobility, improving muscular strength and endurance, and reestablishing neuromuscular control of the elbow complex.
- Phase 3: Advanced Strengthening The third phase involves a progression of activities to prepare the athlete for sport participation. The goals of this phase are to gradually increase strength, power, endurance, and neuromuscular control to prepare for a gradual return to sport. Specific criteria that must be met before entering this phase include full nonpainful external and internal rotation total ROM, no pain or tenderness, and strength that is 70% of the contralateral extremity.
- Phase 4: Return to Activity The final phase of elbow rehabilitation, return to activity, allows the athlete to progressively return to full competition using an interval throwing program. Interval programs are used for the tennis player and golfer.
References[edit | edit source]
- ↑ Fleisig, Glenn S.; Andrews, James R. Prevention of elbow injuries in youth baseball pitchers. Sports health, 2012, 4.5: 419-424.
- ↑ Rettig AC, Sherrill C, Snead DS, Mendler JC, Mieling P. Nonoperative treatment of ulnar collateral ligament injuries in throwing athletes. Am J Sports Med. 2001;29(1):15-17.
- ↑ Ford GM, Genuario J, Kinkartz J, Githens T, Noonan T. Return-to-Play Outcomes in Professional Baseball Players After Medial Ulnar Collateral Ligament Injuries: Comparison of Operative Versus Nonoperative Treatment Based on Magnetic Resonance Imaging Findings. Am J Sports Med. 2016 Mar;44(3):723-8.
- ↑ Frangiamore SJ, Lynch TS, Vaughn MD, Soloff L, Forney M, Styron JF, Schickendantz MS. Magnetic Resonance Imaging Predictors of Failure in the Nonoperative Management of Ulnar Collateral Ligament Injuries in Professional Baseball Pitchers. Am J Sports Med. 2017 Jul;45(8):1783-1789.
- ↑ Erickson BJ, Nwachukwu BU, Rosas S, Schairer WW, McCormick FM, Bach BR Jr, Bush-Joseph CA, Romeo AA. Trends in Medial Ulnar Collateral Ligament Reconstruction in the United States: A Retrospective Review of a Large Private-Payer Database From 2007 to 2011. Am J Sports Med. 2015 Jul;43(7):1770-4.
- ↑ Osbahr DC, Cain EL Jr, Raines BT, Fortenbaugh D, Dugas JR, Andrews JR. Long-term Outcomes After Ulnar Collateral Ligament Reconstruction in Competitive Baseball Players: Minimum 10-Year Follow-up. Am J Sports Med. 2014 Jun;42(6):1333-42.
- ↑ 7.0 7.1 Hodgins JL, Vitale M, Arons RR, Ahmad CS. Epidemiology of Medial Ulnar Collateral Ligament Reconstruction: A 10-Year Study in New York State. Am J Sports Med. 2016 Mar;44(3):729-34.
- ↑ Jones KJ, Dines JS, Rebolledo BJ, Weeks KD, Williams RJ, Dines DM, Altchek DW. Operative management of ulnar collateral ligament insufficiency in adolescent athletes. Am J Sports Med. 2014 Jan;42(1):117-21.
- ↑ Rebolledo BJ, Dugas JR, Bedi A, Ciccotti MG, Altchek DW, Dines JS. Avoiding Tommy John Surgery: What Are the Alternatives? Am J Sports Med. 2017 Nov;45(13):3143-3148.
- ↑ Hoshika S, Nimura A, Yamaguchi R, Nasu H, Yamaguchi K, Sugaya H, Akita K. Medial elbow anatomy: A paradigm shift for UCL injury prevention and management. Clin Anat. 2019 Apr;32(3):379-389.
- ↑ Chumbley E. O'Connor F, Nirschl R. Evaluation of Overuse Elbow Injuries. American Family Physician. Feb 2000. Available at http://www.aafp.org/afp/20000201/691.html. Accessed March 2010.
- ↑ Hoshika S, Nimura A, Takahashi N, Sugaya H, Akita K. Valgus stability is enhanced by flexor digitorum superficialis muscle contraction of the index and middle fingers. J Orthop Surg Res. 2020 Mar 30;15(1):121.
- ↑ Sevivas N, Ferreira N, Pereira H, da Silva MV, Monteiro A, Espregueira MJ. Complex Elbow Dislocations. In: Pederzini L, Eygendaal D, Denti M. (eds) Elbow and Sport. Berlin, Heidelberg, Springer, 2016
- ↑ Acosta Batlle J, Cerezal L, López Parra MD, Alba B, Resano S, Blázquez Sánchez J. The elbow: review of anatomy and common collateral ligament complex pathology using MRI. Insights Imaging. 2019 Apr 3;10(1):43.
- ↑ O'Driscoll, Shawn WM, Richard L. Lawton, and Adam M. Smith. "The “moving valgus stress test” for medial collateral ligament tears of the elbow." The American journal of sports medicine 33.2 (2005): 231-239.
- ↑ Dines JS, Frank JB, Akerman M, Yocum LA. Glenohumeral Internal Rotation Deficits in Baseball Players with Ulnar Collateral Ligament Insufficiency. American Journal of Sports Medicine.2009 Mar;37(3):566-70
- ↑ Wilk KE, Macrina LC, Cain EL, Dugas JR, Andrews JR. Rehabilitation of the Overhead Athlete's Elbow. Sports Health. 2012 Sep;4(5):404-14.