Effects of Ageing on Bone: Difference between revisions
No edit summary |
No edit summary |
||
| Line 37: | Line 37: | ||
=== Prevention === | === Prevention === | ||
[[File:Gym ladies.jpeg|thumb|Ladies gym]] | For more see the informative on prevention, management and physiotherapy for osteoporosis see [[Osteoporosis]] [[File:Gym ladies.jpeg|thumb|Ladies gym]] | ||
[[Therapeutic Exercise|Exercise]] is important | [[Therapeutic Exercise|Exercise]]: Ageing is associated with reduced physical activity and mechanical loading. Decreased mechanical loading exerts a decreased effect upon osteoblasts. Functional loading has been shown to improve bone mass in humans. However exercise training programs can prevent or reverse almost 1% of bone loss per year in both lumbar spine (LS) and femoral neck (FN) for both premenopausal and postmenopausal women.<ref name=":1" /> | ||
It is important exercise to preserve bone density, however care must be taken to avoid high-impact exercises and exercises that present the risk of falling. Functional loading exercises include: | |||
*Weight-bearing exercises e.g. [[Walking: Muscles used|walking]] | *Weight-bearing exercises e.g. [[Walking: Muscles used|walking]] | ||
*[[Strength Training|Strengthening exercises]] using free weights, elastic bands, [[Dumbbell Exercise|dumbbells]] etc. | *[[Strength Training|Strengthening exercises]] using free weights, elastic bands, [[Dumbbell Exercise|dumbbells]] etc. | ||
*[[Balance]] exercises e.g. [[Tai Chi and the Older Person|tai chi]]<br> | *[[Balance]] exercises e.g. [[Tai Chi and the Older Person|tai chi]]<br> | ||
A healthy diet, including adequate dosage of Vitamin D and Calcium, is also useful for preserving bone mass. And it is important to limit [[Caffeine and Exercise|coffee]], alcohol and tobacco consumption as they may have deleterious effect on bone mineral density<ref>http://www.nlm.nih.gov/medlineplus/ency/article/000360.htm</ref><ref>Coronado-Zarco R, de León AO, García-Lara A, Quinzaños-Fresnedo J, Nava-Bringas TI, Macías-Hernández SI. Nonpharmacological interventions for osteoporosis treatment: Systematic review of clinical practice guidelines. Osteoporosis and sarcopenia. 2019 Sep 1;5(3):69-77.</ref> | [[Nutrition|Diet]]: A healthy diet, including adequate dosage of Vitamin D and Calcium, is also useful for preserving bone mass. And it is important to limit [[Caffeine and Exercise|coffee]], alcohol and tobacco consumption as they may have deleterious effect on bone mineral density<ref>http://www.nlm.nih.gov/medlineplus/ency/article/000360.htm</ref><ref>Coronado-Zarco R, de León AO, García-Lara A, Quinzaños-Fresnedo J, Nava-Bringas TI, Macías-Hernández SI. Nonpharmacological interventions for osteoporosis treatment: Systematic review of clinical practice guidelines. Osteoporosis and sarcopenia. 2019 Sep 1;5(3):69-77.</ref>. | ||
== See [[Age and Exercise]] == | == See [[Age and Exercise]] == | ||
Revision as of 02:38, 3 December 2022
Original Editor Oyemi Sillo
Top Contributors - Lucinda hampton, Esraa Mohamed Abdullzaher, Oyemi Sillo, Andeela Hafeez, Tolulope Adeniji, Kim Jackson, Lauren Lopez, Tony Lowe, Scott Buxton, WikiSysop and Jasrah JavedIntroduction[edit | edit source]
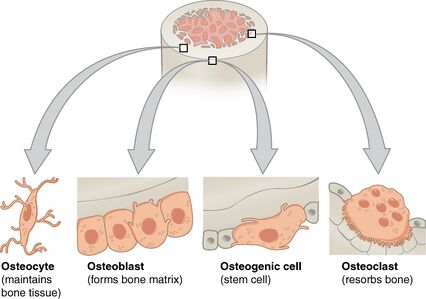
As a result of the ageing process, bone deteriorates in composition, structure and function, which predisposes to osteoporosis. Bone is a dynamic organ that serves mechanical and homeostatic functions. It undergoes a continual self-regeneration process called remodelling ie removing old bone and replacing it with new bone. Bone formation and bone resorption is coupled tightly in a balance to maintain bone mass and strength. With aging this balance moves in a negative direction, resulting in greater bone resorption than bone formation. This combination of bone mass deficiency and reduction in strength ultimately results in osteoporosis and insufficiency fractures.[1]
Ageing Bone Dynamics[edit | edit source]
As people age the rate of bone resorption by osteoclast cells (multinucleated cells which contain mitochondria and lysosomes that is responsible for bone resorption) exceeds the rate of bone formation so bone weaken.[2] The reasons for this are multi factorial, including:.
Non-Modifiable Risk Factor
- Genetics eg family history of osteoporosis
- Peak bone mass accrual in youth
- Alterations in cellular components
- Older than 50 years of age
- Comorbid medical conditions eg Hyperthyroidism, Hyperparathyroidism
- Premature birth
- Hormonal, biochemical and vasculature status eg low levels of estrogen
- Sarcopenia
- Seizure disorder[3]
Modifiable Risk Factor
- Nutrition eg Calcium intake of less than 1200 mg/day, Insufficient protein intake, Inadequate Vitamin D intake, BMI <18.5,
- Physical activity,
- Drugs eg Excessive intake of alcohol, Cigarette smoking[3][1]
Adverse Affects of Bone Changes[edit | edit source]
Osteoporosis: a major cause of hip fractures in the elderly, a type of insufficiency fracture
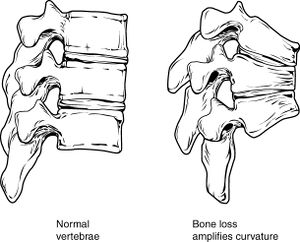
Spinal Compression Fracture: Most occur at the thoracolumbar junction. 40% of the women over 80 years have received at least one compression fracture.[4]See also Osteoporotic Vertebral Fractures
Reduced bone density of the vertebrae: Combined with the loss of fluid in intervertebral discs, result in a curved and shortened spine and possible poor posture, leads to pain, reduced mobility, and other musculoskeletal problems.[5][6]
Prevention[edit | edit source]
For more see the informative on prevention, management and physiotherapy for osteoporosis see Osteoporosis
Exercise: Ageing is associated with reduced physical activity and mechanical loading. Decreased mechanical loading exerts a decreased effect upon osteoblasts. Functional loading has been shown to improve bone mass in humans. However exercise training programs can prevent or reverse almost 1% of bone loss per year in both lumbar spine (LS) and femoral neck (FN) for both premenopausal and postmenopausal women.[1]
It is important exercise to preserve bone density, however care must be taken to avoid high-impact exercises and exercises that present the risk of falling. Functional loading exercises include:
- Weight-bearing exercises e.g. walking
- Strengthening exercises using free weights, elastic bands, dumbbells etc.
- Balance exercises e.g. tai chi
Diet: A healthy diet, including adequate dosage of Vitamin D and Calcium, is also useful for preserving bone mass. And it is important to limit coffee, alcohol and tobacco consumption as they may have deleterious effect on bone mineral density[7][8].
See Age and Exercise[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Demontiero O, Vidal C, Duque G. Aging and bone loss: new insights for the clinician. Therapeutic advances in musculoskeletal disease. 2012 Apr;4(2):61-76. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3383520/ (accessed 2.12.2022)
- ↑ https://www.boundless.com/physiology/textbooks/boundless-anatomy-and-physiology-textbook/appendix-b-development-and-aging-of-the-organ-systems-1417/bone-development-1497/bone-tissue-and-the-effects-of-aging-1500-11222/
- ↑ 3.0 3.1 Andrew A, Rita A, Dale A. Geriatric Physical Therapy. Third Edition. Elsevier Mosby. 2012
- ↑ Lumbar Compression Fracture
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/004015.htm
- ↑ https://medlineplus.gov/ency/article/004015.htm
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/000360.htm
- ↑ Coronado-Zarco R, de León AO, García-Lara A, Quinzaños-Fresnedo J, Nava-Bringas TI, Macías-Hernández SI. Nonpharmacological interventions for osteoporosis treatment: Systematic review of clinical practice guidelines. Osteoporosis and sarcopenia. 2019 Sep 1;5(3):69-77.