Diaphragm Anatomy and Differential Diagnosis: Difference between revisions
Kim Jackson (talk | contribs) m (Changed protection level for "Diaphragm Anatomy and Differential Diagnosis": Course Page ([Edit=⧼protect-level-ppadmin⧽] (indefinite) [Move=⧼protect-level-ppadmin⧽] (indefinite))) |
No edit summary |
||
| Line 7: | Line 7: | ||
* It forms the floor of the thorax and the roof of the abdomen<ref name=":0" /><ref>Kurian J. [https://link.springer.com/chapter/10.1007/978-3-030-31989-2_6 Chest Wall and Diaphragm]. InPediatric Body MRI 2020 (pp. 159-192). Springer, Cham.</ref> | * It forms the floor of the thorax and the roof of the abdomen<ref name=":0" /><ref>Kurian J. [https://link.springer.com/chapter/10.1007/978-3-030-31989-2_6 Chest Wall and Diaphragm]. InPediatric Body MRI 2020 (pp. 159-192). Springer, Cham.</ref> | ||
* The left side is lower than the right due to presence of the liver on the right<ref name=":0" /> | * The left side is lower than the right due to presence of the liver on the right<ref name=":0" /> | ||
* The left side may also be located partially inferiorly due to the "push" by the heart<ref name=":0" /><ref>Bordoni B, Purgol S, Bizzarri A, Modica M, Morabito B. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6070065/ The influence of breathing on the central nervous system.] Cureus. 2018 Jun;10(6).</ref><ref>Oliver KA, Ashurst JV. [https://pubmed.ncbi.nlm.nih.gov/30020697/ Anatomy, Thorax, Phrenic Nerves.] InStatPearls [Internet] 2020 Jul 27. StatPearls Publishing.</ref> | * The left side may also be located partially inferiorly due to the "push" by the [[Anatomy of the Human Heart|heart]]<ref name=":0" /><ref>Bordoni B, Purgol S, Bizzarri A, Modica M, Morabito B. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6070065/ The influence of breathing on the central nervous system.] Cureus. 2018 Jun;10(6).</ref><ref>Oliver KA, Ashurst JV. [https://pubmed.ncbi.nlm.nih.gov/30020697/ Anatomy, Thorax, Phrenic Nerves.] InStatPearls [Internet] 2020 Jul 27. StatPearls Publishing.</ref> | ||
* The peripheral portion of the diaphragm is muscular and is composed of three distinct muscle groups: | * The peripheral portion of the diaphragm is muscular and is composed of three distinct muscle groups: | ||
** The sternal group originates from the xiphoid process | ** The [[Sternum|sternal]] group originates from the xiphoid process | ||
** The costal group originates from the inferior surface of the six lower ribs | ** The costal group originates from the inferior surface of the six lower [[ribs]] | ||
** The lumbar group originates from the two crura and the arcuate ligaments, which are in turn inserted into L1 and L2, and sometimes L3 as well | ** The [[lumbar]] group originates from the two crura and the arcuate ligaments, which are in turn inserted into L1 and L2, and sometimes L3 as well | ||
* The central portion of the diaphragm is made up of very strong aponeurotic tendinous ligaments without any bony attachment. | * The central portion of the diaphragm is made up of very strong [[Aponeurosis|aponeurotic]] tendinous ligaments without any bony attachment. | ||
== Major Openings in the Diaphragm == | == Major Openings in the Diaphragm == | ||
[[File:Henry Vandyke Carter, Public domain, via Wikimedia Commons.png|thumb|Diaphragm Anatomy]] | [[File:Henry Vandyke Carter, Public domain, via Wikimedia Commons.png|thumb|Diaphragm Anatomy]] | ||
# '''Caval hiatus:''' at the level of the T8 vertebra in the central tendon. Allows passage of the inferior vena cava and some right phrenic nerve branches.<ref name=":0" /> | # '''Caval hiatus:''' at the level of the T8 vertebra in the central tendon. Allows passage of the inferior [[Vena Cava|vena cava]] and some right [[Phrenic Nerve|phrenic nerve]] branches.<ref name=":0" /> | ||
# '''Oesophageal hiatus:''' at the level of the T10. It allows the oesophagus, the right and left vagus trunks, the oesophageal branches of the left gastric vessels, and the lymph vessels to pass through.<ref name=":0" /> | # '''Oesophageal hiatus:''' at the level of the T10. It allows the oesophagus, the right and left [[Vagus Nerve|vagus]] trunks, the oesophageal branches of the left gastric vessels, and the [[Lymphatic System|lymph]] vessels to pass through.<ref name=":0" /> | ||
# '''Aortic hiatus:''' anterior to the T12 vertebral body between the crura. Allows the aorta, thoracic duct, and azygos vein to pass through.<ref name=":0" /> | # '''Aortic hiatus:''' anterior to the T12 vertebral body between the crura. Allows the [[aorta]], thoracic duct, and azygos vein to pass through.<ref name=":0" /> | ||
== Nerve Supply == | == Nerve Supply == | ||
| Line 33: | Line 33: | ||
*# The phrenic nerve innervates the parietal pleura and the peritoneum which covers the diaphragm's central surfaces. The periphery of the diaphragm is innervated by the bottom six intercostal nerves.<ref name=":0" /> | *# The phrenic nerve innervates the parietal pleura and the peritoneum which covers the diaphragm's central surfaces. The periphery of the diaphragm is innervated by the bottom six intercostal nerves.<ref name=":0" /> | ||
*# The phrenic nerve is made up of large-diameter myelinated, small-diameter myelinated, and unmyelinated fibres. The large diameter fibres fire when the diaphragm contracts while the small diameter fibers fire throughout respiration.<ref>Nair J, Streeter KA, Turner SM, Sunshine MD, Bolser DC, Fox EJ, Davenport PW, Fuller DD. [https://journals.physiology.org/doi/full/10.1152/jn.00484.2017 Anatomy and physiology of phrenic afferent neurons.] Journal of neurophysiology. 2017 Dec 1;118(6):2975-90.</ref> | *# The phrenic nerve is made up of large-diameter myelinated, small-diameter myelinated, and unmyelinated fibres. The large diameter fibres fire when the diaphragm contracts while the small diameter fibers fire throughout respiration.<ref>Nair J, Streeter KA, Turner SM, Sunshine MD, Bolser DC, Fox EJ, Davenport PW, Fuller DD. [https://journals.physiology.org/doi/full/10.1152/jn.00484.2017 Anatomy and physiology of phrenic afferent neurons.] Journal of neurophysiology. 2017 Dec 1;118(6):2975-90.</ref> | ||
*#* Activation of the phrenic nerve modulates the sympathetic motor outflow.<ref name=":0" /> | *#* Activation of the phrenic nerve modulates the [[Sympathetic Nervous System|sympathetic]] motor outflow.<ref name=":0" /> | ||
*#* Phrenic afferents are also involved in the somatosensation of the diaphragm and they make individuals aware of their breathing while they are awake.<ref name=":0" /> | *#* Phrenic afferents are also involved in the [[somatosensation]] of the diaphragm and they make individuals aware of their breathing while they are awake.<ref name=":0" /> | ||
== Vascular Supply == | == Vascular Supply == | ||
'''Arterial supply:''' | '''Arterial supply:''' | ||
* Inferior phrenic artery from abdominal | * Inferior phrenic artery from abdominal aorta | ||
* Superior phrenic artery | * Superior phrenic artery | ||
* Pericardiophrenic, musculophrenic arteries | * Pericardiophrenic, musculophrenic arteries | ||
| Line 48: | Line 48: | ||
=== 1. Vertebrae === | === 1. Vertebrae === | ||
* Medial lumbocostal arch<ref name=":0" /> | * Medial lumbocostal arch<ref name=":0" /> | ||
** A tendinous arch in the fascia which covers [[Psoas Major|psoas major]] | ** A tendinous arch in the [[fascia]] which covers [[Psoas Major|psoas major]] | ||
** Medially, it attaches to the side of the L1 vertebral body | ** Medially, it attaches to the side of the L1 vertebral body | ||
** Laterally, it attaches at the front of the L1 transverse process | ** Laterally, it attaches at the front of the L1 transverse process | ||
| Line 58: | Line 58: | ||
=== 2. Muscles === | === 2. Muscles === | ||
* Quadratus lumborum (QL) attaches to the inferior portion of the 12th rib. A part of the diaphragm attaches to this rib's superior portion. The fascia is continuous between these attachments.<ref name=":2">Pandya R. Diaphragm Anatomy and Differential Diagnosis Course. Physioplus, 2021.</ref> | * [[Quadratus Lumborum|Quadratus lumborum]] (QL) attaches to the inferior portion of the 12th rib. A part of the diaphragm attaches to this rib's superior portion. The fascia is continuous between these attachments.<ref name=":2">Pandya R. Diaphragm Anatomy and Differential Diagnosis Course. Physioplus, 2021.</ref> | ||
* The psoas muscle is in a similar area as the QL. It blends with the fascia at the proximal end of the posterior portion of the diaphragm.<ref name=":2" /> | * The [[Psoas Major|psoas]] muscle is in a similar area as the QL. It blends with the fascia at the proximal end of the posterior portion of the diaphragm.<ref name=":2" /> | ||
== Aetiology of an Elevated Diaphragm == | == Aetiology of an Elevated Diaphragm == | ||
| Line 67: | Line 67: | ||
# Above the diaphragm | # Above the diaphragm | ||
#* Decreased lung volume | #* Decreased [[Lung Volumes|lung volume]] | ||
#* [[Atelectasis]]/collapse | #* [[Atelectasis]]/collapse | ||
#* Prior lobectomy or pneumonectomy | #* Prior lobectomy or pneumonectomy | ||
| Line 73: | Line 73: | ||
# At the level of the diaphragm | # At the level of the diaphragm | ||
#* Phrenic nerve palsy | #* Phrenic nerve palsy | ||
#* Diaphragmatic eventration | #* Diaphragmatic eventration (an abnormal placement of the diaphragm, located too high in the body, either due to issues with the nerves that supply the muscle, or the muscle itself. In more severe cases, this can compress the lungs and interfere with breathing)<ref>Columbia Surgery Diaphragm Eventration Available:https://columbiasurgery.org/conditions-and-treatments/diaphragm-eventration (accessed 9.5.2022)</ref>. | ||
#* Contralateral [[stroke]]: usually middle cerebral artery (MCA) distribution | #* Contralateral [[stroke]]: usually middle cerebral artery (MCA) distribution | ||
# Below the diaphragm | # Below the diaphragm | ||
| Line 92: | Line 92: | ||
*'''Mechanical trauma:''' such as nerve damage / ligation during surgery | *'''Mechanical trauma:''' such as nerve damage / ligation during surgery | ||
*'''Compression:''' due to a chest cavity tumour | *'''Compression:''' due to a chest cavity tumour | ||
*'''Myopathies:''' including myasthenia gravis | *'''Myopathies:''' including [[Myasthenia Gravis|myasthenia gravis]] | ||
*'''Neuropathic:''' including conditions such as diabetic neuropathy, inclusion body myositis, [[dermatomyositis]], [[Multiple Sclerosis (MS)|multiple sclerosis]], anterior horn cell disease, chronic demyelinating disease, and neuralgic myopathy | *'''Neuropathic:''' including conditions such as [[Diabetic Neuropathy|diabetic neuropathy]], inclusion body [[Myositis Ossificans|myositis]], [[dermatomyositis]], [[Multiple Sclerosis (MS)|multiple sclerosis]], anterior horn cell disease, chronic demyelinating disease, and neuralgic [[Myopathies|myopathy]] | ||
*''' Inflammation:''' a number of systemic diseases can cause inflammation in the phrenic nerve / diaphragm, which results in diaphragmatic palsy. Examples include: | *''' Inflammation:''' a number of systemic diseases can cause inflammation in the phrenic nerve / diaphragm, which results in diaphragmatic palsy. Examples include: | ||
** Viral infections (e.g. [[Human Immunodeficiency Virus (HIV)|HIV]], West Nile virus and poliomyelitis virus) | ** [[Viral Infections|Viral]] infections (e.g. [[Human Immunodeficiency Virus (HIV)|HIV]], West Nile virus and [[poliomyelitis]] virus) | ||
** Bacterial infections (e.g. [[Lyme Disease|Lyme disease]]) | ** [[Bacterial Infections|Bacterial]] infections (e.g. [[Lyme Disease|Lyme disease]]) | ||
** Non-infectious causes (e.g. [[sarcoidosis]] and amyloidosis) | ** Non-infectious causes (e.g. [[sarcoidosis]] and amyloidosis) | ||
| Line 102: | Line 102: | ||
=== Differential Diagnosis for Paralysis of the Diaphragm === | === Differential Diagnosis for Paralysis of the Diaphragm === | ||
* Alveolar hypoventilation | * [[Alveoli|Alveolar]] hypoventilation | ||
* Anterior horn cell or neuromuscular junction disease | * Anterior horn cell or neuromuscular junction disease | ||
* Cerebral haemorrhage | * Cerebral haemorrhage | ||
Revision as of 04:46, 9 May 2022
Top Contributors - Carin Hunter, Jess Bell, Kim Jackson, Wanda van Niekerk, Lucinda hampton, Merinda Rodseth, Ewa Jaraczewska and Tarina van der Stockt
Anatomy of the Diaphragm[edit | edit source]
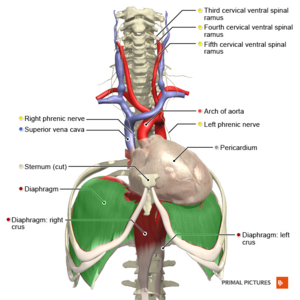
The diaphragm is a major muscle of respiration.[1]
- It is a dome-shaped, "fibromuscular sheet" that separates the thorax from the abdomen[2]
- It forms the floor of the thorax and the roof of the abdomen[2][3]
- The left side is lower than the right due to presence of the liver on the right[2]
- The left side may also be located partially inferiorly due to the "push" by the heart[2][4][5]
- The peripheral portion of the diaphragm is muscular and is composed of three distinct muscle groups:
- The central portion of the diaphragm is made up of very strong aponeurotic tendinous ligaments without any bony attachment.
Major Openings in the Diaphragm[edit | edit source]
- Caval hiatus: at the level of the T8 vertebra in the central tendon. Allows passage of the inferior vena cava and some right phrenic nerve branches.[2]
- Oesophageal hiatus: at the level of the T10. It allows the oesophagus, the right and left vagus trunks, the oesophageal branches of the left gastric vessels, and the lymph vessels to pass through.[2]
- Aortic hiatus: anterior to the T12 vertebral body between the crura. Allows the aorta, thoracic duct, and azygos vein to pass through.[2]
Nerve Supply[edit | edit source]
The diaphragm is supplied by the right and left phrenic nerves:[2] C3, C4, C5 and sometimes C6. Each phrenic nerve divides into four trunks.[6]
- Motor nerve supply:[7]
- Left hemidiaphragm is supplied by the left phrenic nerve
- Right hemidiaphragm is supplied by the right phrenic nerve
- Sensory nerve supply:
- The phrenic nerve innervates the parietal pleura and the peritoneum which covers the diaphragm's central surfaces. The periphery of the diaphragm is innervated by the bottom six intercostal nerves.[2]
- The phrenic nerve is made up of large-diameter myelinated, small-diameter myelinated, and unmyelinated fibres. The large diameter fibres fire when the diaphragm contracts while the small diameter fibers fire throughout respiration.[8]
- Activation of the phrenic nerve modulates the sympathetic motor outflow.[2]
- Phrenic afferents are also involved in the somatosensation of the diaphragm and they make individuals aware of their breathing while they are awake.[2]
Vascular Supply[edit | edit source]
Arterial supply:
- Inferior phrenic artery from abdominal aorta
- Superior phrenic artery
- Pericardiophrenic, musculophrenic arteries
Venous supply:
- Inferior phrenic vein
Fascial Attachments[edit | edit source]
1. Vertebrae[edit | edit source]
- Medial lumbocostal arch[2]
- A tendinous arch in the fascia which covers psoas major
- Medially, it attaches to the side of the L1 vertebral body
- Laterally, it attaches at the front of the L1 transverse process
- Lateral lumbocostal arch[2]
- A tendinous arch in the fascia which covers the upper portion of quadratus lumborum
- Medially, it attaches to the front of the L1 transverse process
- Laterally, it attaches to the lower border of rib 12
2. Muscles[edit | edit source]
- Quadratus lumborum (QL) attaches to the inferior portion of the 12th rib. A part of the diaphragm attaches to this rib's superior portion. The fascia is continuous between these attachments.[9]
- The psoas muscle is in a similar area as the QL. It blends with the fascia at the proximal end of the posterior portion of the diaphragm.[9]
Aetiology of an Elevated Diaphragm[edit | edit source]
An elevated hemidiaphragm may be due to both direct and indirect causes.
The causes can be grouped into three categories based on the location of the cause, including:[7][9]
- Above the diaphragm
- Decreased lung volume
- Atelectasis/collapse
- Prior lobectomy or pneumonectomy
- Pulmonary hypoplasia
- At the level of the diaphragm
- Phrenic nerve palsy
- Diaphragmatic eventration (an abnormal placement of the diaphragm, located too high in the body, either due to issues with the nerves that supply the muscle, or the muscle itself. In more severe cases, this can compress the lungs and interfere with breathing)[10].
- Contralateral stroke: usually middle cerebral artery (MCA) distribution
- Below the diaphragm
- Abdominal tumour, e.g. liver metastases or primary malignancy
- Subphrenic abscess
- Distended stomach or colon, including Chilaiditi sign/syndrome
Differential Diagnosis for Elevated Diaphragm[edit | edit source]
Other situations which may mimic an elevated hemidiaphragm include:[7]
- Subpulmonic effusion
- Diaphragmatic hernia
- Diaphragmatic rupture
- Tumour of the pleura or diaphragm
Aetiology for Paralysis of the Diaphragm[edit | edit source]
Diaphragmatic paralysis occurs when the nerve supply is interrupted. This interruption might occur in the phrenic nerve itself, at the cervical spinal cord, or in the brainstem. However, it is most commonly caused by a phrenic nerve lesion:[6][11]
- Mechanical trauma: such as nerve damage / ligation during surgery
- Compression: due to a chest cavity tumour
- Myopathies: including myasthenia gravis
- Neuropathic: including conditions such as diabetic neuropathy, inclusion body myositis, dermatomyositis, multiple sclerosis, anterior horn cell disease, chronic demyelinating disease, and neuralgic myopathy
- Inflammation: a number of systemic diseases can cause inflammation in the phrenic nerve / diaphragm, which results in diaphragmatic palsy. Examples include:
- Viral infections (e.g. HIV, West Nile virus and poliomyelitis virus)
- Bacterial infections (e.g. Lyme disease)
- Non-infectious causes (e.g. sarcoidosis and amyloidosis)
- Idiopathic: around 20 percent of cases have no obvious cause
Differential Diagnosis for Paralysis of the Diaphragm[edit | edit source]
- Alveolar hypoventilation
- Anterior horn cell or neuromuscular junction disease
- Cerebral haemorrhage
- Cervical fracture
- Decreased pulmonary compliance
- Guillain-Barre syndrome
- Myasthenia gravis
- Peripheral neuropathies
- Pleural adhesions[6]
Symptoms of Diaphragmatic Weakness[edit | edit source]
- Unilateral weakness: Often asymptomatic and detected incidentally. Patients show limitations in exercise capacity, lower oxygen saturation levels:[6]
- A third of patients complain of exertional breathlessness
- Dyspnoea at rest with co-morbidities such as cardiopulmonary conditions
- Bilateral weakness: dyspnoea at mild exertion to dyspnoea at rest:[6]
- Further compromise→ orthopnoea
- Progressive hypoventilation → hypercapnia and right heart failure. Worse during sleep.
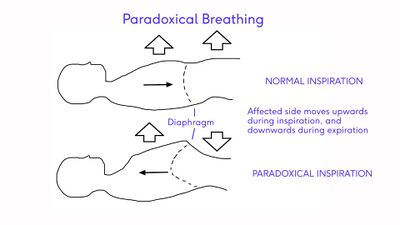
Paradoxical Breathing[edit | edit source]
Paralysis of the diaphragm results in a "paradoxical movement". The affected side moves up during inspiration and down during expiration.[11]
- Unilateral diaphragmatic paralysis is frequently asymptomatic and is often found incidentally on x-ray.[11]
- Bilateral paralysis can result in poor exercise tolerance, orthopnoea and fatigue. There will also be a restrictive deficit on lung function tests.[11]
References[edit | edit source]
- ↑ Fayssoil A, Behin A, Ogna A, Mompoint D, Amthor H, Clair B, Laforet P, Mansart A, Prigent H, Orlikowski D, Stojkovic T, Vinit S, Carlier R, Eymard B, Lofaso F, Annane D. Diaphragm: Pathophysiology and Ultrasound Imaging in Neuromuscular Disorders. J Neuromuscul Dis. 2018;5(1):1-10
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 Bains KN, Kashyap S, Lappin SL. Anatomy, Thorax, Diaphragm. StatPearls [Internet]. 2020 Aug 15.
- ↑ Kurian J. Chest Wall and Diaphragm. InPediatric Body MRI 2020 (pp. 159-192). Springer, Cham.
- ↑ Bordoni B, Purgol S, Bizzarri A, Modica M, Morabito B. The influence of breathing on the central nervous system. Cureus. 2018 Jun;10(6).
- ↑ Oliver KA, Ashurst JV. Anatomy, Thorax, Phrenic Nerves. InStatPearls [Internet] 2020 Jul 27. StatPearls Publishing.
- ↑ 6.0 6.1 6.2 6.3 6.4 Kokatnur L, Vashisht R, Rudrappa M. Diaphragm Disorders. [Updated 2021 Aug 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470172/
- ↑ 7.0 7.1 7.2 Patel PR, Bechmann S. Elevated Hemidiaphragm. [Updated 2021 Aug 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559255/
- ↑ Nair J, Streeter KA, Turner SM, Sunshine MD, Bolser DC, Fox EJ, Davenport PW, Fuller DD. Anatomy and physiology of phrenic afferent neurons. Journal of neurophysiology. 2017 Dec 1;118(6):2975-90.
- ↑ 9.0 9.1 9.2 Pandya R. Diaphragm Anatomy and Differential Diagnosis Course. Physioplus, 2021.
- ↑ Columbia Surgery Diaphragm Eventration Available:https://columbiasurgery.org/conditions-and-treatments/diaphragm-eventration (accessed 9.5.2022)
- ↑ 11.0 11.1 11.2 11.3 TeachMe Anatomy. The diaphragm. Available from: https://teachmeanatomy.info/thorax/muscles/diaphragm/ (accessed 30 November 2021).