Diaphragm Anatomy and Differential Diagnosis: Difference between revisions
Carin Hunter (talk | contribs) No edit summary |
No edit summary |
||
| Line 3: | Line 3: | ||
== Anatomy of the Diaphragm == | == Anatomy of the Diaphragm == | ||
* | The diaphragm is the main respiratory muscle.<ref>Fayssoil A, Behin A, Ogna A, Mompoint D, Amthor H, Clair B, Laforet P, Mansart A, Prigent H, Orlikowski D, Stojkovic T, Vinit S, Carlier R, Eymard B, Lofaso F, Annane D. [https://content.iospress.com/articles/journal-of-neuromuscular-diseases/jnd170276 Diaphragm: Pathophysiology and Ultrasound Imaging in Neuromuscular Disorders.] J Neuromuscul Dis. 2018;5(1):1-10</ref> | ||
* Forms the floor of thorax and roof of abdomen<ref>Kurian J. [https://link.springer.com/chapter/10.1007/978-3-030-31989-2_6 Chest Wall and Diaphragm]. InPediatric Body MRI 2020 (pp. 159-192). Springer, Cham.</ref> | * It is a dome-shaped, "fibromuscular sheet" that separates the thorax from the abdomen<ref name=":0">Bains KN, Kashyap S, Lappin SL. [https://www.ncbi.nlm.nih.gov/books/NBK519558/ Anatomy, Thorax, Diaphragm.] StatPearls [Internet]. 2020 Aug 15.</ref> | ||
* Left side lower than the right due to presence of the liver on the right | * Forms the floor of thorax and roof of abdomen<ref name=":0" /><ref>Kurian J. [https://link.springer.com/chapter/10.1007/978-3-030-31989-2_6 Chest Wall and Diaphragm]. InPediatric Body MRI 2020 (pp. 159-192). Springer, Cham.</ref> | ||
* The left side may also be partially inferiorly | * Left side is lower than the right due to presence of the liver on the right<ref name=":0" /> | ||
* The left side may also be located partially inferiorly due to the "push" by the heart<ref name=":0" /><ref>Bordoni B, Purgol S, Bizzarri A, Modica M, Morabito B. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6070065/ The influence of breathing on the central nervous system.] Cureus. 2018 Jun;10(6).</ref><ref>Oliver KA, Ashurst JV. [https://pubmed.ncbi.nlm.nih.gov/30020697/ Anatomy, Thorax, Phrenic Nerves.] InStatPearls [Internet] 2020 Jul 27. StatPearls Publishing.</ref> | |||
== Major Openings in the Diaphragm == | == Major Openings in the Diaphragm == | ||
[[File:Henry Vandyke Carter, Public domain, via Wikimedia Commons.png|thumb|Diaphragm Anatomy]] | [[File:Henry Vandyke Carter, Public domain, via Wikimedia Commons.png|thumb|Diaphragm Anatomy]] | ||
# '''Caval hiatus:''' at the level of the T8 vertebra in the central tendon. | # '''Caval hiatus:''' at the level of the T8 vertebra in the central tendon. Allows passage of the inferior vena cava and some right phrenic nerve branches.<ref name=":0" /> | ||
# '''The oesophageal hiatus:''' at the level of the T10. It allows | # '''The oesophageal hiatus:''' at the level of the T10. It allows the oesophagus, the right and left vagus trunks, the oesophageal branches of the left gastric vessels, and the lymph vessels to pass through.<ref name=":0" /> | ||
# '''The aortic hiatus:''' anterior to the body | # '''The aortic hiatus:''' anterior to the T12 vertebral body between the crura. Allows the aorta, thoracic duct, and azygos vein to pass through.<ref name=":0" /> | ||
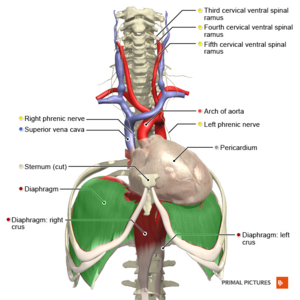
== Nerve Supply == | == Nerve Supply == | ||
[[File:Cervical plexus phrenic nerve Primal.png|thumb|Cervical plexus phrenic nerve]] | [[File:Cervical plexus phrenic nerve Primal.png|thumb|Cervical plexus phrenic nerve]] | ||
The diaphragm is supplied by the [[Phrenic Nerve]]: C3, C4, C5 and sometimes C6 | The diaphragm is supplied by the [[Phrenic Nerve]]:<ref name=":0" /> C3, C4, C5 and sometimes C6 | ||
* '''Motor nerve supply:''' | * '''Motor nerve supply:'''<ref name=":1">Patel PR, Bechmann S. Elevated Hemidiaphragm. 2021 Aug 9. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan–. PMID: 32644681.</ref> | ||
# Left hemidiaphragm with left phrenic nerve | # Left hemidiaphragm with left phrenic nerve | ||
| Line 24: | Line 25: | ||
* '''Sensory nerve supply:''' | * '''Sensory nerve supply:''' | ||
*# The phrenic nerve innervates the parietal pleura and peritoneum | *# The phrenic nerve innervates the parietal pleura and the peritoneum which covers the diaphragm's central surfaces. The periphery of the diaphragm is innervated by the bottom six intercostal nerves.<ref name=":0" /> | ||
*# The phrenic nerve is made up of large | *# The phrenic nerve is made up of large-diameter myelinated, small-diameter myelinated, and unmyelinated fibres. The large diameter fibres fire when the diaphragm contracts whilst the small diameter fibers fire throughout the respiration.<ref>Nair J, Streeter KA, Turner SM, Sunshine MD, Bolser DC, Fox EJ, Davenport PW, Fuller DD. [https://journals.physiology.org/doi/full/10.1152/jn.00484.2017 Anatomy and physiology of phrenic afferent neurons.] Journal of neurophysiology. 2017 Dec 1;118(6):2975-90.</ref> | ||
*#* Activation of the phrenic nerve modulates the sympathetic motor outflow. | *#* Activation of the phrenic nerve modulates the sympathetic motor outflow.<ref name=":0" /> | ||
*#* Phrenic afferents also | *#* Phrenic afferents are also involved in the somatosensation of the diaphragm and they make individuals aware of their breathing while they are awake.<ref name=":0" /> | ||
== Vascular Supply == | == Vascular Supply == | ||
'''Arterial supply:''' | '''Arterial supply:''' | ||
* Inferior phrenic | * Inferior phrenic artery from abdominal [[aorta]] | ||
* | * Superior phrenic artery | ||
* Pericardiophrenic, musculophrenic arteries | |||
'''Venous supply:''' | '''Venous supply:''' | ||
* Inferior phrenic vein | * Inferior phrenic vein | ||
| Line 39: | Line 41: | ||
=== 1. Vertebrae === | === 1. Vertebrae === | ||
* | * Medial lumbocostal arch<ref name=":0" /> | ||
* | ** A tendinous arch in the fascia which covers [[Psoas Major]] | ||
** Medially, it attaches to the side of the L1 vertebral body | |||
** Laterally, it attaches at the front of the L1 transverse process | |||
* Lateral lumbocostal arch<ref name=":0" /> | |||
** A tendinous arch in the fascia which covers the upper portion of [[Quadratus Lumborum]] | |||
** Medially, it attaches to the front of the L1 transverse process | |||
** Laterally, it attaches to the lower border of rib 12 | |||
=== 2. Muscles === | === 2. Muscles === | ||
* | * Quadratus Lumborum (QL) attaches to the inferior portion of the 12th rib. A part of the diaphragm attaches to this rib's superior portion. The fascia is continuous between these attachments.<ref name=":2">Pandya R. Diaphragm Anatomy and Differential Diagnosis Course. Physioplus, 2021.</ref> | ||
* The Psoas muscle | * The Psoas muscle is in a similar area as the QL. It blends with the fascia at the proximal end of the posterior portion of the diaphragm.<ref name=":2" /> | ||
== Aetiology | == Aetiology of an Elevated Diaphragm == | ||
An elevated hemidiaphragm may | An elevated hemidiaphragm may be due to both direct and indirect causes. | ||
The causes can be grouped into | The causes can be grouped into three categories based on the location of the cause, including:<ref name=":1" /><ref name=":2" /> | ||
# Above the diaphragm | # Above the diaphragm | ||
| Line 67: | Line 75: | ||
=== Differential Diagnosis for Elevated Diaphragm === | === Differential Diagnosis for Elevated Diaphragm === | ||
Other situations which may mimic an elevated hemidiaphragm include: | Other situations which may mimic an elevated hemidiaphragm include:<ref name=":1" /> | ||
* [https://radiopaedia.org/articles/subpulmonic-effusion?lang=us Subpulmonic effusion] | * [https://radiopaedia.org/articles/subpulmonic-effusion?lang=us Subpulmonic effusion] | ||
| Line 75: | Line 83: | ||
== Aetiology for Paralysis of the Diaphragm == | == Aetiology for Paralysis of the Diaphragm == | ||
Diaphragmatic paralysis is | Diaphragmatic paralysis occurs when the nerve supply is interrupted. This interruption might occur in the phrenic nerve itself, at the cervical spinal cord, or in the brainstem. However, it is most commonly caused by a phrenic nerve lesion:<ref name=":3">Kokatnur L, Vashisht R, Rudrappa M. Diaphragm Disorders. [Updated 2021 Aug 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470172/</ref><ref name=":4">TeachMe Anatomy. The diaphragm. Available from: https://teachmeanatomy.info/thorax/muscles/diaphragm/ (accessed 30 November 2021).</ref> | ||
*'''Mechanical trauma:''' such as nerve damage / ligation during surgery | |||
*'''Compression:''' due to a chest cavity tumour | |||
*'''Myopathies:''' including myasthenia gravis | |||
*'''Neuropathic:''' including conditions such as diabetic neuropathy, inclusion body myositis, [[dermatomyositis]], [[MS Multiple Sclerosis|multiple sclerosis]], anterior horn cell disease, chronic demyelinating disease, and neuralgic myopathy | |||
*''' Inflammation:''' a number of systemic diseases can cause inflammation in the phrenic nerve / diaphragm, which results in diaphragmatic palsy. Examples include: | |||
** Viral infections (e.g. [[HIV/AIDS|HIV]], West Nile virus and poliomyelitis virus) | |||
** Bacterial infections (e.g. [[Lyme Disease|Lyme disease]]) | |||
** Non-infectious causes (e.g. [[sarcoidosis]] and amyloidosis) | |||
*''' Idiopathic:''' around 20 percent of cases have no obvious cause | |||
=== Differential Diagnosis for Paralysis of the Diaphragm === | === Differential Diagnosis for Paralysis of the Diaphragm === | ||
| Line 93: | Line 104: | ||
* [[Myasthenia Gravis|Myasthenia gravis]] | * [[Myasthenia Gravis|Myasthenia gravis]] | ||
* Peripheral neuropathies | * Peripheral neuropathies | ||
* Pleural adhesions | * Pleural adhesions<ref name=":3" /> | ||
== Symptoms of Diaphragmatic Weakness == | == Symptoms of Diaphragmatic Weakness == | ||
# '''Unilateral weakness:''' Often asymptomatic and detected incidentally. Patients show limitations in exercise capacity, lower oxygen ( O<sup>2</sup>) saturation levels | # '''Unilateral weakness:''' Often asymptomatic and detected incidentally. Patients show limitations in exercise capacity, lower oxygen ( O<sup>2</sup>) saturation levels:<ref name=":3" /> | ||
#* | #* A third of patients complain of exertional breathlessness | ||
#* Dyspnoea at rest with co-morbidities such as cardiopulmonary conditions | #* Dyspnoea at rest with co-morbidities such as cardiopulmonary conditions | ||
# '''Bilateral weakness:''' dyspnoea at mild exertion to dyspnoea at rest | # '''Bilateral weakness:''' dyspnoea at mild exertion to dyspnoea at rest:<ref name=":3" /> | ||
#* Further compromise→ orthopnoea | #* Further compromise→ orthopnoea | ||
#* Progressive hypoventilation → hypercapnia and right heart failure. Worse during sleep. | #* Progressive hypoventilation → hypercapnia and right heart failure. Worse during sleep. | ||
| Line 105: | Line 116: | ||
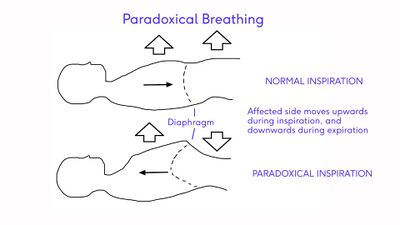
== Paradoxical Breathing == | == Paradoxical Breathing == | ||
[[File:Paradoxical Breathing Image - recreated with labels.jpg|thumb|400x400px|Paradoxical Breathing]] | [[File:Paradoxical Breathing Image - recreated with labels.jpg|thumb|400x400px|Paradoxical Breathing]] | ||
Paralysis of the diaphragm | Paralysis of the diaphragm results in a "paradoxical movement". The affected side moves up during inspiration and down during expiration.<ref name=":4" /> | ||
* Unilateral diaphragmatic paralysis is frequently asymptomatic and is often found incidentally on x-ray.<ref name=":4" /> | |||
* Bilateral paralysis can result in poor exercise tolerance, orthopnoea and fatigue. There will also be a restrictive deficit on lung function tests.<ref name=":4" /> | |||
{{#ev:youtube|8TnrNrrEjuE}} | {{#ev:youtube|8TnrNrrEjuE}} | ||
Revision as of 11:59, 30 November 2021
Top Contributors - Carin Hunter, Jess Bell, Kim Jackson, Wanda van Niekerk, Merinda Rodseth, Lucinda hampton, Ewa Jaraczewska and Tarina van der Stockt
Anatomy of the Diaphragm[edit | edit source]
The diaphragm is the main respiratory muscle.[1]
- It is a dome-shaped, "fibromuscular sheet" that separates the thorax from the abdomen[2]
- Forms the floor of thorax and roof of abdomen[2][3]
- Left side is lower than the right due to presence of the liver on the right[2]
- The left side may also be located partially inferiorly due to the "push" by the heart[2][4][5]
Major Openings in the Diaphragm[edit | edit source]
- Caval hiatus: at the level of the T8 vertebra in the central tendon. Allows passage of the inferior vena cava and some right phrenic nerve branches.[2]
- The oesophageal hiatus: at the level of the T10. It allows the oesophagus, the right and left vagus trunks, the oesophageal branches of the left gastric vessels, and the lymph vessels to pass through.[2]
- The aortic hiatus: anterior to the T12 vertebral body between the crura. Allows the aorta, thoracic duct, and azygos vein to pass through.[2]
Nerve Supply[edit | edit source]
The diaphragm is supplied by the Phrenic Nerve:[2] C3, C4, C5 and sometimes C6
- Motor nerve supply:[6]
- Left hemidiaphragm with left phrenic nerve
- Right hemidiaphragm with right phrenic nerve
- Sensory nerve supply:
- The phrenic nerve innervates the parietal pleura and the peritoneum which covers the diaphragm's central surfaces. The periphery of the diaphragm is innervated by the bottom six intercostal nerves.[2]
- The phrenic nerve is made up of large-diameter myelinated, small-diameter myelinated, and unmyelinated fibres. The large diameter fibres fire when the diaphragm contracts whilst the small diameter fibers fire throughout the respiration.[7]
Vascular Supply[edit | edit source]
Arterial supply:
- Inferior phrenic artery from abdominal aorta
- Superior phrenic artery
- Pericardiophrenic, musculophrenic arteries
Venous supply:
- Inferior phrenic vein
Fascial Attachments[edit | edit source]
1. Vertebrae[edit | edit source]
- Medial lumbocostal arch[2]
- A tendinous arch in the fascia which covers Psoas Major
- Medially, it attaches to the side of the L1 vertebral body
- Laterally, it attaches at the front of the L1 transverse process
- Lateral lumbocostal arch[2]
- A tendinous arch in the fascia which covers the upper portion of Quadratus Lumborum
- Medially, it attaches to the front of the L1 transverse process
- Laterally, it attaches to the lower border of rib 12
2. Muscles[edit | edit source]
- Quadratus Lumborum (QL) attaches to the inferior portion of the 12th rib. A part of the diaphragm attaches to this rib's superior portion. The fascia is continuous between these attachments.[8]
- The Psoas muscle is in a similar area as the QL. It blends with the fascia at the proximal end of the posterior portion of the diaphragm.[8]
Aetiology of an Elevated Diaphragm[edit | edit source]
An elevated hemidiaphragm may be due to both direct and indirect causes.
The causes can be grouped into three categories based on the location of the cause, including:[6][8]
- Above the diaphragm
- Decreased lung volume
- Atelectasis/collapse
- Prior lobectomy or pneumonectomy
- Pulmonary hypoplasia
- At the level of the diaphragm
- Phrenic nerve palsy
- Diaphragmatic eventration
- Contralateral stroke: usually middle cerebral artery (MCA) distribution
- Below the diaphragm
- Abdominal tumour, e.g. liver metastases or primary malignancy
- Subphrenic abscess
- Distended stomach or colon, including Chilaiditi sign/syndrome
Differential Diagnosis for Elevated Diaphragm[edit | edit source]
Other situations which may mimic an elevated hemidiaphragm include:[6]
- Subpulmonic effusion
- Diaphragmatic hernia
- Diaphragmatic rupture
- Tumour of the pleura or diaphragm
Aetiology for Paralysis of the Diaphragm[edit | edit source]
Diaphragmatic paralysis occurs when the nerve supply is interrupted. This interruption might occur in the phrenic nerve itself, at the cervical spinal cord, or in the brainstem. However, it is most commonly caused by a phrenic nerve lesion:[9][10]
- Mechanical trauma: such as nerve damage / ligation during surgery
- Compression: due to a chest cavity tumour
- Myopathies: including myasthenia gravis
- Neuropathic: including conditions such as diabetic neuropathy, inclusion body myositis, dermatomyositis, multiple sclerosis, anterior horn cell disease, chronic demyelinating disease, and neuralgic myopathy
- Inflammation: a number of systemic diseases can cause inflammation in the phrenic nerve / diaphragm, which results in diaphragmatic palsy. Examples include:
- Viral infections (e.g. HIV, West Nile virus and poliomyelitis virus)
- Bacterial infections (e.g. Lyme disease)
- Non-infectious causes (e.g. sarcoidosis and amyloidosis)
- Idiopathic: around 20 percent of cases have no obvious cause
Differential Diagnosis for Paralysis of the Diaphragm[edit | edit source]
- Alveolar hypoventilation
- Anterior horn cell or neuromuscular junction disease
- Cerebral haemorrhage
- Cervical fracture
- Decreased pulmonary compliance
- Guillain-Barre syndrome
- Myasthenia gravis
- Peripheral neuropathies
- Pleural adhesions[9]
Symptoms of Diaphragmatic Weakness[edit | edit source]
- Unilateral weakness: Often asymptomatic and detected incidentally. Patients show limitations in exercise capacity, lower oxygen ( O2) saturation levels:[9]
- A third of patients complain of exertional breathlessness
- Dyspnoea at rest with co-morbidities such as cardiopulmonary conditions
- Bilateral weakness: dyspnoea at mild exertion to dyspnoea at rest:[9]
- Further compromise→ orthopnoea
- Progressive hypoventilation → hypercapnia and right heart failure. Worse during sleep.
Paradoxical Breathing[edit | edit source]
Paralysis of the diaphragm results in a "paradoxical movement". The affected side moves up during inspiration and down during expiration.[10]
- Unilateral diaphragmatic paralysis is frequently asymptomatic and is often found incidentally on x-ray.[10]
- Bilateral paralysis can result in poor exercise tolerance, orthopnoea and fatigue. There will also be a restrictive deficit on lung function tests.[10]
References[edit | edit source]
- ↑ Fayssoil A, Behin A, Ogna A, Mompoint D, Amthor H, Clair B, Laforet P, Mansart A, Prigent H, Orlikowski D, Stojkovic T, Vinit S, Carlier R, Eymard B, Lofaso F, Annane D. Diaphragm: Pathophysiology and Ultrasound Imaging in Neuromuscular Disorders. J Neuromuscul Dis. 2018;5(1):1-10
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 Bains KN, Kashyap S, Lappin SL. Anatomy, Thorax, Diaphragm. StatPearls [Internet]. 2020 Aug 15.
- ↑ Kurian J. Chest Wall and Diaphragm. InPediatric Body MRI 2020 (pp. 159-192). Springer, Cham.
- ↑ Bordoni B, Purgol S, Bizzarri A, Modica M, Morabito B. The influence of breathing on the central nervous system. Cureus. 2018 Jun;10(6).
- ↑ Oliver KA, Ashurst JV. Anatomy, Thorax, Phrenic Nerves. InStatPearls [Internet] 2020 Jul 27. StatPearls Publishing.
- ↑ 6.0 6.1 6.2 Patel PR, Bechmann S. Elevated Hemidiaphragm. 2021 Aug 9. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan–. PMID: 32644681.
- ↑ Nair J, Streeter KA, Turner SM, Sunshine MD, Bolser DC, Fox EJ, Davenport PW, Fuller DD. Anatomy and physiology of phrenic afferent neurons. Journal of neurophysiology. 2017 Dec 1;118(6):2975-90.
- ↑ 8.0 8.1 8.2 Pandya R. Diaphragm Anatomy and Differential Diagnosis Course. Physioplus, 2021.
- ↑ 9.0 9.1 9.2 9.3 Kokatnur L, Vashisht R, Rudrappa M. Diaphragm Disorders. [Updated 2021 Aug 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470172/
- ↑ 10.0 10.1 10.2 10.3 TeachMe Anatomy. The diaphragm. Available from: https://teachmeanatomy.info/thorax/muscles/diaphragm/ (accessed 30 November 2021).