Dermatomes: Difference between revisions
Anas Mohamed (talk | contribs) (Undo revision 231840 by Anas Mohamed (talk)) |
Anas Mohamed (talk | contribs) No edit summary |
||
| Line 105: | Line 105: | ||
* '''Light touch test''' (light touch sensation) - Dab a piece of cotton wool on an area of skin <ref>Slide share. [https://www.slideshare.net/TafzzSailo/special-test-for-dermatomes-and-myotomes Dermatomes and myotomes]. Available from: https://www.slideshare.net/TafzzSailo/special-test-for-dermatomes-and-myotomes (last accessed 23.4.2019)</ref> | * '''Light touch test''' (light touch sensation) - Dab a piece of cotton wool on an area of skin <ref>Slide share. [https://www.slideshare.net/TafzzSailo/special-test-for-dermatomes-and-myotomes Dermatomes and myotomes]. Available from: https://www.slideshare.net/TafzzSailo/special-test-for-dermatomes-and-myotomes (last accessed 23.4.2019)</ref> | ||
During the review of systems, asking the patient to carefully describe the pattern or distribution of sensory symptoms (e.g., tingling, numbness, diminished, or absent sensation) provides the therapist with preliminary information to help guide the examination and to assist in identifying the dermatome(s) and nerve(s) involved.<ref name=":0">Susan B.O'Sullivan, Thomas J. Schmitz, George D. Fulk. Physical Rehabilitation. 6th edition. F. A. Davis Company. 2014.</ref> | During the review of systems, asking the patient to carefully describe the pattern or distribution of sensory symptoms (e.g., tingling, numbness, diminished, or absent sensation) provides the therapist with preliminary information to help guide the examination and to assist in identifying the dermatome(s) and nerve(s) involved.<ref name=":0">Susan B.O'Sullivan, Thomas J. Schmitz, George D. Fulk. Physical Rehabilitation. 6th edition. F. A. Davis Company. 2014.</ref> | ||
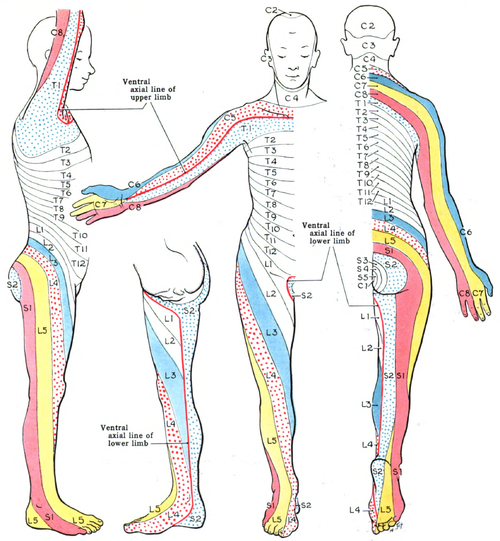
Peripheral nerve injuries generally present sensory impairments that parallel the distribution of the involved nerve and correspond to its pattern of innervation.'''For example,''' if a patient presents with complaints of numbness on the ulnar half of the ring finger, the little finger, and the ulnar side of the hand, the therapist would be alerted to carefully address ulnar nerve (C8 and T1) integrity during the sensory examination. Complaints of sensory disturbances on the palmar surface of the thumb and the palmar and distal dorsal aspects of the index, middle, and the radial half of the ring finger would be indicative of median nerve (C6–8 and T1) involvement.<ref name=":0" />[[File:Dermatomes Grant.png|center|frameless|541x541px]]There exist some discrepancies among published dermatome maps based on the methodologies used to identify skin segment innervation. In a clinical commentary, Downs and Laporte discuss the history of dermatome mapping, including the variations in methodologies employed, and the inconsistencies in the dermatome maps used in education and practice.<ref name=":0" />[[[https://www.jospt.org/doi/citedby/10.2519/jospt.2011.3506 Laporte C. Conflicting dermatome maps: educational and clinical implications. journal of orthopaedic & sports physical therapy. 2011 Jun;41(6):42]<ref>Downs MB, Laporte C. Conflicting dermatome maps: educational and clinical implications. journal of orthopaedic & sports physical therapy. 2011 Jun;41(6):427-34.</ref>[https://www.jospt.org/doi/citedby/10.2519/jospt.2011.3506 7-34.]]]{{#ev:youtube|ETvKVAYxKO0}} | |||
== References == | == References == | ||
Revision as of 12:31, 26 February 2020
Original Editor - Your name will be added here if you created the original content for this page.
Lead Editors
Dermatomes[edit | edit source]
A dermatome is an area of skin that is mainly supplied by a single spinal nerve. There are 8 cervical nerves (note C1 has with no dermatome), 12 thoracic nerves, 5 lumbar nerves and 5 sacral nerves. Each of these spinal nerves relay sensation from a particular region of the skin to the brain.[1]
The nerves from the
- C2 to C4 supply the skin of the neck.
- C5 to T1 nerves supply the arms.
- T2 to L2 nerves supply the chest and abdomen.
- L3 to S1 nerves supply the skin of the legs.
- S1 to S4 nerves go to the groin.
| Nerve Root | Dermatomes |
|---|---|
| Cervical | |
| C2 | Temple, forehead, occiput |
| C3 | Entire neck, posterior cheek, temporal area, prolongation forward under mandible |
| C4 | Shoulder area, clavicular area, upper scapular area |
| C5 | Deltoid area, anterior aspect of entire arm to base of thumb |
| C6 | Anterior arm, radial side of hand to thumb and index finger |
| C7 | Lateral arm and forearm to index, long, and ring fingers |
| C8 | Medial arm and forearm to long, ring, and little fingers |
| Thoracic | |
| T1 | Medial side of forearm to base of little finger |
| T2 | Medial side of upper arm to medial elbow, pectoral and midscapular areas |
| T3-T12 | T3–T6, upper thorax;
T5–T7, costal margin; T8–T12, abdomen and lumbar region |
| Lumbar | |
| L1 | Back, over trochanter and groin |
| L2 | Back, front of thigh to knee |
| L3 | Back, upper buttock, anterior thigh and knee, medial lower leg |
| L4 | Medial buttock, latera thigh, medial leg, dorsum of foot, big toe |
| L5 | Buttock, posterior and lateral thigh, lateral aspect of leg, dorsum of foot, medial half of sole, first, second, and third toes |
| Sacral | |
| S1 | Buttock, thigh, and leg posterior |
| S2 | Same as S1 |
| S3 | Groin, medial thigh to knee |
| S4 | Perineum, genitals, lower sacrum |
Purpose[edit | edit source]
Testing of dermatomes is part of the neurological examination looking for radiculopathy as sensation changes within a specific dermatome may help in determining the pathological disc level.
Technique[edit | edit source]
Dermatome Testing is done ideally with a pin and cotton wool. Ask the patient to close their eyes and give the therapist feedback regarding the various stimuli. Testing should be done on specific dermatomes and should be compared to bilaterally.
- Pinprick test (pain sensation) - Gently touches the skin with the pin ask the patient whether it feels sharp or blunt
- Light touch test (light touch sensation) - Dab a piece of cotton wool on an area of skin [4]
During the review of systems, asking the patient to carefully describe the pattern or distribution of sensory symptoms (e.g., tingling, numbness, diminished, or absent sensation) provides the therapist with preliminary information to help guide the examination and to assist in identifying the dermatome(s) and nerve(s) involved.[5]
Peripheral nerve injuries generally present sensory impairments that parallel the distribution of the involved nerve and correspond to its pattern of innervation.For example, if a patient presents with complaints of numbness on the ulnar half of the ring finger, the little finger, and the ulnar side of the hand, the therapist would be alerted to carefully address ulnar nerve (C8 and T1) integrity during the sensory examination. Complaints of sensory disturbances on the palmar surface of the thumb and the palmar and distal dorsal aspects of the index, middle, and the radial half of the ring finger would be indicative of median nerve (C6–8 and T1) involvement.[5]
There exist some discrepancies among published dermatome maps based on the methodologies used to identify skin segment innervation. In a clinical commentary, Downs and Laporte discuss the history of dermatome mapping, including the variations in methodologies employed, and the inconsistencies in the dermatome maps used in education and practice.[5][[Laporte C. Conflicting dermatome maps: educational and clinical implications. journal of orthopaedic & sports physical therapy. 2011 Jun;41(6):42[6]7-34.]]
References[edit | edit source]
- ↑ Wikipedia Dermatome. Available from: https://en.wikipedia.org/wiki/Dermatome_(anatomy) (last accessed 23.4.2019)
- ↑ M Roehrs. Dermatomes. Available from: https://www.youtube.com/watch?v=CYZBH6NX8wg&feature=youtu.be (last accessed 23.4.2019)
- ↑ David J. Magee. Orthopedic Physical Assessment. 6th edition. Elsevier. 2014.
- ↑ Slide share. Dermatomes and myotomes. Available from: https://www.slideshare.net/TafzzSailo/special-test-for-dermatomes-and-myotomes (last accessed 23.4.2019)
- ↑ 5.0 5.1 5.2 Susan B.O'Sullivan, Thomas J. Schmitz, George D. Fulk. Physical Rehabilitation. 6th edition. F. A. Davis Company. 2014.
- ↑ Downs MB, Laporte C. Conflicting dermatome maps: educational and clinical implications. journal of orthopaedic & sports physical therapy. 2011 Jun;41(6):427-34.