De Quervain's Tenosynovitis: Difference between revisions
No edit summary |
(rewrote epidemiology section a bit) |
||
| Line 38: | Line 38: | ||
#*Artery: A. interossea posterior | #*Artery: A. interossea posterior | ||
== Epidemiology == | == Epidemiology == | ||
* | * Estimated prevalence is 0.5% in men and 1.3% in women. Peak prevalence is usually among individuals between the ages of 40 -50 years<ref name=":3" /> | ||
* | * More commonly found in people with a history of [[Medial Epicondyle Tendinopathy|medial]] or [[Lateral Epicondylitis|lateral epicondylitis]] | ||
* | * New mothers or child care providers often experience bilateral symptoms, but these symptoms usually subside once the child is lifted less often.<ref name=":0">Satteson E, Tannan SC. [https://www.ncbi.nlm.nih.gov/books/NBK442005/ De Quervain Tenosynovitis.] StatPearls [Internet]. 2021 Aug 8.</ref> | ||
* In industrial settings, studies have shown a point prevalence of 8% when wrist pain and a positive [http://www.physio-pedia.com/Finkelstein_Test Finkelstein’s test] is present.<ref name="Ashurst" /> | * In industrial settings, studies have shown a point prevalence of 8% when wrist pain and a positive [http://www.physio-pedia.com/Finkelstein_Test Finkelstein’s test] is present.<ref name="Ashurst" /> | ||
Revision as of 11:30, 9 December 2021
Original Editor - Elizabeth Dallas, Boris Alexandra, Robin Leigh Tacchetti
Top Contributors - Wanda van Niekerk, John Winkelhaus, David Cameron, John Fite, Robin Leigh Tacchetti, Robin Tacchetti, Laura Ritchie, Admin, Boris Alexandra, Kim Jackson, Aurelie Canas Perez, Julie Schuermans, Elizabeth Dallas, Lucinda hampton, Redisha Jakibanjar, Corin Arundale, Rachael Lowe, Tarina van der Stockt, Jess Bell, Jorge Rodríguez Palomino, WikiSysop, Claire Knott, Anas Mohamed, Chrysolite Jyothi Kommu, Evan Thomas, Naomi O'Reilly, Arturo Quiroz Marnef, 127.0.0.1 and Kai A. Sigel - Corin Arundale, David Cameron, John Fite, Bryan Purkey, John Winkelhaus
Definition/Description[edit | edit source]
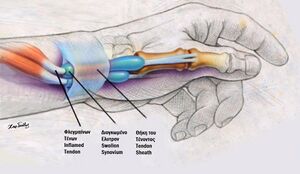
De Quervain's Tenosynovitis is a painful, inflammatory condition caused by tendons on the side of the wrist at the base of the thumb. Pain, which is the main complaint, gets worse with abduction of the thumb, a grasping action of the hand, and an ulnar deviation of the wrist. Thickening and swelling can also be present. [1] [2][3]
Aetiology[edit | edit source]
- The most common cause is chronic overuse.
- Activities such as golfing, playing the piano, fly fishing, carpentry, or activities by office workers and musicians can lead to chronic overuse injuries.
- The classic patient population is mothers of newborns who are repeatedly lifting their baby with their thumbs radially abducted and wrists going from ulnar to radial deviation.
- Repetitive gripping, grasping or wringing of objects can cause inflammation of the tendons and tendon sheaths which narrows the first dorsal compartment limiting motion of the tendons. If left untreated, the inflammation and progressive narrowing (stenosis) can lead to scarring that further limits thumb motion. [2][3]
- De Quervain's has been "attributed to myxoid degeneration (the process in which the connective tissues are replaced by a gelatinous substance) with fibrous tissue deposits and increased vascularity rather than acute inflammation of the synovial lining."[4] It is for this reason that is thought to be a tendinosis rather than a tendonitis.[5] This deposition of the fibrous tissues causes thickening of the tendon sheath, and this can entrap the abductor pollicis longus and extensor pollicis brevis tendons and cause pain.
Relevant Clinical Anatomy[edit | edit source]
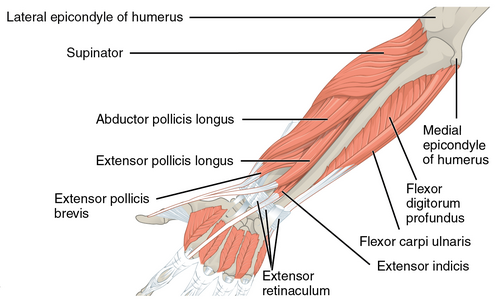
De Quervain's syndrome affects the extensor pollicis brevis (EPB) tendon and the abductor pollicis longus (APL) tendon. These muscles are located on the dorsal side of the forearm and go to the lateral side of the thumb through a fibrous-osseous tunnel made of the processus styloideus radii and the extensor retinaculum. [6] The tendon sheaths around the abductor pollicis longus and extensor pollicis brevis pass through the fibro-osseous tunnel located along the radial styloid at the distal wrist.
- Extensor pollicis brevis (EPB)
- Origin: ½ dorsal side of the radius, the membrana interossea
- Insertion: base of the proximal phalanx of the thumb
- Function:
- Wrist joint: radial abduction
- Thumb: extension
- Innervations: posterior interosseus branch of N. radialis
- Artery: A. interossea posterior
- Abductor pollicis longus (APL)
- Origin: dorsal side of the radius and the ulna, the membrana interossea
- Insertion: base of ossis metacarpi
- Function:
- Wrist joint: radial abduction
- Thumb: abduction
- Innervations: posterior interosseus branch of N. radialis
- Artery: A. interossea posterior
Epidemiology[edit | edit source]
- Estimated prevalence is 0.5% in men and 1.3% in women. Peak prevalence is usually among individuals between the ages of 40 -50 years[7]
- More commonly found in people with a history of medial or lateral epicondylitis
- New mothers or child care providers often experience bilateral symptoms, but these symptoms usually subside once the child is lifted less often.[4]
- In industrial settings, studies have shown a point prevalence of 8% when wrist pain and a positive Finkelstein’s test is present.[2]
Clinical Presentation[edit | edit source]
Examination[edit | edit source]
The evaluation of a patient with signs and symptoms of De Quervain’s Tenosynovitis begins with a thorough history followed by a physical examination.
History[edit | edit source]
- Overuse injury vs acute trauma
- Prior history of symptoms
- Repetitive movements of the upper extremity with work or activities of daily living (ADL)
- Hand dominance
- Pregnant or currently in the post-partum stage
- Pain:
- The primary complaint is radial sided wrist pain (base of thumb and dorsolateral aspect of the wrist near the radial styloid process) that radiates up the forearm with grasping or extension of the thumb
- Described as a “constant aching, burning, pulling sensation."[8]
- Aggravated by repetitive lifting, gripping, or twisting motions of the hand (such as opening a jar lid).[8]
Physical Examination[edit | edit source]
- On palpation, some key, significant findings will be tenderness over the base of the thumb and/or first dorsal compartment extensor tendons on the thumb side of the wrist, particularly over the radial styloid process[2]
- Swelling in the anatomical snuffbox
- Decreased carpometacarpal (CMC) abduction range of motion (ROM) of the first digit
- Palpable thickening of the extensor sheaths of the first dorsal compartment and crepitus of the tendons moving from the extensor sheath [9]
- Other possible findings include:
- Weakness and paraesthesia in the hand[3]
- A provocative Finkelstein test
- During this test, the thumb is flexed and held inside a fist. The patient actively deviates the wrist towards the ulnar side. This causes sharp pain along the radial wrist at the first dorsal compartment.[4]
Video provided by Clinically Relevant
Non-Surgical Treatment[edit | edit source]
The aim of non-surgical management is to reduce pain and swelling. Interventions can include:
- Patient education regarding avoiding repetitive or aggravating movements[5]
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Ice/heat packs
- Physical therapy[10]
- Thumb splinting
- Literature supports the use of a forearm brace including the thumb to reduce ulnar deviation and thumb movement.[5]
- Clinicians do not agree on the frequency and duration of splint use; some think it should be worn continually for four to six weeks; others recommend wearing it only as needed for pain.[11]
- Weiss and colleagues[12] found that a 19% improvement was observed when splints were used, but when splint use was combined with NSAIDs, the improvement was 57%. Cavaleri et al.[7] reported that combined orthosis/corticosteroid injection approaches are more effective than either intervention alone in the treatment of de Quervain's disease.
- Ultrasound is thought to improve treatment outcomes and can be used as a diagnostic tool in the management of De Quervain’s disease.[13]
- McDermott et al.[14] found that ultrasound-guided injections were beneficial for De Quervain's tenosynovitis. There results were slightly better than was previously reported in the literature and they reported no adverse reactions.[14]
- Kume et al.[15] found that ultrasound-guided injections which target the Extensor Pollicis Brevis with septation was more effective than manual injection.
- Corticosteroid injection has been reported to provide near-complete relief with one or two injections. The injection is performed into the tendon sheath about 1 cm proximal to the radial styloid where tendons can be palpated tendons.
- If symptoms do not improve or recur after two corticosteroid injections, operative management may be considered. Surgery is usually done in an outpatient setting and the anaesthetic may be local, regional or general.[4]
- Patients with moderate to severe symptoms usually require cortisone injections in combination with splinting.[5]
** For those individuals with persistent symptoms, splinting, systemic anti-inflammatories, and corticosteroid injection is the most frequently utilised non-surgical treatment option.[7][13] [16]
Surgical Treatment[edit | edit source]
- Surgery is rare and is usually selected in cases where non-surgical treatment has failed and the patient experiences persistent inflammation affecting his or her function. The goal of surgery is to open the dorsal compartment covering to make more room for the irritated tendons. The opening allows pressure relief of the tendons, to ultimately restore free tendon gliding.[17]
- Post-operative care is usually limited. A simple dressing or wrap is frequently utilized with no need for complex wound care. Patients are advised to begin early use for activities of daily living and other light activities. Once sutures are removed, usually by two weeks, patients are typically released to resume normal activities. Patients may continue to experience mild swelling and tenderness at the surgical site for a few months.[4]
Physical Therapy Management[edit | edit source]
- Ice/Heat Packs
- Heat can help relax and loosen tight musculature, and ice can be used to help relieve inflammation of the extensor sheath.
- Massage
- Deep tissue massage at the thenar eminence can help relax tight musculature that causes pain. The Graston Technique of manual soft tissue mobilisation along with eccentric exercise is also helpful. This technique includes breaking down fascia restriction, stretching connective tissue, and promoting a better healing environment.[18]
- Strengthening
- The progression of exercise therapy is as follows:[5]
- Isometric
- Eccentric
- Concentric inner range
- Theraputy
- Radial nerve glides
- The progression of exercise therapy is as follows:[5]
Patients can start with strengthening exercises once their pain has settled to a manageable level. The strengthening programme should be graded and very gradual. Only progress patients through the strengthening programme if they are able to tolerate their current strength programme for at least 1 week. It is important to progress slowly and that patients strengthen in a pain-free range of motion, to avoid aggravation of symptoms.[5] Below are some examples of strengthening exercises.
- Mobilisation
- Mobilisation with movement has shown effectiveness in decreasing the pain, improving range of motion, and improving the function of a patient with De-Quervain's tenosynovitis. The therapist provided a manual radial glide of the proximal row of carpals, then asked the patient to move her thumb into radial abduction-adduction.[29] Mobilisation with movement performed for 3 sets of 10 repetitions and followed by eccentric hammer curl exercise with theraband and high voltage electrical stimulation was shown to be effective at 6 months follow-up.[30] Savva et al.[31] investigated the analgesic effect of joint mobilisation in tendinopathy and concluded that the literature on joint mobilisations in tendinopathies such as De Quervain's remains limited since the effect of these techniques have been sparsely reported in a few retrospective case-series and case studies.
- Taping
- Taping can also be used to decrease pain and improve function.[33]
- Ultrasound
- Therapeutic ultrasound has also better outcomes in pain reduction and healing. [18]
Red Flags[edit | edit source]
Red flags to look out for in patients with De Quervain's can include:[5]
- Signs of infection such as unresolved redness or swelling
- High levels of pain (≥ 7/10) after 4 weeks of conservative treatment
- High demand workplace or someone who is forced to continue with aggravating activities
Conclusion[edit | edit source]
Effective management of DeQuervain’s tenosynovitis will involve a highly individualised, impairment driven approach for the patient in question. Early splinting during the acute phase will prevent aggravation of the tissues, and allow the patient to perform activities essential to self-care and employment. The patient will need to be educated on the tissue healing timetables, as well as why it is important to avoid activities that are aggravating to their symptoms. The progression of exercise therapy is from isometric to eccentric to concentric inner range. Patients should be pain-free before progressing to the next level of strengthening.
References[edit | edit source]
- ↑ Pagonis T, Ditsios K, Toli P, Givissis P, Christodoulou A. Improved corticosteroid treatment of recalcitrant de Quervain tenosynovitis with a novel 4-point injection technique. The American journal of sports medicine. 2011 Feb;39(2):398-403.
- ↑ 2.0 2.1 2.2 2.3 Ashurst JV, Turco DA, Lieb BE. Tenosynovitis caused by texting: an emerging disease. Journal of Osteopathic Medicine. 2010 May 1;110(5):294-6.
- ↑ 3.0 3.1 3.2 González-iGlesias J, Huijbregts P, Fernández-de-Las-Peñas C, Cleland JA. Differential diagnosis and physical therapy management of a patient with radial wrist pain of 6 months' duration: a case report. journal of orthopaedic & sports physical therapy. 2010 Jun;40(6):361-8.
- ↑ 4.0 4.1 4.2 4.3 4.4 Satteson E, Tannan SC. De Quervain Tenosynovitis. StatPearls [Internet]. 2021 Aug 8.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 Kate Thorn. De Quervain's Tenosynovitis. Physioplus Course. 2021
- ↑ Katechia D, Gujral S. De Quervain's tenosynovitis. InnovAiT. 2017 Sep;10(9):505-9.
- ↑ 7.0 7.1 7.2 Cavaleri R, Schabrun SM, Te M, Chipchase LS. Hand therapy versus corticosteroid injections in the treatment of de Quervain's disease: A systematic review and meta-analysis. Journal of Hand Therapy. 2016 Jan 1;29(1):3-11.
- ↑ 8.0 8.1 Walker MJ. Manual physical therapy examination and intervention of a patient with radial wrist pain: a case report. Journal of orthopaedic & sports physical therapy. 2004 Dec;34(12):761-9.
- ↑ Anderson M, Tichenor CJ. A patient with de Quervain's tenosynovitis: a case report using an Australian approach to manual therapy. Physical therapy. 1994 Apr 1;74(4):314-26.
- ↑ Földvári-Nagy L, Takács J, Hetthéssy JR, Mayer ÁA, Szakács N, Szávin-Pósa Á, Lenti K. Treatment of De Quervain's tendinopathy with conservative methods. Orvosi Hetilap. 2020 Mar 1;161(11):419-24.
- ↑ Huisstede BM, Gladdines S, Randsdorp MS, Koes BW. Effectiveness of conservative, surgical, and postsurgical interventions for trigger finger, Dupuytren disease, and De Quervain disease: a systematic review. Archives of physical medicine and rehabilitation. 2018 Aug 1;99(8):1635-49.
- ↑ Weiss AP, Akelman E, Tabatabai M. Treatment of de Quervain's disease. The Journal of hand surgery. 1994 Jul 1;19(4):595-8.
- ↑ 13.0 13.1 Abi-Rafeh J, Kazan R, Safran T, Thibaudeau S. Conservative management of de Quervain stenosing tenosynovitis: review and presentation of treatment algorithm. Plastic and reconstructive surgery. 2020 Apr 15;146(1):105-26.
- ↑ 14.0 14.1 McDermott JD, Ilyas AM, Nazarian LN, Leinberry CF. Ultrasound-guided injections for de Quervain’s tenosynovitis. Clinical Orthopaedics and Related Research®. 2012 Jul;470(7):1925-31.
- ↑ Kume K, Amano K, Yamada S, Amano K, Kuwaba N, Ohta H. In de Quervain’s with a separate EPB compartment, ultrasound-guided steroid injection is more effective than a clinical injection technique: a prospective open-label study. Journal of Hand Surgery (European Volume). 2012 Jul;37(6):523-7.
- ↑ Başar B, Aybar A, Basar G, Başar H. The effectiveness of corticosteroid injection and splint in diabetic de Quervain's tenosynovitis patients: A single-blind, randomized clinical consort study. Medicine. 2021 Sep 3;100(35).
- ↑ Saaiq M. Management Outcome of de Quervain’s Disease with Corticosteroid Injection Versus Surgical Decompression. Archives of Bone and Joint Surgery. 2021 Mar;9(2):167.
- ↑ 18.0 18.1 Goel R, Abzug JM. De Quervain's tenosynovitis: a review of the rehabilitative options. Hand. 2015 Mar;10(1):1-5.
- ↑ Graston IASTM treatment for hand, thumb and wristAvailable from: https://https://youtu.be/8-pjnTwX45s [last accessed 26/10/2021]
- ↑ Rehab my Patient. Abductor pollicis longus strengthening. Available from: https://www.youtube.com/watch?v=3_8SIqWZ8w4&t=9s[last accessed 10 November 2021]
- ↑ Rehab my Patient. Isometric thumb extension. Available from: https://www.youtube.com/watch?v=JlNiPRTe4Rw [last accessed 10 November 2021]
- ↑ Rehab my Patient. Radial deviation isometric. Available from: https://www.youtube.com/watch?v=rSzba5Cq6SM [last accessed 10 November 2021]
- ↑ Rehab my Patient. Thumb and finger band strengthening Available from: https://www.youtube.com/watch?v=5kp45nPJxa8 [last accessed 11 November 2021]
- ↑ Rehab my Patient.Thumb strengthening with band part 1 Available from: https://www.youtube.com/watch?v=0me9b2Kjkbc [last accessed 6/6/2009]
- ↑ Rehab my Patient. Thumb strengthening with band part 2 Available from: https://www.youtube.com/watch?v=IgokBrYeIy8 [last accessed 11 November 2021]
- ↑ Rehab my Patient. Wrist flexion with a band. Available from: https://www.youtube.com/watch?v=qSLGFWWQjfU[last accessed 11 November 2021]
- ↑ Rehab my Patient. Wrist band strengthening. Available from: https://www.youtube.com/watch?v=YetNUU3sCH4 [last accessed 11 November 2021]
- ↑ Rehab my Patient. Radial deviation band Available from: https://www.youtube.com/watch?v=a_92x8kpOqo [last accessed 11 November 2021]
- ↑ Backstrom KM. Mobilization with movement as an adjunct intervention in a patient with complicated de Quervain's tenosynovitis: a case report. Journal of Orthopaedic & Sports Physical Therapy. 2002 Mar;32(3):86-97.
- ↑ Rabin A, Israeli T, Kozol Z. Physiotherapy Management of People Diagnosed with de Quervain's Disease: A Case Series. Physiotherapy Canada. 2015 Aug;67(3):263-7.
- ↑ Savva C, Karagiannis C, Korakakis V, Efstathiou M. The analgesic effect of joint mobilization and manipulation in tendinopathy: a narrative review. Journal of Manual & Manipulative Therapy. 2021 Mar 28:1-2.
- ↑ Bob & Brad | KDe Quervain's Syndrome-How to Stop It When It Just Keeps Hurting! Available from: https://youtu.be/eRCE501w0-s [last accessed 26/10/2021]
- ↑ Kaçmaz İE, Koca A, Basa CD, Zhamilov V, Reisoğlu A. Efficacy of Kinesiologic Taping in de Quervain's Tenosynovitis: Case Series and Review of Literature. Medical Journal of Bakirkoy. 2019 Sep 1;15(3).
- ↑ STRENGTHTAPE®| Kinesiology Tape | De Quervain. Available from: https://youtu.be/n-m9RT7sdUA [last accessed 26/10/2021]
- Assessment
- Hand
- Wrist
- Special Tests
- Tendons
- Texas State University EBP Project
- Vrije Universiteit Brussel Project
- EIM Residency Project
- Musculoskeletal/Orthopaedics
- Primary Contact
- Sports Medicine
- Sports Injuries
- Conditions
- Wrist - Conditions
- Hand - Conditions
- Hand - Special Tests
- Wrist - Special Tests
- Course Pages
- Physioplus Content