Considering the Stress Pain Cycle in Assessment: Difference between revisions
Kim Jackson (talk | contribs) No edit summary |
Kim Jackson (talk | contribs) No edit summary |
||
| Line 15: | Line 15: | ||
==== Physiological Response to Stress ==== | ==== Physiological Response to Stress ==== | ||
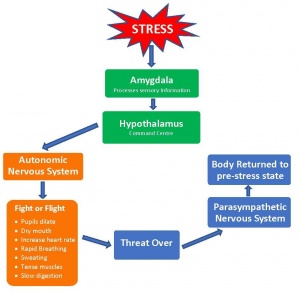
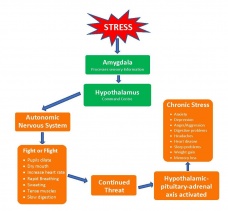
When we are faced with a stressor messages that come from our senses are processed in the brain, this information is then sent to amygdala, (defintion). The first step in this process is for our bodies to determine the severity of the threat, based on our senses, perception and memories. If the threat is strong and our processing decides action is necessary then the hypothalamus is activated. The hypothalmus is the command centre of the brain and communicates with the rest of the body through the two branches of the autonomic system. The sympathetic nervous system, that stimulates the adrenal glands releasing adrenaline (epinephrine) and cortisol into the blood stream triggering physiological changes preparing us for action and the parasympathetic nervous system, that acts to slow down the response (diagram). However, if the stress chronic,repeated, ongoing or long-term, then the responses designed to protect us actually become detrimental to our health(diagram) | When we are faced with a stressor messages that come from our senses are processed in the brain, this information is then sent to amygdala, (defintion). The first step in this process is for our bodies to determine the severity of the threat, based on our senses, perception and memories. If the threat is strong and our processing decides action is necessary then the hypothalamus is activated. The hypothalmus is the command centre of the brain and communicates with the rest of the body through the two branches of the autonomic system. The sympathetic nervous system, that stimulates the adrenal glands releasing adrenaline (epinephrine) and cortisol into the blood stream triggering physiological changes preparing us for action and the parasympathetic nervous system, that acts to slow down the response (diagram). However, if the stress chronic,repeated, ongoing or long-term, then the responses designed to protect us actually become detrimental to our health(diagram) | ||
[[File:Stress response 1.jpg|left|alt=Acute Stress - Physiological Response|'''Acute Stress -Physiological Response'''|none|thumb]][[File:Stress_response_2.jpg|right||none|thumb|228x228px|Chronic Stress - Physiological Response]]{{#ev:youtube | dErTZ-zj1dQ | 180<ref>Intro to Psychology. Two Pathways for Stress Response. Available from: https://www.youtube.com/watch?v=dErTZ-zj1dQ</ref>}} | [[File:Stress response 1.jpg|left|200|alt=Acute Stress - Physiological Response|'''Acute Stress -Physiological Response'''|none|thumb]][[File:Stress_response_2.jpg|right|200|none|thumb|228x228px|Chronic Stress - Physiological Response]]{{#ev:youtube | dErTZ-zj1dQ | 180<ref>Intro to Psychology. Two Pathways for Stress Response. Available from: https://www.youtube.com/watch?v=dErTZ-zj1dQ</ref>}} | ||
==== The Relationship between Chronic Pain and Stress ==== | ==== The Relationship between Chronic Pain and Stress ==== | ||
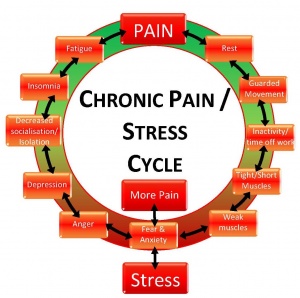
It has been established that [https://www.physio-pedia.com/Chronic_Pain chronic pain] can contribute to stress and also stress can contribute to chronic pain. The burden of of a long-term illness or disability can put a lot of emotional and financial pressure on a person, the worry of not being able to work or feeling excluded from activities as well as feeling misunderstood can have a negative impact on the way a person sees their role within their family and society. Table 1 shows the link between chronic stress and pain. | It has been established that [https://www.physio-pedia.com/Chronic_Pain chronic pain] can contribute to stress and also stress can contribute to chronic pain. The burden of of a long-term illness or disability can put a lot of emotional and financial pressure on a person, the worry of not being able to work or feeling excluded from activities as well as feeling misunderstood can have a negative impact on the way a person sees their role within their family and society. Table 1 shows the link between chronic stress and pain. | ||
Revision as of 18:42, 19 June 2018
Original Editor - Your name will be added here if you created the original content for this page.
Top Contributors - Kim Jackson, Admin, George Prudden, Claire Knott, Lucinda hampton and Jess Bell
Introduction[edit | edit source]
Physiotherapists are trained professionals who, on a daily basis, help clients deal with pain and movement dysfunction. As the profession has moved towards evidence based practice the way a client's therapy is delivered has also changed, we are moving away from didactic teaching and anecdotal practices, to provide the client with interventions that are based not only our clinical experiences but solid research[1]. This has led to to changing from the biomedical based approach to a more client centred biopsychosocial approach. This has been largely influenced by the recognition that emotional factors such as fear, anxiety and stress can delay and impede the recovery of those suffering from pain. Fear and anxiety may be personality traits but they can also be a byproduct of stress and stress has now been recognised as a factor in pain. It is well known that short term stress can be beneficial, especially in a crisis, but persistent or long term (chronic stress) can be the cause of pain. It has also been determined that stress can be one of the symptoms of chronic pain. In order to fully understand the shift in assessment and treatment approaches it is important to understand stress and also how people’s behaviour and fears affects not only their pain but also their perception and approach to pain and participation recovery.
What is Stress?[edit | edit source]
Stress is an emotional (and physiological) response to either a known or perceived threat and it can be categorised as either acute or chronic. Although just the mention of stress can have a negative connotation, it can also be seen as a positive and necessary process. Acute stress in the face of danger can actually prepare us for response and illicit a fight or flight response, acute stress that is repetitive or not released and chronic stress on the other hand can be negative and detrimental to our health and well-being. It is something until recently that did not receive a lot of attention but the World Health Organisation have recognised the need for strategies to be in place to help those suffering from various forms of stress [2] and have also recognised the increasing problem of stress in the work place, stating that it is becoming a worldwide epidemic (source). To better understand how this impacts physiotherapists it is important to understand not only the biological and physiological response to stress but also the relationship between chronic pain and stress and how it can influence individuals.
Physiological Response to Stress[edit | edit source]
When we are faced with a stressor messages that come from our senses are processed in the brain, this information is then sent to amygdala, (defintion). The first step in this process is for our bodies to determine the severity of the threat, based on our senses, perception and memories. If the threat is strong and our processing decides action is necessary then the hypothalamus is activated. The hypothalmus is the command centre of the brain and communicates with the rest of the body through the two branches of the autonomic system. The sympathetic nervous system, that stimulates the adrenal glands releasing adrenaline (epinephrine) and cortisol into the blood stream triggering physiological changes preparing us for action and the parasympathetic nervous system, that acts to slow down the response (diagram). However, if the stress chronic,repeated, ongoing or long-term, then the responses designed to protect us actually become detrimental to our health(diagram)
The Relationship between Chronic Pain and Stress[edit | edit source]
It has been established that chronic pain can contribute to stress and also stress can contribute to chronic pain. The burden of of a long-term illness or disability can put a lot of emotional and financial pressure on a person, the worry of not being able to work or feeling excluded from activities as well as feeling misunderstood can have a negative impact on the way a person sees their role within their family and society. Table 1 shows the link between chronic stress and pain.
Chronic pain affects ?? adults worldwide[4] (talk about YDLs QofL), it is a debilitating condition that affects not only a person's mobility and function but can also have an impact on their personal relationships, work experience and finances. To feel isolated and separate can affect stress levels but scientific evidence also shows that both chronic pain and chronic stress release the same chemicals and can also result in maldaptive changes in physiology and behaviour.[5] These are not the only factors that determine our response to chronic pain or stress our social upbringing and environment also influence our health and attitude. People of lower social standing, living in impoverished areas are found to have poorer diets and increased exposure to crime and risky behaviours[6]
As mentioned earlier when discussing stress it was established that if a person experiences continued or chronic stress the stress response of flight or fight is not regulated and a new pathway for stress is developed and new memories associated with fear and behaviour are learnt. Chronic pain follows a similar pattern, movement and pain become associated with further damage although in most cases there is little evidence support this. In fact it has been proven that movement and exercise have a positive effect on the management of chronic pain.(ref). Another link between chronic pain and chronic stress is the change in size of the amygdala; in both the amygdala has shown a decrease in volume. In a study undertaken to investigate the effects of chronic pain on the brain 10 patients suffering from hip osteoarthritis showed an increase in amygdala size after surgery and the abolition of pain. The study concluded that the changes in the brain are not the cause of the pain but rather a response to pain.[7] It is a complex area of study but there is no doubt a connection between chronic pain and chronic stress; people's attitudes and responses can influence their participation and commitment to their rehabilitation programme. It is far more difficult to encourage a person in pain to exercise and move, if they have fear behaviours and are also suffering from the effects of chronic stress.
Diagram pain-stress cycle or a diagram showing similiarities of cp and cs
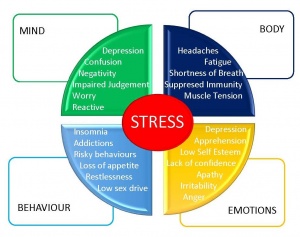
Insert diagram of stress and mind, body, emotions and behaviour
BioMedical vs Biopsychosocial approaches to assessment and treatment[edit | edit source]
Physiotherapists along with other medical professions are taught to recognise the biological aspect of pain and dysfunction – anatomy, physiology and condition/problem based case studies, in class and in our working environments.[8]
However, over the past few years the emphasis is changing to use a client-centred approach where treatment is guided by evidence-based practice. At the core of this approach is encouraging participation of the client in their recovery. When client stress and pain learned behaviours are added to the equation assessment and treatment can become complicated and definitely unique . This is outside the scope and teaching of the biomedical model and n 1977 George Engel a ?? suggested the biopsychosocial mode. This model encourages clinicians to factor in the client's psychological and social experiences as well as the biological aspects of their presenting condition (table). Low back pain is an area where research has shown adopting a biopsychosocial approach to treatment is effective[9][10]
An assessment can be long and detailed process which when including the biopsychosocial model may be daunting; it requires asking questions and paying attention not only to pain intensity and movement dysfunction and restrictions but also to behaviours and beliefs. This can be a complex process and there are factors in place to guide the assessment and subsequent treatments. Physiotherapists are not new to using markers and signs to lead their assessment. A flag system has been developed to identify risk factors in musculoskeletal disorders. Red flags were first introduced into practice in 1994 (CSP) and are used to identify serious pathology. Since then other flags have been introduced to highlight potential barriers to treatment and rehabilitation. (refer to physiopedia page). These flags help guide our approach and give insight in how to engage clients and improve treatment outcomes.
One of the tools that physiotherapist's have access to is the flag system[11]
| Flag | Introduced | Indicators |
|---|---|---|
| Red | 1994 | Serious pathology, eg. |
| Yellow | 1997 | Psychosocial factors, eg |
| Blue | 2000 | Perception to work, eg |
| Black | 2000 | Work conditions inhibiting rehabilitation eg |
| Orange | 2005 | Abnormal psychological processes eg alcohol or drug abuse |
New Approaches to Assessment and Treatment[edit | edit source]
Fortunately the change in practice is being guided by research and new models have been developed. To date the most commonly used models are CFT and TNE, both of these are client-centred with emphasis on psychosocial behaviours and factor in fear, stress and beliefs. Talk about CFT. Talk about TNE
Barriers to a Successful BioPsychoSocial Approach[edit | edit source]
Misunderstanding and misusing flags eg labelling clients rather than using flags to guide interventions, or inappropriately refering client to other disciplines or departments[11]
Patient's biomedical treatment expectations[9]
Good communication and the ability to challenge patient's beliefs[9]
Effectiveness of teaching, interpretation and implementation the biopsychosocial model[12]
Resources[edit | edit source]
- bulleted list
- x
or
- numbered list
- x
References[edit | edit source]
- ↑ Schreiber J, Stern P. A Review of the Literature on Evidence-Based Practice in Physical Therapy. The Internet Journal of Allied Health Sciences and Practice, 2005, 2005 Oct 01;3(4) Article 9
- ↑ WHO guidelines on conditions specifically related to stress
- ↑ Intro to Psychology. Two Pathways for Stress Response. Available from: https://www.youtube.com/watch?v=dErTZ-zj1dQ
- ↑ Breivik H, Collett B, Ventafridda V, Choen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10:287-333
- ↑ Abdallah CG, Geha P. Chronic Pain and Chronic Stress: Two sides of the same coin? Chronic Stress (Thousand Oaks, Calif.) 2017 Feb 1: 10.1177/2470547017704763
- ↑ Cohen S, Janicki-Deverts D, Chen E, Matthews KA. Childhood socioeconomic status and adult health. Ann N Y Acad Sc. 2010;1186:37-55
- ↑ Rodiriguez-Raecke R, Niemeier A, Ihle K, Ruether W, May A. Brain gray matter decrease in chronic pain is the consequence and not the cause of pain. J Neurosci. 2009;29:13746-13750
- ↑ Pincus T, Vogel S, Breen A, Foster N, Underwood M. Persistent back pain - why do physical therapy clinicians continue treatment? A mixed methods study of chiropractors, osteopaths and physiotherapists. Eur Journal of Pain 2006;10(1):67-76
- ↑ 9.0 9.1 9.2 Synnott A, O'Keefe M, Bunzli S, Dankaerts W, O'Sullivan P, O'Sullivan K. Physiotherapists may stigmatise or feel unprepared to treat people with low ack pain and psychosocial factors that influence recovery: a systematic review. Journal of Physiotherapy 61 (2015) 68-76
- ↑ Kendall NA. Psychosocial approaches to the prevention of chronic pain: the low back paradigm. Best Practice Re Clinical Rheumatology. 1999; 13(3):545-554
- ↑ 11.0 11.1 11.2 Carvalho A. How useful are flags for identifying the origins of pain and barriers to rehabilitation. CSP - Frontline. 2007 September 5;13(17)
- ↑ Overmeer T, Boersma K,Denison E, Linton SJ. Doesteaching physical therapists to deliver a biopsychosocial treatment programe result in better patient outcomes? A randomised controlled trial. Physical Therapy Review 2005; 91(5):804-819