Compartment Syndrome of the Foot: Difference between revisions
Tomer Yona (talk | contribs) No edit summary |
Leana Louw (talk | contribs) No edit summary |
||
| (33 intermediate revisions by 11 users not shown) | |||
| Line 6: | Line 6: | ||
== Definition/Description == | == Definition/Description == | ||
Compartment syndrome is a condition where bleeding or edema develops in an area of the body which is surrounded by non-expandable structures of bone and fascia, increasing the local pressure and causing circulatory disturbance in that space. This can lead to ischaemia and necrosis if left improperly diagnosed.The cause is usually following acute trauma<ref name=":0">Frink M, Hildebrand F, Krettek C, Brand J, Hankemeier S. [https://link.springer.com/article/10.1007/s11999-009-0891-x Compartment syndrome of the lower leg and foot.] Clinical Orthopaedics and Related Research 2010;468(4):940-50. </ref> or it can be due to intense or overly frequent exercise (chronic exertional compartment syndrome) or overly tight casts. Fasciotomy is usually performed although non surgical treatment is also an option.<ref name=":0" /><ref name="Abraham et al.">Medscape. Acute compartment syndrome. Available from: https://emedicine.medscape.com/article/307668-overview (accessed 06/04/2020).</ref> | |||
== Clinically Relevant Anatomy == | |||
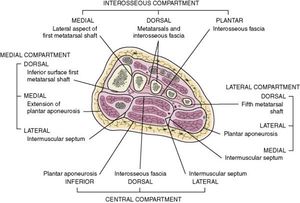
= | The [[Foot Anatomy|foot]] is divided into 4 large compartments (interosseous, medial, lateral, central) each including muscles, nerves and arteries, although it is debated whether there are actually 9 compartments, however, it is more practical to think of the foot in 4 compartments.<ref name="BRON 2">Ortho Info. Compartment syndrome. Available from: https://orthoinfo.aaos.org/en/diseases--conditions/compartment-syndrome/ (accessed 04/06/2020). </ref> | ||
There are three compartments, medial, lateral and superficial that run the entire length of the [[Foot Anatomy|foot]]. although a 4th, the calcaneal compartment has been described in patients who develop progressive claw-toe deformities due to [[Calcaneal Fractures|calcaneal fractures]], [[File:C3.jpg|thumb]] | |||
The boundary between flexor digitorum brevis and the calcaneal compartment ([[Quadratus Plantae|quadratus plantae]]) becomes incompetent at a pressure gradient of less than 10mm Hg, so tissue perfusion becomes insignificant, effectively creating an independent compartment syndrome.<ref name="Guyton et al.">Guyton GP, Shearman CM, Saltzman CL. [https://pdfs.semanticscholar.org/6280/3847824176a1b538fc9082ff2219d09584bf.pdf The compartments of the foot revisited: rethinking the validity of cadaver infusion experiments.] The Journal of bone and joint surgery, British volume 2001;83(2):245-9.</ref><ref name="Manoli A et al." /> | |||
{| border="1" cellspacing="1" cellpadding="1" width=" | {| border="1" cellspacing="1" cellpadding="1" width="100%" | ||
|- | |- | ||
| valign="top" width="250" align="left" | ''' | | valign="top" width="250" align="left" | '''Interosseous compartment''' | ||
*Dorsal interossei muscles | |||
*Plantar interossei muscles | |||
*Plantar lateral artery, vein and nerve | |||
'''<br>''' | '''<br>''' | ||
| valign="middle" width="250" align="left" | ''' | | valign="middle" width="250" align="left" | '''Medial compartment''' | ||
* Abductor hallucis | |||
* Flexor hallucis brevis | |||
*Tendon of flexor hallucis brevis | |||
*Medial plantar arteries, veins and nerves | |||
<br> | <br> | ||
|- | |- | ||
| valign="top" width="250" align="left" | ''' | | valign="top" width="250" align="left" | '''Lateral compartment:''' | ||
* [[Abductor Digiti Minimi (Foot)|Abductor digiti minimi]]/quinti | |||
* Flexor digiti minimi | |||
*Opponens digiti minimi | |||
*Branches of the lateral plantar artery vein and nerve | |||
<br> | <br> | ||
| valign="top" width="250" align="left" | | | valign="top" width="250" align="left" | '''Central compartment''' '''(3 levels)''' | ||
''' | * <u>First level:</u> Adductor hallucis | ||
* <u>Second level:</u> [[Quadratus Plantae|Quadratus plantae]]; lumbrical muscles; tendons of [[flexor digitorum longus]] | |||
*<u>Third level:</u> Flexor digitorum brevis | |||
*All levels of the central compartment contain (deep) branches of the plantar lateral artery, vein and nerve<br> | |||
|} | |} | ||
== Epidemiology /Etiology == | |||
[[Image:Compartments of the foot-14E9C44BFB5786DE26D.jpg|thumb|right|300x300px]] | [[Image:Compartments of the foot-14E9C44BFB5786DE26D.jpg|thumb|right|300x300px]] | ||
Incidence of compartment syndrome of the foot is low. The calcaneal compartment seems to be at higher risk for developing compartment syndrome, whereas the interosseous compartments are usually at a lower risk.<ref name=":0" /><ref name="Manoli A et al.">Manoli A, Weber TG. [https://journals.sagepub.com/doi/abs/10.1177/107110079001000505 Fasciotomy of the foot: an anatomical study with special reference to release of the calcaneal compartment.] Foot Ankle 1990;10:267–275.</ref><ref name="Myerson et al.">Myerson MS. [https://europepmc.org/article/med/1680591 Management of compartment syndromes of the foot.] Clinical orthopaedics and related research 1991(271):239-48.</ref><ref name="Shereff et al.">Shereff MJ. [https://europepmc.org/article/med/1970832 Compartment syndromes of the foot.] Instructional course lectures 1990;39:127-32.</ref> | |||
< | Chronic (exertional) compartment syndrome can develop through over exertion during sporting activity. The muscles become fatigued and irritated resulting in an inflammatory response and swelling. Sports like football, motorcross, running, tennis and gymnastics can be risk factors.<ref name="BRON 8">Physio Adviser. Compartment Syndrome (Deep Posterior). Available from: http://www.physioadvisor.com.au/10513350/compartment-syndrome-chronic-compartment-syndrom.htm (accessed 06/04/2020).</ref> Training programmes may be inappropriate or incorrect footwear could be a cause.<ref name="BRON 2" /> Other causes can be biomechanical abnormailities, limb length differences, muscle weakness or muscular tightness.<ref name="BRON 8" /> | ||
< | Crush injuries are the most common cause of compartment syndromes of the foot <ref name="BRON 2" />, as well as snake bites, burns, too tightly fitted bandages or casts, [[Metatarsal Fractures|metatarsal fractures]], [[talus]] or [[Calcaneal Fractures|calcaneus fractures]], [[Chopart fracture-dislocation|Chopart]] and/or [[Lisfranc Injuries|Lisfranc joint dislocations]],<ref name="BRON 2" /> steroid or creatine use which can cause muscles to increase in volume.<ref name="BRON 7">Tucker Alicia K. Chronic exertional compartment syndrome of the leg. Current Reviews in Musculoskeletal Medicine. 2 September 2010 http://ukpmc.ac.uk/articles/PMC2941579/ (accessed on november/december 2010) Level of evidence: A1</ref> | ||
== Characteristics/Clinical Presentation == | |||
< | |||
< | Pain is one of the key symptoms for compartment syndrome, being severe and spontaneous or occurring during active exercises, often increasing in intensity as the activity continues, only resolving on rest. Typically, the pain is described as an aching and/or burning sensation.<ref name="Tucker Alicia K. et al." /> | ||
'''Movement usually eliciting pain:'''<ref name=":0" /><ref name="Abraham et al." /><ref name="Tucker Alicia K. et al." /><ref name="Ulmer T. et al.">Ulmer T. [https://journals.lww.com/jorthotrauma/Abstract/2002/09000/The_Clinical_Diagnosis_of_Compartment_Syndrome_of.6.aspx The clinical diagnosis of compartment syndrome of the lower leg: are clinical findings predictive of the disorder?] Journal of orthopaedic trauma 2002;16(8):572-7. </ref> | |||
*Pain with passive stretching | |||
*Pain during active dorsiflexion of the [[Ankle Joint|ankle]] | |||
*Increased soreness caused by moving the toes | |||
*Pain on palpation or compressing the affected compartments | |||
< | '''Other relevant signs:'''<ref name=":0" /><ref name="Abraham et al." /><ref name="Tucker Alicia K. et al." /><ref name="Ulmer T. et al." /> | ||
< | *Swelling and tightness | ||
*Pale skin in the area of tissue damage | |||
*Sensory deficits caused by neurological injury<ref name="Vaillancourt C. et al.">Vaillancourt C, Shrier I, Vandal A, Falk M, Rossignol M, Vernec A, Somogyi D. [https://www.cambridge.org/core/journals/canadian-journal-of-emergency-medicine/article/acute-compartment-syndrome-how-long-before-muscle-necrosis-occurs/0BC7916DBCB088647ED7266A772D48CF Acute compartment syndrome: how long before muscle necrosis occurs?] Canadian Journal of Emergency Medicine 2004;6(3):147-54.</ref> | |||
*Firmness of the involved compartments<ref name="Tucker Alicia K. et al." /> | |||
*Muscle weakness of the intrinsic foot muscles<ref name="Tucker Alicia K. et al.">Tucker AK. [https://link.springer.com/article/10.1007/s12178-010-9065-4 Chronic exertional compartment syndrome of the leg.] Current reviews in musculoskeletal medicine 2010;3(1-4):32-7.</ref> | |||
< | The 5 P’s may be considered when diagnosing compartment syndrome: '''P'''ain, '''P'''allor, '''P'''aresthesia, '''P'''aralysis, '''P'''ulselessness <ref name="BRON 1">Schünke M, Schulte E, Schumacher U, Voll M, Wesker K. Prometheus. Bohn Stafleu Van Loghum, Houten 2005. Pg 463</ref> | ||
< | |||
== Differential Diagnosis == | |||
Compartment syndrome is characterised by an increase of the interstitial pressure with severe pain and pain associated with passive stretching of the muscles as a result. Other consequences consist of a reduced supply of blood and fluid supply to tissues.<ref name=":0" /> | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
Awareness of the signs and symptoms specific to this syndrome are key to an accurate diagnosis, alongside an appropriate clinical examination.<ref name=":0" /> Where compartment syndrome is suspected, frequent examination is required in the acute phase, sometimes hourly, as muscle necrosis can occur within 3 hours.<ref name="Vaillancourt C. et al." /> | |||
= | A quick and safe procedure to diagnose compartment syndrome is invasive measurement.<ref name="Whitesides et al.">Whitesides TE, Haney TC, Harada H, Holmes HE, Morimoto K. [https://jamanetwork.com/journals/jamasurgery/article-abstract/581027 A simple method for tissue pressure determination.] Archives of Surgery 1975;110(11):1311-3.</ref> where a needle is placed into the area, the only valuable test to diagnose this syndrome, otherwise known as [[Compartment Syndrome|intracompartmental pressure monitoring]]. | ||
== Outcome measures == | |||
Foot and Ankle visual analog scale from the American Orthopaedic Foot and Ankle Society measures the quality of life after fasciotomy.<ref name="Han F. et al.">Han F, Daruwalla ZJ, Shen L, Kumar VP. [https://www.sciencedirect.com/science/article/pii/S106725161400444X A prospective study of surgical outcomes and quality of life in severe foot trauma and associated compartment syndrome after fasciotomy.] The Journal of Foot and Ankle Surgery 2015;54(3):417-23.</ref> | |||
== Physical Examination == | |||
Awareness of the complication, an appropriate clinical examination, comparison of the affected foot to the unaffected foot with attention to the syndrome's specific symptoms are most important. Pain levels are assessed through palpation and active and passive range of motion tests on the patient. | |||
== | '''Physically relevant findings that may occur for compartment syndrome:'''<ref name=":0" /><ref name="Guyton et al." /> | ||
*Weak dorsiflexion (anterior compartment) | |||
*Weak eversion (lateral compartment) | |||
*Weak plantar flexion (posterior compartment) | |||
== Medical Management == | |||
It is necessary to immediately carry out a fasciotomy in order to remove the excess pressure. A cast or brace can be used, but they should be left open for patients with severe pain and/or excess pressure in the affected compartment. Affected limbs should not be raised in order to not affect the already impaired blood flow any further.<ref name=":0" /> | |||
Emergency decompressive fasciotomy is conducted with an acute compartment syndrome. | |||
''' | *'''Indication: '''when the intracompartmental pressure measurement has an absolute value of 30-45 mm Hg. | ||
*'''Techniques: ''' | |||
**Dual dorsal incision is the gold standard technique. A dorsal medial and lateral incision is made to release the compartments. | |||
**A single medial incision is used to release all compartments, but it is technically more challenging. | |||
**'''Complications:''' chronic pain and hypersensitivity are possible complications and can be difficult to manage. Sometimes claw toes develops.<ref name="kardsheh M">Ortho Bullets. Foot Compartment Syndrome. Available from: https://www.orthobullets.com/trauma/1065/foot-compartment-syndrome (accessed 27/12/2016).</ref> | |||
== Physiotherapy Management == | |||
Non-operative treatment is generally not successful.<ref name="BRON 13">Bong MR, Polatsch DB, Jazrawi LM, Rokito AS. [https://pdfs.semanticscholar.org/e36f/04d74152ef531e43a1828b1075a79003ee20.pdf Chronic Exertional Compartment Syndrome.] Bulletin of the NYU Hospital for Joint Diseases 2005;62. </ref> Post-operatively, patients are advised to use ice and anti-inflammatory medication to reduce swelling and to rest. An exercise programme is given to improve muscle weakness and to stimulate [[Proprioception|proprioceptive]] sensors. | |||
[[Massage|Soft tissue massage]]<ref name="BRON 8" /> may be used to provide lymphatic drainage. Passive mobilisation of the ankle joint, the metatarsals and phalanges<ref name="BRON 8" /> is useful for increased range of motion and mobility of joints along with lower limb stretches. | |||
Orthotics<ref name="BRON 2" /><ref name="BRON 8" /> can be prescribed where there are biomechanical defaults. <br> | |||
'''Recommended strength exercises for the intrinsic foot muscles:''' | |||
*Toe curl: Place a towel beneath the feet of the patient and ask them to pull the towel towards them by curling the toes into the towel. | |||
*Picking up marbles or other small objects: The patient has to claw their toes to be able to pick up the object from the floor. | |||
*Walking: Early post-operative exercises include mobilising with [[crutches]], gradually progressing to full weight bearing | |||
*Toe squeeze: Soft objects are squeezed between the toes and held for 5 seconds | |||
*Toe raises, toe curls | |||
*Dorsal and plantar flexion, inversion and eversion using a resistance band<ref name="BRON 9">Physio Adviser. Ankle stretches. Available from:http://www.physioadvisor.com.au/8047989/ankle-flexibility-exercises-ankle-sprains-ankle.htm (accessed 06/04/2020).</ref> | |||
If pain or swelling occurs during or after exercise, elevate the foot and use ice to reduce the swelling. | |||
== Clinical Bottom Line == | |||
Compartment syndrome needs immediate surgical treatment to avoid ischemia, possible functional impairment and/or potential nerve damage of the foot.<ref name=":0" /> | |||
== References == | == References == | ||
<references />[[Category:Vrije_Universiteit_Brussel_Project]] | |||
[[Category:Musculoskeletal/Orthopaedics|Orthopaedics]] | |||
[[Category:Foot]] | |||
[[Category:Conditions]] | |||
[[Category:Foot - Conditions]] | |||
[[Category:Vrije_Universiteit_Brussel_Project]] [[Category:Musculoskeletal/Orthopaedics|Orthopaedics]] [[Category:Foot]] | [[Category:Sports Medicine]] | ||
[[Category:Acute Care]] | |||
Latest revision as of 17:16, 6 April 2020
Original Editors - Jessie Tourwe
Top Contributors - Jessie Tourwe, Admin, Scott Cornish, Shaimaa Eldib, Tomer Yona, Rachael Lowe, Samrah khan, Kim Jackson, Leana Louw, Kevin Vandebroucq, Karen Wilson, Wanda van Niekerk, 127.0.0.1 and Sigrid Bortels
Definition/Description[edit | edit source]
Compartment syndrome is a condition where bleeding or edema develops in an area of the body which is surrounded by non-expandable structures of bone and fascia, increasing the local pressure and causing circulatory disturbance in that space. This can lead to ischaemia and necrosis if left improperly diagnosed.The cause is usually following acute trauma[1] or it can be due to intense or overly frequent exercise (chronic exertional compartment syndrome) or overly tight casts. Fasciotomy is usually performed although non surgical treatment is also an option.[1][2]
Clinically Relevant Anatomy[edit | edit source]
The foot is divided into 4 large compartments (interosseous, medial, lateral, central) each including muscles, nerves and arteries, although it is debated whether there are actually 9 compartments, however, it is more practical to think of the foot in 4 compartments.[3]
There are three compartments, medial, lateral and superficial that run the entire length of the foot. although a 4th, the calcaneal compartment has been described in patients who develop progressive claw-toe deformities due to calcaneal fractures,
The boundary between flexor digitorum brevis and the calcaneal compartment (quadratus plantae) becomes incompetent at a pressure gradient of less than 10mm Hg, so tissue perfusion becomes insignificant, effectively creating an independent compartment syndrome.[4][5]
Interosseous compartment
|
Medial compartment
|
Lateral compartment:
|
Central compartment (3 levels)
|
Epidemiology /Etiology [edit | edit source]
Incidence of compartment syndrome of the foot is low. The calcaneal compartment seems to be at higher risk for developing compartment syndrome, whereas the interosseous compartments are usually at a lower risk.[1][5][6][7]
Chronic (exertional) compartment syndrome can develop through over exertion during sporting activity. The muscles become fatigued and irritated resulting in an inflammatory response and swelling. Sports like football, motorcross, running, tennis and gymnastics can be risk factors.[8] Training programmes may be inappropriate or incorrect footwear could be a cause.[3] Other causes can be biomechanical abnormailities, limb length differences, muscle weakness or muscular tightness.[8]
Crush injuries are the most common cause of compartment syndromes of the foot [3], as well as snake bites, burns, too tightly fitted bandages or casts, metatarsal fractures, talus or calcaneus fractures, Chopart and/or Lisfranc joint dislocations,[3] steroid or creatine use which can cause muscles to increase in volume.[9]
Characteristics/Clinical Presentation[edit | edit source]
Pain is one of the key symptoms for compartment syndrome, being severe and spontaneous or occurring during active exercises, often increasing in intensity as the activity continues, only resolving on rest. Typically, the pain is described as an aching and/or burning sensation.[10]
Movement usually eliciting pain:[1][2][10][11]
- Pain with passive stretching
- Pain during active dorsiflexion of the ankle
- Increased soreness caused by moving the toes
- Pain on palpation or compressing the affected compartments
Other relevant signs:[1][2][10][11]
- Swelling and tightness
- Pale skin in the area of tissue damage
- Sensory deficits caused by neurological injury[12]
- Firmness of the involved compartments[10]
- Muscle weakness of the intrinsic foot muscles[10]
The 5 P’s may be considered when diagnosing compartment syndrome: Pain, Pallor, Paresthesia, Paralysis, Pulselessness [13]
Differential Diagnosis[edit | edit source]
Compartment syndrome is characterised by an increase of the interstitial pressure with severe pain and pain associated with passive stretching of the muscles as a result. Other consequences consist of a reduced supply of blood and fluid supply to tissues.[1]
Diagnostic Procedures[edit | edit source]
Awareness of the signs and symptoms specific to this syndrome are key to an accurate diagnosis, alongside an appropriate clinical examination.[1] Where compartment syndrome is suspected, frequent examination is required in the acute phase, sometimes hourly, as muscle necrosis can occur within 3 hours.[12]
A quick and safe procedure to diagnose compartment syndrome is invasive measurement.[14] where a needle is placed into the area, the only valuable test to diagnose this syndrome, otherwise known as intracompartmental pressure monitoring.
Outcome measures[edit | edit source]
Foot and Ankle visual analog scale from the American Orthopaedic Foot and Ankle Society measures the quality of life after fasciotomy.[15]
Physical Examination[edit | edit source]
Awareness of the complication, an appropriate clinical examination, comparison of the affected foot to the unaffected foot with attention to the syndrome's specific symptoms are most important. Pain levels are assessed through palpation and active and passive range of motion tests on the patient.
Physically relevant findings that may occur for compartment syndrome:[1][4]
- Weak dorsiflexion (anterior compartment)
- Weak eversion (lateral compartment)
- Weak plantar flexion (posterior compartment)
Medical Management[edit | edit source]
It is necessary to immediately carry out a fasciotomy in order to remove the excess pressure. A cast or brace can be used, but they should be left open for patients with severe pain and/or excess pressure in the affected compartment. Affected limbs should not be raised in order to not affect the already impaired blood flow any further.[1]
Emergency decompressive fasciotomy is conducted with an acute compartment syndrome.
- Indication: when the intracompartmental pressure measurement has an absolute value of 30-45 mm Hg.
- Techniques:
- Dual dorsal incision is the gold standard technique. A dorsal medial and lateral incision is made to release the compartments.
- A single medial incision is used to release all compartments, but it is technically more challenging.
- Complications: chronic pain and hypersensitivity are possible complications and can be difficult to manage. Sometimes claw toes develops.[16]
Physiotherapy Management[edit | edit source]
Non-operative treatment is generally not successful.[17] Post-operatively, patients are advised to use ice and anti-inflammatory medication to reduce swelling and to rest. An exercise programme is given to improve muscle weakness and to stimulate proprioceptive sensors.
Soft tissue massage[8] may be used to provide lymphatic drainage. Passive mobilisation of the ankle joint, the metatarsals and phalanges[8] is useful for increased range of motion and mobility of joints along with lower limb stretches.
Orthotics[3][8] can be prescribed where there are biomechanical defaults.
Recommended strength exercises for the intrinsic foot muscles:
- Toe curl: Place a towel beneath the feet of the patient and ask them to pull the towel towards them by curling the toes into the towel.
- Picking up marbles or other small objects: The patient has to claw their toes to be able to pick up the object from the floor.
- Walking: Early post-operative exercises include mobilising with crutches, gradually progressing to full weight bearing
- Toe squeeze: Soft objects are squeezed between the toes and held for 5 seconds
- Toe raises, toe curls
- Dorsal and plantar flexion, inversion and eversion using a resistance band[18]
If pain or swelling occurs during or after exercise, elevate the foot and use ice to reduce the swelling.
Clinical Bottom Line[edit | edit source]
Compartment syndrome needs immediate surgical treatment to avoid ischemia, possible functional impairment and/or potential nerve damage of the foot.[1]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 1.9 Frink M, Hildebrand F, Krettek C, Brand J, Hankemeier S. Compartment syndrome of the lower leg and foot. Clinical Orthopaedics and Related Research 2010;468(4):940-50.
- ↑ 2.0 2.1 2.2 Medscape. Acute compartment syndrome. Available from: https://emedicine.medscape.com/article/307668-overview (accessed 06/04/2020).
- ↑ 3.0 3.1 3.2 3.3 3.4 Ortho Info. Compartment syndrome. Available from: https://orthoinfo.aaos.org/en/diseases--conditions/compartment-syndrome/ (accessed 04/06/2020).
- ↑ 4.0 4.1 Guyton GP, Shearman CM, Saltzman CL. The compartments of the foot revisited: rethinking the validity of cadaver infusion experiments. The Journal of bone and joint surgery, British volume 2001;83(2):245-9.
- ↑ 5.0 5.1 Manoli A, Weber TG. Fasciotomy of the foot: an anatomical study with special reference to release of the calcaneal compartment. Foot Ankle 1990;10:267–275.
- ↑ Myerson MS. Management of compartment syndromes of the foot. Clinical orthopaedics and related research 1991(271):239-48.
- ↑ Shereff MJ. Compartment syndromes of the foot. Instructional course lectures 1990;39:127-32.
- ↑ 8.0 8.1 8.2 8.3 8.4 Physio Adviser. Compartment Syndrome (Deep Posterior). Available from: http://www.physioadvisor.com.au/10513350/compartment-syndrome-chronic-compartment-syndrom.htm (accessed 06/04/2020).
- ↑ Tucker Alicia K. Chronic exertional compartment syndrome of the leg. Current Reviews in Musculoskeletal Medicine. 2 September 2010 http://ukpmc.ac.uk/articles/PMC2941579/ (accessed on november/december 2010) Level of evidence: A1
- ↑ 10.0 10.1 10.2 10.3 10.4 Tucker AK. Chronic exertional compartment syndrome of the leg. Current reviews in musculoskeletal medicine 2010;3(1-4):32-7.
- ↑ 11.0 11.1 Ulmer T. The clinical diagnosis of compartment syndrome of the lower leg: are clinical findings predictive of the disorder? Journal of orthopaedic trauma 2002;16(8):572-7.
- ↑ 12.0 12.1 Vaillancourt C, Shrier I, Vandal A, Falk M, Rossignol M, Vernec A, Somogyi D. Acute compartment syndrome: how long before muscle necrosis occurs? Canadian Journal of Emergency Medicine 2004;6(3):147-54.
- ↑ Schünke M, Schulte E, Schumacher U, Voll M, Wesker K. Prometheus. Bohn Stafleu Van Loghum, Houten 2005. Pg 463
- ↑ Whitesides TE, Haney TC, Harada H, Holmes HE, Morimoto K. A simple method for tissue pressure determination. Archives of Surgery 1975;110(11):1311-3.
- ↑ Han F, Daruwalla ZJ, Shen L, Kumar VP. A prospective study of surgical outcomes and quality of life in severe foot trauma and associated compartment syndrome after fasciotomy. The Journal of Foot and Ankle Surgery 2015;54(3):417-23.
- ↑ Ortho Bullets. Foot Compartment Syndrome. Available from: https://www.orthobullets.com/trauma/1065/foot-compartment-syndrome (accessed 27/12/2016).
- ↑ Bong MR, Polatsch DB, Jazrawi LM, Rokito AS. Chronic Exertional Compartment Syndrome. Bulletin of the NYU Hospital for Joint Diseases 2005;62.
- ↑ Physio Adviser. Ankle stretches. Available from:http://www.physioadvisor.com.au/8047989/ankle-flexibility-exercises-ankle-sprains-ankle.htm (accessed 06/04/2020).