Chopart fracture-dislocation: Difference between revisions
(replace wrong ampersand with single one) |
No edit summary |
||
| (25 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor ''' [[User:Zoë Vaes|Zoë Vaes]] |
'''Original Editor ''' [[User:Zoë Vaes|Zoë Vaes]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} </div> | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} </div> | ||
== Definition/Description<br> == | == Definition/Description == | ||
A Chopart fracture-dislocation is a dislocation of the mid-tarsal joints of the foot, often with associated [http://www.physio-pedia.com/index.php5?title=Calcaneal_fracture fractures of the calcaneus], [[cuboid]] and [[navicular]] bone. | |||
== Clinically Relevant Anatomy == | |||
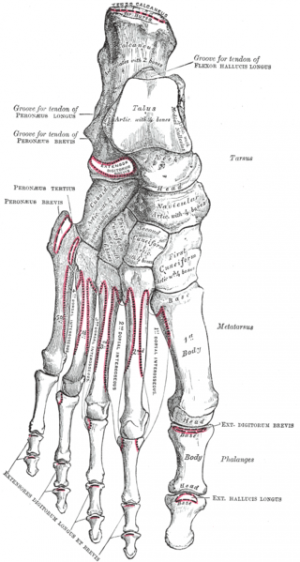
The transverse tarsal joint is also called the midtarsal joint and is referred to as Chopart’s joint. The midtarsal joint is composed of the talonavicular and calcaneocuboid joints.<ref name="p1">Puthezhath, K., Veluthedath, R., Kumaran, C.M., & Patinharayil, G. (2009). Acute Isolated Dorsal Midtarsal (Chopart's) Dislocation: A Case Report [electronic version]. The Journal of Foot and Ankle Surgery, Vol. 48, No.4 , 462-465. B</ref> The bones which form the Chopart joint are the [[talus]] and [[calcaneus]] proximally, and the [[navicular]] and [[cuboid]] bone distally. When the foot skeleton is viewed from above, the joint line of the transverse tarsal articulation has the shape of an 'S'.<ref name="p2">Signe Brunnstrom, M.A. (1975). Clinical Kinesiology. Philadelphia: F.A. Davis Company.</ref> | |||
== Epidemiology / Etiology == | |||
Among the uncommon midfoot injuries, Chopart joint dislocations or fracture-dislocations are the most severe injuries.<sup><ref name="p3">Richter, M., Thermann, H., Huefner, T., Schmidt, U., Goesling, T., & Krettek, C. (2004). Foot & Ankle International, Vol 25., No.5, 340-348. 5 november, 2011. http://www.krankenhaus-rummelsberg.de/uploads/tx_templavoila/chopart.pdf</ref></sup> Chopart fracture-dislocations are caused most commonly by motor vehicle accidents and falls from a height. [[Avulsion Fractures of the Ankle|Avulsion fractures]] localized to the midfoot are typically caused by low-energy trauma e.g. sprain or sports injuries. Concomitant fractures occur in approximately 75% to 90% of Chopart injuries, and only 10% to 25% of Chopart dislocations are pure ligamentous injuries.<sup><ref name="p4">Van Dorp, K.B., De Vries, M.R., Van der Elst, M., & Schepers, T. (2010). Chopart Joint Injury: A Study of Outcome and Morbidity [electronic version]. The Journal of Foot and Ankle Surgery, Vol. 49, No. 6, 541-545. C</ref></sup> Injuries with a combined Chopart and [[Lisfranc Injuries|Lisfranc fracture-dislocation]] are often part of so called "crush" injuries of the foot.<ref name="p5">Richter, M., Wippermann, B., Krettek, C., Schratt, H.E., Hufner, T., & Thermann, H. (2001). Foot & Ankle International, Vol. 22, No. 5, 392-379. 5 november, 2011. http://olc.metrohealth.org/SubSpecialties/Trauma/Media/Other/Fractures%20and%20fracture-dislocations%20of%20the%20midfoot,%20occurrence,%20causes,%20long-term%20results.pdf A</ref> | |||
Main and Jowet classified midtarsal joint injuries into five groups, according to the direction of the deforming force and the resulting displacement of the forefoot:<ref name="p1" /> | |||
(1) medial force with medial displacement<br>(2) longitudinal force with impaction and twisting<br>(3) lateral force with lateral displacement<br>(4) plantar force with plantar displacement<br>(5) crush injury | |||
<div class="row"> | |||
<div class="col-md-5"> [[Image:Bones of the foot.png|thumb|300px|Superior view of the foot, showing S-shaped curve of the Chopart joint]] </div> | |||
<div class="col-md-5">{{#ev:youtube|LzkRdkxkY6o|250}} <div class="text-right"><ref> Medical Diagnostic Imaging University of Sharjah. Chopart fracture-dislocations. Available from: http://www.youtube.com/watch?v=LzkRdkxkY6o[last accessed 20/04/22]</ref></div></div> | |||
</div> | |||
== Characteristics == | |||
Chopart joint dislocations and especially fracture-dislocations are still problematic in both diagnosis (they are missed or misdiagnosed in up to 41% of cases<ref name="p4" />) as well as treatment, thus resulting in a high degree of long-term morbidity.<ref name="p3" /> Isolated midtarsal dislocations are rare because of the close proximity of the midtarsal to subtalar and [[Lisfranc]] joints.<ref name="p6">Ip, K.Y., & Lui, T.H. (2006). Journal of Orthopaedic Surgery, 14(3), 357-359. 11 november, 2011. http://www.josonline.org/pdf/v14i3p357.pdf B</ref> | |||
Crush injuries of the foot often cause gross soft tissue damage and have very high rates of deep infection.<ref name="p5" /> | |||
< | The symptoms and signs of a Chopart fracture-dislocation are:<ref name="p9">Bahr, R., & Maehlum, S. (2004). Clinical Guide to Sports Injuries. Oslo: Human Kinetics.</ref> | ||
1) abnormal position of the forefoot to medial direction | |||
2) swelling of the dorsum of foot | |||
3) pain in the midtarsal region when it gets strained | |||
== | == Diagnosis == | ||
Injuries involving the Chopart joint complex are rare and frequently missed or misdiagnosed.<ref name="p4" /> Dislocation is often combined with fracture in these areas.<ref name="p9" /> Serious injuries may present in a subtle manner and are often misdiagnosed as a sprain. Small [http://www.physio-pedia.com/index.php5?title=Avulsion_Fractures_of_the_Ankle avulsion fractures] of the navicular and cuboid may be misdiagnosed as a simple avulsion when in fact they represent a more severe midfoot injury. A high index of suspicion is required.<ref name="p7">Makwana, K.N., & Van Liefland, M.R. (2005). Injuries of the midfoot [electronic version]. Current Orthopaedics, Vol. 19, No. 3, 231-242. A</ref> | |||
For the initial diagnosis, x-rays in three views (dorsoplantar, lateral and oblique) are recommended.<ref name="p3" /> In case of a present injury or in doubt, a [[CT Scans|CT scan]] or [[MRI Scans|MRI]] should be performed.<ref name="p0">Frink, M., Geerling, J., Hildebrand, F., Knobloch, K., Zech, S., Droste, P., …, Richter, M. (2006). Etiology, treatment and long-term results of isolated midfoot fractures [electronic version]. Foot and Ankle Surgery, Vol. 12, 121-125. A</ref> Knowledge of the exact radiographic projections is essential for making the correct diagnosis. For preoperative planning, the routine use of CT scanning is suggested. In any case of isolated navicular or cuboid compression fractures a corresponding ligamentous injury to the other side of the mid-tarsal joint has to be ruled out by stress films.<ref name="p8">Rammelt, S., Biewener, A., Grass, R., & Zwipp, H. (2004). Diagnostik und Therapie von Chopart-Luxationsfrakturen [electronic version]. Aktuelle Traumatologie Y, Vol. 34, No. 1, 16-25. A</ref> | |||
Furthermore the examination of the foot should include an evaluation of the patient's gait and extra attention should be paid to malalignment and swelling of the foot. | |||
< | {{#ev:youtube|KYy0p-xZzoU|250}} <div class="row"><div class="col-md-6 col-md-offset-3"><div class="text-right"><ref>RadioGraphics. Normal Anatomy and Traumatic Injury of the Midtarsal (Chopart) Joint Complex: An Imaging Primer. Available from: http://www.youtube.com/watch?v=KYy0p-xZzoU[last accessed 20/04/22]</ref></div></div></div> | ||
== | == Treatment == | ||
'''''Medical Management''' ''<br>A nonoperative treatment is used in non-dislocated or minimally dislocated fractures. Closed reduction is the most known non-operative treatment. After closed reduction, a rigid leg cast for 6 to 8 weeks with partial weight-bearing is recommended.<ref name="p4" /> Medication to prevent deep venous thrombosis is commonly given to patients, treated with a short leg cast with reduced weight bearing status.<ref name="p3" /> Though external fixation is a useful tool for the treatment of complex foot injuries, it is often associated with problematic residual stiffness of the foot and ankle.<ref name="p1" /><ref name="p4" /> | |||
Open reduction should be considered if closed reduction could not achieve the correct anatomic alignment.<ref name="p0" /> | |||
The | The aim of treatment of a Chopart fracture or dislocation should be reconstruction of the medial and lateral foot arch, and achieving congruent joint surfaces and ligamentous stability. Attention should be paid to the talonavicular joint because it is essential for satisfactory function of the ankle. Traditionally, open reduction improves outcome in Chopart fracture-dislocations and complex midfoot fractures, because ligamentous structures can be repaired and joint surfaces can be reconstructed.<ref name="p4" /> | ||
'''''Physiotherapy''''' | |||
Physiotherapy intervention should begin as soon as possible. Because the injured area will be immobilised for a period of weeks, the role of the physiotherapist is to educate and facilitate the patient in; | |||
* maintaining surrounding muscular strength and range of motion | |||
* maintaining functional independence as much as possible | |||
* preventing secondary complications | |||
* effective cast care | |||
* mobility progression as appropriate | |||
Following the immobilisation period, permitted physiotherapy interventions are usually guided by the treating orthopaedic surgeon. Common types of rehabilitation include;<ref name="p9" /> | |||
< | * techniques to reduce edema | ||
* strengthening exercises | |||
* static and dynamic flexibility exercises | |||
* gait training and weight-bearing progression | |||
* proprioceptive training | |||
* return-to-sport specific preparation<sup> </sup> | |||
== Prognosis | == Prognosis == | ||
Midfoot injuries have a high rate of mid and long-term morbidity. | Midfoot injuries have a high rate of mid- and long-term morbidity. This is because of the crucial role of the midfoot in the balance and stability of the foot. A fracture-dislocation of a midfoot bone results in a higher morbidity and greater functional impairment than an isolated midfoot fracture.<ref name="p3" /><ref name="p4" /><ref name="p5" /> | ||
The prognosis is good | The prognosis is improved by achieving good joint congruency post-reduction. If the injury does not result in chronic subluxation, the patient is mobilized earlier. If the injury results in chronic subluxation, the patient will often develop chronic pain exacerbated by loading and osteoarthritis will develop in the involved joints.<ref name="p9" /> | ||
< | Polytrauma patients, open injuries and the occurrence of compartment syndrome have been identified as significant variables that worsen final outcome after midfoot fractures and dislocation.<ref name="p4" /> | ||
Due to risk of developing post-traumatic arthrosis, long-term follow-up evaluation is an important aspect of the management of patients who have sustained dislocation of the mid tarsal joint.<ref name="p1" /> | |||
< | |||
== References == | |||
<references /> | <references /> | ||
[[Category:Foot]][[Category:Musculoskeletal/Orthopaedics|Orthopaedics]][[Category: | [[Category:Foot]] | ||
[[Category:Musculoskeletal/Orthopaedics|Orthopaedics]] | |||
[[Category:Conditions]] | |||
[[Category:Foot - Conditions]] | |||
[[Category:Primary Contact]] | |||
[[Category:Sports Medicine]] | |||
[[Category:Sports Injuries]] | |||
[[Category:Fractures]] | |||
Latest revision as of 04:38, 21 April 2022
Original Editor Zoë Vaes
Top Contributors - Laura Ritchie, Oyemi Sillo, Kim Jackson, Claire Knott, Admin, WikiSysop, Zoë Vaes, Wanda van Niekerk and 127.0.0.1Definition/Description[edit | edit source]
A Chopart fracture-dislocation is a dislocation of the mid-tarsal joints of the foot, often with associated fractures of the calcaneus, cuboid and navicular bone.
Clinically Relevant Anatomy[edit | edit source]
The transverse tarsal joint is also called the midtarsal joint and is referred to as Chopart’s joint. The midtarsal joint is composed of the talonavicular and calcaneocuboid joints.[1] The bones which form the Chopart joint are the talus and calcaneus proximally, and the navicular and cuboid bone distally. When the foot skeleton is viewed from above, the joint line of the transverse tarsal articulation has the shape of an 'S'.[2]
Epidemiology / Etiology[edit | edit source]
Among the uncommon midfoot injuries, Chopart joint dislocations or fracture-dislocations are the most severe injuries.[3] Chopart fracture-dislocations are caused most commonly by motor vehicle accidents and falls from a height. Avulsion fractures localized to the midfoot are typically caused by low-energy trauma e.g. sprain or sports injuries. Concomitant fractures occur in approximately 75% to 90% of Chopart injuries, and only 10% to 25% of Chopart dislocations are pure ligamentous injuries.[4] Injuries with a combined Chopart and Lisfranc fracture-dislocation are often part of so called "crush" injuries of the foot.[5]
Main and Jowet classified midtarsal joint injuries into five groups, according to the direction of the deforming force and the resulting displacement of the forefoot:[1]
(1) medial force with medial displacement
(2) longitudinal force with impaction and twisting
(3) lateral force with lateral displacement
(4) plantar force with plantar displacement
(5) crush injury
Characteristics[edit | edit source]
Chopart joint dislocations and especially fracture-dislocations are still problematic in both diagnosis (they are missed or misdiagnosed in up to 41% of cases[4]) as well as treatment, thus resulting in a high degree of long-term morbidity.[3] Isolated midtarsal dislocations are rare because of the close proximity of the midtarsal to subtalar and Lisfranc joints.[7]
Crush injuries of the foot often cause gross soft tissue damage and have very high rates of deep infection.[5]
The symptoms and signs of a Chopart fracture-dislocation are:[8]
1) abnormal position of the forefoot to medial direction
2) swelling of the dorsum of foot
3) pain in the midtarsal region when it gets strained
Diagnosis[edit | edit source]
Injuries involving the Chopart joint complex are rare and frequently missed or misdiagnosed.[4] Dislocation is often combined with fracture in these areas.[8] Serious injuries may present in a subtle manner and are often misdiagnosed as a sprain. Small avulsion fractures of the navicular and cuboid may be misdiagnosed as a simple avulsion when in fact they represent a more severe midfoot injury. A high index of suspicion is required.[9]
For the initial diagnosis, x-rays in three views (dorsoplantar, lateral and oblique) are recommended.[3] In case of a present injury or in doubt, a CT scan or MRI should be performed.[10] Knowledge of the exact radiographic projections is essential for making the correct diagnosis. For preoperative planning, the routine use of CT scanning is suggested. In any case of isolated navicular or cuboid compression fractures a corresponding ligamentous injury to the other side of the mid-tarsal joint has to be ruled out by stress films.[11]
Furthermore the examination of the foot should include an evaluation of the patient's gait and extra attention should be paid to malalignment and swelling of the foot.
Treatment[edit | edit source]
Medical Management
A nonoperative treatment is used in non-dislocated or minimally dislocated fractures. Closed reduction is the most known non-operative treatment. After closed reduction, a rigid leg cast for 6 to 8 weeks with partial weight-bearing is recommended.[4] Medication to prevent deep venous thrombosis is commonly given to patients, treated with a short leg cast with reduced weight bearing status.[3] Though external fixation is a useful tool for the treatment of complex foot injuries, it is often associated with problematic residual stiffness of the foot and ankle.[1][4]
Open reduction should be considered if closed reduction could not achieve the correct anatomic alignment.[10]
The aim of treatment of a Chopart fracture or dislocation should be reconstruction of the medial and lateral foot arch, and achieving congruent joint surfaces and ligamentous stability. Attention should be paid to the talonavicular joint because it is essential for satisfactory function of the ankle. Traditionally, open reduction improves outcome in Chopart fracture-dislocations and complex midfoot fractures, because ligamentous structures can be repaired and joint surfaces can be reconstructed.[4]
Physiotherapy
Physiotherapy intervention should begin as soon as possible. Because the injured area will be immobilised for a period of weeks, the role of the physiotherapist is to educate and facilitate the patient in;
- maintaining surrounding muscular strength and range of motion
- maintaining functional independence as much as possible
- preventing secondary complications
- effective cast care
- mobility progression as appropriate
Following the immobilisation period, permitted physiotherapy interventions are usually guided by the treating orthopaedic surgeon. Common types of rehabilitation include;[8]
- techniques to reduce edema
- strengthening exercises
- static and dynamic flexibility exercises
- gait training and weight-bearing progression
- proprioceptive training
- return-to-sport specific preparation
Prognosis[edit | edit source]
Midfoot injuries have a high rate of mid- and long-term morbidity. This is because of the crucial role of the midfoot in the balance and stability of the foot. A fracture-dislocation of a midfoot bone results in a higher morbidity and greater functional impairment than an isolated midfoot fracture.[3][4][5]
The prognosis is improved by achieving good joint congruency post-reduction. If the injury does not result in chronic subluxation, the patient is mobilized earlier. If the injury results in chronic subluxation, the patient will often develop chronic pain exacerbated by loading and osteoarthritis will develop in the involved joints.[8]
Polytrauma patients, open injuries and the occurrence of compartment syndrome have been identified as significant variables that worsen final outcome after midfoot fractures and dislocation.[4]
Due to risk of developing post-traumatic arthrosis, long-term follow-up evaluation is an important aspect of the management of patients who have sustained dislocation of the mid tarsal joint.[1]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Puthezhath, K., Veluthedath, R., Kumaran, C.M., & Patinharayil, G. (2009). Acute Isolated Dorsal Midtarsal (Chopart's) Dislocation: A Case Report [electronic version]. The Journal of Foot and Ankle Surgery, Vol. 48, No.4 , 462-465. B
- ↑ Signe Brunnstrom, M.A. (1975). Clinical Kinesiology. Philadelphia: F.A. Davis Company.
- ↑ 3.0 3.1 3.2 3.3 3.4 Richter, M., Thermann, H., Huefner, T., Schmidt, U., Goesling, T., & Krettek, C. (2004). Foot & Ankle International, Vol 25., No.5, 340-348. 5 november, 2011. http://www.krankenhaus-rummelsberg.de/uploads/tx_templavoila/chopart.pdf
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 Van Dorp, K.B., De Vries, M.R., Van der Elst, M., & Schepers, T. (2010). Chopart Joint Injury: A Study of Outcome and Morbidity [electronic version]. The Journal of Foot and Ankle Surgery, Vol. 49, No. 6, 541-545. C
- ↑ 5.0 5.1 5.2 Richter, M., Wippermann, B., Krettek, C., Schratt, H.E., Hufner, T., & Thermann, H. (2001). Foot & Ankle International, Vol. 22, No. 5, 392-379. 5 november, 2011. http://olc.metrohealth.org/SubSpecialties/Trauma/Media/Other/Fractures%20and%20fracture-dislocations%20of%20the%20midfoot,%20occurrence,%20causes,%20long-term%20results.pdf A
- ↑ Medical Diagnostic Imaging University of Sharjah. Chopart fracture-dislocations. Available from: http://www.youtube.com/watch?v=LzkRdkxkY6o[last accessed 20/04/22]
- ↑ Ip, K.Y., & Lui, T.H. (2006). Journal of Orthopaedic Surgery, 14(3), 357-359. 11 november, 2011. http://www.josonline.org/pdf/v14i3p357.pdf B
- ↑ 8.0 8.1 8.2 8.3 Bahr, R., & Maehlum, S. (2004). Clinical Guide to Sports Injuries. Oslo: Human Kinetics.
- ↑ Makwana, K.N., & Van Liefland, M.R. (2005). Injuries of the midfoot [electronic version]. Current Orthopaedics, Vol. 19, No. 3, 231-242. A
- ↑ 10.0 10.1 Frink, M., Geerling, J., Hildebrand, F., Knobloch, K., Zech, S., Droste, P., …, Richter, M. (2006). Etiology, treatment and long-term results of isolated midfoot fractures [electronic version]. Foot and Ankle Surgery, Vol. 12, 121-125. A
- ↑ Rammelt, S., Biewener, A., Grass, R., & Zwipp, H. (2004). Diagnostik und Therapie von Chopart-Luxationsfrakturen [electronic version]. Aktuelle Traumatologie Y, Vol. 34, No. 1, 16-25. A
- ↑ RadioGraphics. Normal Anatomy and Traumatic Injury of the Midtarsal (Chopart) Joint Complex: An Imaging Primer. Available from: http://www.youtube.com/watch?v=KYy0p-xZzoU[last accessed 20/04/22]