Characteristics and Identification of Wound Types: Arterial and Venous Insufficiency Ulcers: Difference between revisions
No edit summary |
No edit summary |
||
| (38 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Stacy Schiurring|Stacy Schiurring]] based on the course by [https://members.physio-pedia.com/instructor/dana-palmer// Dana Palmer]<br> | <div class="editorbox"> '''Original Editor '''- [[User:Stacy Schiurring|Stacy Schiurring]] based on the course by [https://members.physio-pedia.com/instructor/dana-palmer// Dana Palmer]<br> | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
This article provides information for those rehabilitation professionals who are new to wound care or have been away from the | This article provides information for those rehabilitation professionals who are new to wound care or have been away from the practice and need a review of wound type identification. This article will not go into specifics on wound assessment or treatment. | ||
The five most common types of chronic wounds include (1) arterial ulcers, (2) venous insufficiency ulcers or venous wounds, (3) neuropathic wounds, or diabetic foot ulcers (DFUs), (4) pressure injuries, formerly known as pressure ulcers, and (5) non-healing surgical wounds. | The five most common types of chronic wounds include (1) arterial ulcers, (2) venous insufficiency ulcers or venous wounds, (3) neuropathic wounds, or diabetic foot ulcers (DFUs), (4) pressure injuries, formerly known as pressure ulcers, and (5) non-healing surgical wounds. | ||
| Line 10: | Line 10: | ||
The terms ulcer and wound will be used interchangeably throughout this article.<ref name=":0">Palmer, D. Characteristics and Identification of Wound Types. Physiotherapy Wound Care Programme. Plus. 2022.</ref> | The terms ulcer and wound will be used interchangeably throughout this article.<ref name=":0">Palmer, D. Characteristics and Identification of Wound Types. Physiotherapy Wound Care Programme. Plus. 2022.</ref> | ||
Due to the large amount of information to be presented, this topic has been divided into three separate pages. | Due to the large amount of information to be presented, this topic has been divided into three separate pages. This page will cover arterial and venous insufficiency ulcers. To learn more about neuropathic wounds, please see [[Characteristics and Identification of Wound Types: Neuropathic Wounds|this article]]. To learn more about pressure injuries and non-healing surgical wounds, please see [https://www.physio-pedia.com/Characteristics_and_Identification_of_Wound_Types:_Pressure_Injuries_and_Non-healing_Surgical_Wounds this article]. | ||
== Arterial Ulcers == | == Arterial Ulcers == | ||
<blockquote>'''Arterial ulcers''' ( | <blockquote>'''Arterial ulcers''' (also known as ischaemic ulcers) are caused by poor tissue profusion to the lower extremities. This impaired blood supply causes nutrient and oxygen deprivation and results in tissue hypoxia and cell death. This leads to wound formation in the overlying skin and tissues. Additionally, decreased blood supply can impair the body's ability to heal, allowing minor scrapes or cuts to develop into ulcers.<ref>Wound Source. Arterial Ulcers. Available from: https://www.woundsource.com/patientcondition/arterial-ulcers (accessed 10/09/2022).</ref> </blockquote> | ||
* Arterial wounds account for about 10 to 20% of lower extremity ulcers | * Arterial wounds account for about 10 to 20% of lower extremity ulcers | ||
* Arterial ulcers are the result of | * Arterial ulcers are the result of peripheral arterial disease<ref name=":0" /> | ||
=== Peripheral Arterial Disease === | |||
<blockquote>'''Peripheral arterial disease''' (PAD) is caused by the narrowing or blockage of the arteries, most commonly due to [[atherosclerosis]]. PAD can occur in any artery, but it is more common in the legs than the arms.<ref name=":2">Centers for Disease Control and Prevention. Peripheral Arterial Disease (PAD). Available from: https://www.cdc.gov/heartdisease/PAD.htm (accessed 10/09/2022).</ref> 40% of people with PAD are asymptomatic. Knowing what to look for may save a limb or a life.<ref name=":0" /> </blockquote> | |||
* PAD occurs along a spectrum and progresses incrementally | * PAD occurs along a spectrum and progresses incrementally | ||
* It is asymptomatic until it reaches a threshold where the body is no longer able to compensate for the reduced blood flow, which can be when the artery is 60% or more occluded<ref name=":0" /> | * It is asymptomatic until it reaches a threshold where the body is no longer able to compensate for the reduced blood flow, which can be when the artery is 60% or more occluded<ref name=":0" /> | ||
To learn more about PAD and its signs and symptoms, please read [[Peripheral Arterial Disease|this article]]. | |||
==== PAD Screening ==== | ==== PAD Screening ==== | ||
Patients with PAD have a higher risk of asymptomatic coronary artery disease | Patients with PAD have a higher risk of asymptomatic coronary artery disease and are at a greater risk of cardiovascular events. Therefore, it is important for the rehabilitation professional to be able to screen for PAD. As rehabilitation professionals often spend large amounts of time with their patients and get to know them well, they may be the first healthcare professional to note the possibility of PAD. Simple and efficient bedside screens allow the rehabilitation professional to gather information and initiate the appropriate referral.<ref name=":0" /> | ||
{| class="wikitable" | {| class="wikitable" | ||
|+ | |+ | ||
If these screening tests are positive, the patient should receive an [[Ankle-Brachial Index|ankle-brachial index test]] (ABI).<ref name=":0" /> It assesses the severity of arterial insufficiency of arterial narrowing during walking. ABI is measured by dividing the ankle systolic pressure by brachial systolic pressure. Normal ABI is between 0.90 and 1.30. A lower score may indicate PAD, a higher score may be a sign of arterial calcification.<ref>Crawford F, Welch K, Andras A, Chappell FM. [https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD010680.pub2/full Ankle brachial index for the diagnosis of lower limb peripheral arterial disease]. Cochrane Database of Systematic Reviews. 2016(9).</ref> | |||
! | ! | ||
!'''Screening reasoning''' | !'''Screening reasoning''' | ||
!'''Procedure''' | !'''Procedure''' | ||
!'''Test | !'''Test example''' | ||
(click | (click to enlarge) | ||
|- | |- | ||
|'''[[Dorsalis Pedis Artery#Palpation Dorsalis Pedis Artery Pulse|Dorsalis pedis pulse]]''' | |'''[[Dorsalis Pedis Artery#Palpation Dorsalis Pedis Artery Pulse|Dorsalis pedis pulse]]''' | ||
|The dorsalis pedis artery is the supplier of blood to the foot. A weak dorsalis pedis pulse may signify an underlying circulatory condition such as PAD.<ref>Verywell Health. Anatomy of the Dorsalis Pedis Artery. Available from: https://www.verywellhealth.com/dorsalis-pedis-artery-5097663 (accessed 11/09/2022).</ref> | |The dorsalis pedis artery is the supplier of blood to the foot. A weak dorsalis pedis pulse may signify an underlying circulatory condition such as PAD.<ref>Verywell Health. Anatomy of the Dorsalis Pedis Artery. Available from: https://www.verywellhealth.com/dorsalis-pedis-artery-5097663 (accessed 11/09/2022).</ref> | ||
| | | | ||
* | * Possible to visualise this pulse | ||
* | * Locate palpation point by asking the patient to lift their great toe, the artery is located just lateral to this tendon | ||
* | * Pulse is located just past the midfoot towards the ankle region | ||
* | * Document which grading scale is being used<ref name=":0" /> ''See table below for details'' | ||
|[[File:Dorsalis_pedis_pulse.jpeg|alt=|frameless|200x200px]] | |[[File:Dorsalis_pedis_pulse.jpeg|alt=|frameless|200x200px]] | ||
|- | |- | ||
|'''Posterior tibial artery pulse''' | |'''Posterior tibial artery pulse''' | ||
|The posterior tibial artery provides blood flow to the posterior compartment of the leg. | |The posterior tibial artery provides blood flow to the posterior compartment of the leg. A weak posterior tibial pulse may signify PAD or compartment syndrome.<ref>Verywell Health. The Anatomy of the Posterior Tibial Artery. Available from: https://www.verywellhealth.com/posterior-tibial-artery-anatomy-4707725#:~:text=The%20posterior%20tibial%20artery%20plays,connects%20to%20the%20femoral%20artery. (accessed 11/09/2022).</ref> | ||
| | | | ||
* | * Locate the palpation point midway between the medial malleolus and the Achilles tendon | ||
* | * Document which grading scale is being used<ref name=":0" />''See table below for details'' | ||
|[[File:Posterior_tibial_artery_pulse.jpeg|alt=|frameless|200x200px]] | |[[File:Posterior_tibial_artery_pulse.jpeg|alt=|frameless|200x200px]] | ||
|- | |- | ||
| Line 55: | Line 55: | ||
(CRT) | (CRT) | ||
| | | | ||
* CRT is a physical | * CRT is a physical examination technique which provides a quick and reliable assessment regarding the adequacy of peripheral perfusion in both adults and children.<ref>McGuire D, Gotlib A, King J. [https://www.ncbi.nlm.nih.gov/books/NBK557753/#_NBK557753_pubdet_ Capillary Refill Time]. InStatPearls [Internet] 2022 Apr 21. StatPearls Publishing.</ref> | ||
* | * Beneficial to perform when the patient has absent or diminished posterior tibial or dorsalis pedis pulses | ||
| | | | ||
* | * Provide light compression at the end of a digit or the skin just distal to a wound or area of concern until the colour disappears (blanches) | ||
* | * Release the pressure and count how many seconds until the skin returns to its original colour | ||
* | * A normal CRT is less than three seconds<ref name=":0" /> | ||
|[[File:Capillary refill test.jpeg|frameless|200x200px]] | |[[File:Capillary refill test.jpeg|frameless|200x200px]] | ||
|- | |- | ||
|'''Rubor dependency test''' | |'''Rubor dependency test'''<ref name=":6">Hamm, RL. Text and atlas of wound diagnosis and treatment, (2nd ed). 2019. McGraw Hill.126044046X</ref> | ||
| | | | ||
* Bedside assessment to assess for PAD | |||
* Dependent rubor is a fiery-red to dusky-red colouration to the skin when the leg is in a dependent position, but not when it’s elevated above the heart<ref name=":1">Woundcare Advisor. What’s causing your patient’s lower-extremity redness? Available from: https://woundcareadvisor.com/whats-causing-your-patients-lower-extremity-redness_vol2-no4/#:~:text=Dependent%20rubor%20is%20a%20fiery,is%20cool%20to%20the%20touch. (accessed 11/09/2022).</ref> | |||
|''Please read the special topic box below for more information on this test'' | |||
* The limb is elevated to 60 degrees from horizontal for 60 seconds | |||
* Examine the sole of the foot and assess for pallor. PAD causes the soles to change from pink to pale in people with fair skin and to grey or ashen in people with dark skin | |||
* Pallor within 25 seconds of leg elevation indicates severe occlusive disease. The more quickly the pallor appears, the worse the PAD | |||
* Then it is moved to a dependent position by assisting the patient into a sitting position | |||
* A limb with normal profusion will return to a healthy colour within about 15 seconds of being lowered<ref name=":1" /><ref name=":0" /> | |||
|''Please view the video below for an example of how to perform this test.'' | |||
|} | |} | ||
# | # | ||
{| class="wikitable" | |||
{{#ev:youtube| eJWbJ4pzX18 |500}}<ref>YouTube. Capillary Refill & Rubor of Dependency - Vascular Test | Klose Training. Available from: https://www.youtube.com/watch?v=eJWbJ4pzX18 [last accessed 11/09/2022]</ref> | |+ | ||
Two options of grading scales to measure pulse amplitude. | |||
!'''Grading Scale''' | |||
!'''Description''' | |||
|- | |||
|'''3-Point Scale'''<ref>Lapum JL, Verkuyl M, Garcia W. Vital Sign Measurement Across the Lifespan–1st Canadian Edition. OpenStax Anatomy and Physiology; 2017.</ref> | |||
|0 no palpable pulse | |||
1+ weak pulse | |||
2+ normal pulse | |||
3+ increased, full, bounding pulse | |||
|- | |||
|'''4-Point Scale'''<ref>Hill RD, Smith RB. [https://www.ncbi.nlm.nih.gov/books/NBK350/ Chapter 30: Examination of the extremities: pulses, bruits, and phlebitis]. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd ed. Boston, MA: Butterworths. 1990.</ref> | |||
|0 no palpable pulse | |||
1 + faint, but detectable pulse | |||
2 + suggesting a slightly more diminished pulse than normal | |||
3 + is a normal pulse | |||
4 + bounding pulse | |||
|} | |||
# | |||
The following short video includes a demonstration of how to perform the CRT and rubor dependency test. | |||
{{#ev:youtube| eJWbJ4pzX18 |500}}<ref>YouTube. Capillary Refill & Rubor of Dependency - Vascular Test | Klose Training. Available from: https://www.youtube.com/watch?v=eJWbJ4pzX18 [last accessed 11/09/2022]</ref><blockquote>'''Special topic:''' What is dependent rubor and how is it tested at the bedside?<ref name=":6" /> | |||
'''Dependent rubor''' (also known as erythromelalgia chronic rubor, reactionary rubor, induced rubor, and hyperemic response) is a physiological sign associated with PVD.<ref name=":4">Wright WF, Rajachandran M. [https://www.degruyter.com/document/doi/10.7556/jaoa.2017.023/html?lang=de Buerger Test for erythromelalgia revisited]. Journal of Osteopathic Medicine. 2017 Feb 1;117(2):124-6.</ref> It is a dusky-red discolourisation of the lower leg and foot which occurs when the extremity is placed in a dependent position below the heart. It occurs because the arterioles in that extremity are maximally dilated as a compensatory response to ischaemia. The arterioles fail to constrict despite the hydrostatic pressure being high when the extremity is in the dependent position, resulting in red discolourisation.<ref>Ijaz S, Mazhar M, Ali I, Latif F. [https://shmabstracts.org/abstract/every-red-is-not-cellulitis-dependent-rubor-rare-but-classical-finding-of-severe-arterial-insufficiency/ Every red is not cellulitis: dependent rubor rare but classical finding of severe arterial insufficiency]. Hospital Medicine 2018; 2018 April 8-11; Orlando, FL, USA.</ref> | |||
Moving a healthy foot into a dependent position decreases capillary blood flow, and elevation produces no changes in blood flow. However, the same positioning in patients with PVD increases capillary blood flow in the dependent position and decreases capillary blood flow with elevation.<ref name=":4" /> This change in physiology is the basis of the rubor dependency testing. | |||
'''The Buerger test is classically performed by'': | |||
# Placing the patient in supine | |||
# Elevating the leg to 90 degrees to the horizontal plane until pallor is noted | |||
# The leg is then slowly lowered, and the angle at which colour returns is recorded. This angle is known as the angle of circulatory sufficiency. | |||
'''The rubor dependency test (variation of the Buerger test) is performed by'': | |||
# Placing the patient in supine | |||
# Elevating the leg to 60 degrees from the horizontal plane for 2 minutes, note any appearance of pallor | |||
# The leg is then moved into the dependent position for another 2 minutes, note any change in colour. The dependent positioning of the leg can be achieved by asking the patient to sit at the bed of the examination surface with legs dangling over the side.<ref name=":5">Bartholomew JR. [https://journals.sagepub.com/doi/full/10.1177/1358863X211022807 From the Masters: Lessons learned about the vascular medicine history and physical examination from the past and present]. Vascular Medicine. 2021 Aug;26(4):361-6.</ref> | |||
Limb pallor during this test indicates peripheral artery disease, as does rubor in the dependent position.<ref name=":4" /> | |||
'''Other modifications to this examination found in the literature include''': | |||
* The angle of elevation of the leg when observing for pallor<ref name=":4" /><ref name=":5" /> | |||
* Addition of exercise, such as ankle pumps, when the leg is elevated<ref>Insall RL, Davies RJ, Prout WG. [https://journals.sagepub.com/doi/pdf/10.1177/014107688908201209 Significance of Buerger's test in the assessment of lower limb ischaemia]. Journal of the Royal Society of Medicine. 1989 Dec;82(12):729-31.</ref> | |||
* With legs elevated above the level of the heart, gently ‘milk’ the colour from the patient's feet. Persistent pallor after 30 seconds suggests severe PAD with this technique.<ref name=":5" /> | |||
According to Wright et al.,<ref name=":4" /> the angle which results in pallor in the leg is likely to be important in identifying the extent of circulatory disturbance and prognosis. However, at the time of publication of Wright and colleague's article, no studies had been completed that correlate specific angles to the degree of arterial occlusion.<ref name=":4" /> For example, a textbook published in 2019 teaches that elevating an ischaemic leg 15-30 degrees for 30-60 seconds is enough to cause pallor in the suspected limb.<ref>Sacchidanand S, Eswari L, Shilpa K. Leg Ulcers: Diagnosis & Management. Jaypee Brothers Medical Publishers; 2019 Sep 30.</ref> Further research may provide insight into the degree of elevation and its relationship to the severity of arterial occlusion. This would provide rehabilitation professionals with a stronger bedside assessment tool to aid in the creation of effective plans of care and when to initiate a medical referral. | |||
Research has shown that the "Buerger test may be highly sensitive for detecting arterial occlusions below the popliteal fossa but is not specific for arterial occlusion above the popliteal fossa."<ref name=":4" /> This strengthens the case that a positive Buerger test indicates probable PVD.<ref name=":4" /></blockquote>Other tests that may be considered are the (1) toe-brachial index, (2) transcutaneous oxygen pressure, or (3) segmental perfusion pressure. The gold standard to diagnose PAD is contrast angiography, which is an invasive exam.<ref name=":0" /> | |||
==== PAD Risk Factors ==== | |||
'''Risk factors for PAD and arterial ulcers:''' | |||
# '''Smoking'''. Cigarette smoking doubles the risk of PAD. The risk increases cumulatively with the number of cigarettes smoked and the number of years spent smoking.<ref name=":0" /> | |||
# '''Age above 60 years''' | |||
#* 5-10% of those aged 50 to 80 years has PAD. | |||
#* 20-30% of those over 80 years have PAD.<ref name=":0" /> | |||
# '''Diabetes'''. The risk of PAD in patients with diabetes is increased by two to three times.<ref name=":0" /> | |||
# '''Hypertension''' | |||
# '''High cholesterol''' | |||
# '''Atherosclerosis.''' However, it is important to note that not all PAD is caused by atherosclerosis.<ref name=":2" /> Health screening and referral to the appropriate healthcare provider can assist with a formal diagnosis. | |||
# '''Sedentary lifestyle''' | |||
# '''Family history''' | |||
Both sexes are affected by PAD. However, biological males are more likely to present with [[claudication]] symptoms and biological females are more likely to be asymptomatic.<ref name=":0" /> | |||
==== PAD Differential Diagnosis ==== | |||
Spinal stenosis, a condition commonly treated in rehabilitation clinics, can present with symptoms similar to peripheral arterial disease. It is important to be able to differentiate between the symptoms of these conditions, but also to be aware that they can both occur simultaneously.<ref name=":0" /> | |||
* '''Ischaemic claudication pain associated with PAD:'''<ref name=":0" /> | |||
** In the early stages, can be relieved with rest. | |||
** In the later stages, pain is present at rest and does not change except when the limb is placed in a dependent position. | |||
* '''Spinal stenosis claudication pain:'''<ref name=":0" /> | |||
** Typically relieved with a change in position that reduces the compression at the spine, such as moving from standing to sitting; sitting to lying; extension into flexion. | |||
* Looking at the other signs and symptoms of PAD will also help to differentiate between the two. | |||
=== Arterial Wound Characteristics === | |||
* Occur on the lower third of the leg. | |||
* Often seen on the lateral side and distally, ie: the mid-tibia region, the lateral malleolus, the toes, the web spaces, and the heels. | |||
* Wound bed tends to be pale with well-defined edges or a punched out appearance. | |||
* Wound bed is typically dry and has minimal drainage. It usually does not bleed. | |||
* Necrotic tissue is common, especially black eschar. | |||
* The skin is pale, darkened, or cyanotic. | |||
* The area of skin around the wound is commonly shiny, brittle, and hairless. | |||
* May observe slow-growing, brittle, or rigid toenails. | |||
* The posterior tibial and/or dorsalis pedis pulses are diminished or absent. | |||
* The lower leg is often cool to the touch and muscle atrophy can be observed in the calves or feet. | |||
* Arterial wounds are typically quite painful, pain is often worse with elevation. In the later stages of PAD, pain at rest and burning in the toes and soles of the feet are common. | |||
<gallery> | |||
File:Arterial wound 1.jpeg | |||
File:Arterial wound 2.jpeg | |||
File:Arterial wound 3.jpeg | |||
File:Arterial wound 4.jpeg | |||
File:Arterial wound 1 DP.jpeg|''Used with kind permission from Dana Palmer, PT'' | |||
File:Arterial wound 2 DP.jpeg|''Used with kind permission from Dana Palmer, PT'' | |||
File:Arterial wound 3 DP.jpeg|''Used with kind permission from Dana Palmer, PT'' | |||
File:Arterial wound 4 DP.jpeg|''Used with kind permission from Dana Palmer, PT'' | |||
File:Arterial wound 5 DP.jpeg|''Used with kind permission from Dana Palmer, PT'' | |||
File:Arterial wound 6 DP.jpeg|''Used with kind permission from Dana Palmer, PT'' | |||
</gallery> | |||
'''Symptoms of PAD and arterial wounds:'''<ref name=":0" /> | |||
* Slow healing wounds | |||
* Feet usually feel "cold, tingly or numb" | |||
* Muscle cramping is common, especially with exercise or exertion in daily activities such as stair climbing | |||
'''How PAD pain can effect rehabilitation assessments:'''<ref name=":0" /> | |||
* Pain symptoms are often reported unilaterally. However, approximately 80% of patients have significant bilateral disease. If one side is more severe, it may be masking symptoms on the contralateral side. | |||
* Pain is commonly relieved with a dependency position which can result in oedema in the limb. This is significant for differential diagnosis with venous disease. | |||
* Ambulation tolerance is limited by pain, cramping, or weakness after a few blocks distance. Watch for expected patterns of pain improving with rest to differentiate from other types of walking pain. | |||
=== | === Arterial Wound Management === | ||
'''The three most important factors in arterial wound management:'''<ref name=":0" /> | |||
# '''Perfusion'''. Tissue perfusion needs to be restored as soon as possible and must be addressed before any wound healing can occur. Avoid compression and elevation in these patients. If screening tests indicate poor perfusion, the patient should receive an ankle-brachial index test and a referral back to a vascular specialist. | |||
# '''Smoking cessation'''. This is the largest modifiable risk factor for arterial ulcers. Smoking cessation has been shown to restore the tissue microenvironment and cellular functions within approximately four weeks time and continues the longer the individual can abstain from smoking. ''Please see additional resources section for more information.'' | |||
# '''Nutrition'''. In general, adequate hydration and reducing trans fats and inflammatory foods will all help to manage blood pressure, cholesterol, and inflammation.<ref name=":3">Hart MJ, Torres SJ, McNaughton SA, Milte CM. [https://nutritionj.biomedcentral.com/articles/10.1186/s12937-021-00674-9 Dietary patterns and associations with biomarkers of inflammation in adults: a systematic review of observational studies]. Nutrition journal. 2021 Dec;20(1):1-4.</ref> Ideally, each patient should work with a dietitian to develop a customised nutrition plan. | |||
== | == Venous Ulcers == | ||
<blockquote>'''Venous ulcers''' (also known as venous stasis ulcers, venous insufficiency ulcers, or varicose ulcers) are caused by malfunctioning valves in the veins which increase venous hypertension. This results in blood pooling and decreases the ability of the circulatory system to efficiently pump blood back towards to heart causing venous insufficiency. Blood pooling and venous hypertension also result in blood cells and proteins leaching out into the surrounding subcutaneous tissues, causing oedema and the eventual tissue breakdown and wound formation due to lack of oxygen and nutrients.<ref>Wound Source. Venous Ulcers. Available from: https://www.woundsource.com/patientcondition/venous-ulcers (accessed 10/14/2022).</ref></blockquote> | |||
* Venous ulcers are the most common type of chronic wound, accounting for more than 70% of all leg ulcers. | |||
* Approximately one-third of adults have venous insufficiency, the prevalence increases with age. | |||
* Chronic venous insufficiency (CVI) is approximately three times more common in biological females than biological males primarily due to the effect oestrogen and progesterone have on vein function. | |||
* Approximately 25% of patients with CVI will have concomitant arterial disease. Use the PAD screening tests listed above to screen for a mixed symptom presentation.<ref name=":0" /> | |||
=== Venous Wound Characteristics === | |||
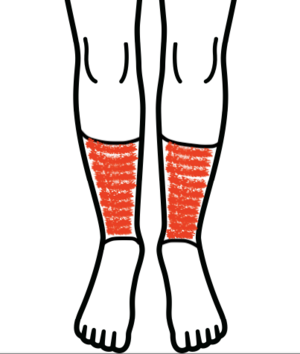
* [[File:Gaiter area.png|thumb|The gaiter area of the leg ]]Occur on the lower third of the leg in the gaiter area. | |||
* More common on the medial side of the leg. | |||
* Venous wounds tend to be shallow with uneven edges and a granular or a gelatinous fibrotic base. | |||
* Yellow slough may be seen, but black or brown eschar is rare. | |||
* Venous wounds tend to be wet due to the often copious amount of serous exudate which seeps from the wound and sometimes weeps from the surrounding skin. | |||
* Venous wounds have an insidious onset and are often proceeded by changes in skin colour and texture. The skin may appear inflamed, thickened, crusty, scaled, shiny or tight. | |||
* '''Stasis dermatitis''' may occur: redness is seen in lighter skin tones and a purple-grey or ashen tone is seen in darker skin tones. | |||
* '''Varicose veins''' | |||
* '''Haemosiderin staining''' may occur: brownish speckled staining of the skin. | |||
* '''Atrophie blanche''' may occur: whitish discolouration of the skin. This can be seen in the skin with healed ulcers or may be a precursor to future ulceration. | |||
* Pulses are present but can be difficult to palpate if the patient has severe oedema. | |||
* The lower leg is typically warm to the touch. | |||
* Venous wounds are less painful than arterial wounds, and patients often report feeling "aches" in their entire lower extremity. | |||
<gallery> | |||
File:Pitting oedema.jpeg|Pitting oedema | |||
File:Varicose vein BLE.jpeg|Varicose veins | |||
File:Haemosiderin staining.jpeg|Haemosiderin staining | |||
File:Venous wound.jpeg | |||
File:Venous wound 1.jpeg|''Used with kind permission from Dana Palmer, PT'' | |||
File:Venous wound 2.jpeg|''Used with kind permission from Dana Palmer, PT'' | |||
File:Venous wound 3.jpeg|''Used with kind permission from Dana Palmer, PT'' | |||
File:Venous wound 4.jpeg|''Used with kind permission from Dana Palmer, PT'' | |||
File:Venous wound 5.jpeg|''Used with kind permission from Dana Palmer, PT'' | |||
</gallery> | |||
'''Chronic oedema and venous wounds''':<ref name=":0" /> | |||
Chronic oedema is worse after prolonged standing. | * Common symptoms in CVI. | ||
* Chronic oedema is worse after prolonged standing. | |||
* Initially, oedema is pitting, meaning a finger intention will stay visible after pressing on the skin. | |||
* In more advanced disease, oedema may become firm and have a 'woody' consistency. This presents as a dark, discoloured, firm, nonpitting oedema. | |||
* Late stages of the disease may present with a 'champagne bottle' shape of the lower leg. | |||
* For differential diagnosis: CVI oedema is generally only observed below the knee, if it extends up into the thigh it is more likely to be due to [[lymphoedema]]. | |||
* For differential diagnosis: CVI oedema is also likely to be unilateral, if oedema is bilateral and equal, it is more likely due to medications or another systemic condition such as [[Congestive Heart Failure|congestive heart failure.]] | |||
'''Symptoms of CVI and venous ulcers:'''<ref name=":0" /> | |||
* Common for wounds to improve and regress multiple times. 60-70% of patients who have had a venous wound will have a recurrence within 10 years. | |||
* Aching or cramping in the leg. | |||
* Patient reports the leg feeling "heavy or tired". | |||
* Itching or tingling of the skin is common, especially with stasis dermatitis. | |||
* Discomfort is relieved with elevation and worsened with dependency or prolonged standing. | |||
* Frequent urination at night. | |||
* Achey lower legs. | |||
The | === CVI screening and examination === | ||
* Skin assessment: looking for visible varicose veins, oedema, and any skin changes that are commonly seen with CVI | |||
* Assess arterial circulation with palpation of the posterior tibial and dorsalis pedis pulses | |||
* If pulses are not palpable, check capillary refill. If it is intact, the lack of pulses is more likely due to venous oedema rather than arterial insufficiency occluding the vessels. | |||
* [[Brodie–Trendelenburg Test|Brodie-Trendelenberg's]] and Perthe's tests can be used clinically to test for venous backflow.<ref name=":0" /> ''Please see the additional resources section for optional reading about these tests.'' | |||
Please view the following optional video for a quick demonstration of a peripheral venous examination as performed by a medical doctor, including the Brodie-Trendelenburg and Perthe's tests. | |||
{{#ev:youtube| veeEgFHmz4M |500}}<ref>YouTube. Examination of the Peripheral Venous System. Available from: https://www.youtube.com/watch?v=veeEgFHmz4M [last accessed 14/09/2022]</ref> | |||
=== Venous Wound Management === | |||
'''The three most important factors for venous wound management:''' | |||
# '''Compression'''. Oedema management is vital for proper wound healing. Compression must be worn 24 hours a day and kept dry. For patients with an open wound, compression dressings are changed regularly as the circumference changes with oedema fluid loss. Once the wounds have healed and the oedema is stable, the limb should be measured for custom compression stockings. These should be worn all day when the patient's leg would be in a dependent position but can be removed for sleep. The patient may continue to use old compression stockings if they are in good shape and provide the appropriate amount of compression. Patients should not continue to wear compression stockings that have holes or runs. Stockings typically need to be replaced every six months. And if possible, the patient should have two pairs so that they have something to wear while one of them is being washed.<ref name=":0" /> Do not put compression stockings in the dryer. | |||
#* Prior to applying any compression, you need to ensure that the patient has adequate tissue perfusion and that the level of compression is appropriate for them. This is determined with ABI testing.<ref name=":0" /> | |||
# '''Nutrition'''. As with arterial ulcers, a patient with venous wounds will require adequate hydration and reduced intake of foods that can cause inflammation of the blood vessels.<ref name=":3" /> | |||
# '''Exercise'''. Encourage exercises that activate muscle pump action in the lower extremities to assist with venous return, examples include: a walking programme, bicycling, ankle pumps, ankle circumduction, ankle alphabet, heel-toe raises in both sitting and standing positions, and ankle rocker board exercises. Include soleus stretches and ankle mobility to optimise ankle joint range of motion. Whenever possible, combine exercises with supine positioning and elevate the legs above the level of the heart to have gravity assist with venous return.<ref name=":0" /> | |||
== Resources == | == Resources == | ||
* | '''Clinical resources for patient education''': | ||
* World Health Organization (WHO) resources for [https://www.who.int/activities/quitting-tobacco smoking cessation] | |||
'''Optional additional reading on Brodie-Trendelenberg and Perthes screening tests''': | |||
* Kim J, Richards S, Kent PJ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2503433/pdf/annrcse01625-0031.pdf Clinical examination of varicose veins--a validation study]. Annals of the Royal College of Surgeons of England. 2000 May;82(3):171. | |||
* Krishnan S, Nicholls SC. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3036279/ Chronic venous insufficiency: clinical assessment and patient selection]. InSeminars in Interventional Radiology 2005 Sep (Vol. 22, No. 03, pp. 169-177). Copyright© 2005 by Thieme Medical Publishers, Inc., 333 Seventh Avenue, New York, NY 10001, USA.. | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Course Pages]] | |||
[[Category:Integumentary System]] | |||
[[Category:Plus Content]] | |||
Latest revision as of 19:14, 12 October 2022
Top Contributors - Stacy Schiurring, Jess Bell and Tarina van der Stockt
Introduction[edit | edit source]
This article provides information for those rehabilitation professionals who are new to wound care or have been away from the practice and need a review of wound type identification. This article will not go into specifics on wound assessment or treatment.
The five most common types of chronic wounds include (1) arterial ulcers, (2) venous insufficiency ulcers or venous wounds, (3) neuropathic wounds, or diabetic foot ulcers (DFUs), (4) pressure injuries, formerly known as pressure ulcers, and (5) non-healing surgical wounds.
The terms ulcer and wound will be used interchangeably throughout this article.[1]
Due to the large amount of information to be presented, this topic has been divided into three separate pages. This page will cover arterial and venous insufficiency ulcers. To learn more about neuropathic wounds, please see this article. To learn more about pressure injuries and non-healing surgical wounds, please see this article.
Arterial Ulcers[edit | edit source]
Arterial ulcers (also known as ischaemic ulcers) are caused by poor tissue profusion to the lower extremities. This impaired blood supply causes nutrient and oxygen deprivation and results in tissue hypoxia and cell death. This leads to wound formation in the overlying skin and tissues. Additionally, decreased blood supply can impair the body's ability to heal, allowing minor scrapes or cuts to develop into ulcers.[2]
- Arterial wounds account for about 10 to 20% of lower extremity ulcers
- Arterial ulcers are the result of peripheral arterial disease[1]
Peripheral Arterial Disease[edit | edit source]
Peripheral arterial disease (PAD) is caused by the narrowing or blockage of the arteries, most commonly due to atherosclerosis. PAD can occur in any artery, but it is more common in the legs than the arms.[3] 40% of people with PAD are asymptomatic. Knowing what to look for may save a limb or a life.[1]
- PAD occurs along a spectrum and progresses incrementally
- It is asymptomatic until it reaches a threshold where the body is no longer able to compensate for the reduced blood flow, which can be when the artery is 60% or more occluded[1]
To learn more about PAD and its signs and symptoms, please read this article.
PAD Screening[edit | edit source]
Patients with PAD have a higher risk of asymptomatic coronary artery disease and are at a greater risk of cardiovascular events. Therefore, it is important for the rehabilitation professional to be able to screen for PAD. As rehabilitation professionals often spend large amounts of time with their patients and get to know them well, they may be the first healthcare professional to note the possibility of PAD. Simple and efficient bedside screens allow the rehabilitation professional to gather information and initiate the appropriate referral.[1]
| Screening reasoning | Procedure | Test example
(click to enlarge) | |
|---|---|---|---|
| Dorsalis pedis pulse | The dorsalis pedis artery is the supplier of blood to the foot. A weak dorsalis pedis pulse may signify an underlying circulatory condition such as PAD.[5] |
|

|
| Posterior tibial artery pulse | The posterior tibial artery provides blood flow to the posterior compartment of the leg. A weak posterior tibial pulse may signify PAD or compartment syndrome.[6] |
|

|
| Capillary refill time
(CRT) |
|
|

|
| Rubor dependency test[8] |
|
Please read the special topic box below for more information on this test
|
Please view the video below for an example of how to perform this test. |
| Grading Scale | Description |
|---|---|
| 3-Point Scale[10] | 0 no palpable pulse
1+ weak pulse 2+ normal pulse 3+ increased, full, bounding pulse |
| 4-Point Scale[11] | 0 no palpable pulse
1 + faint, but detectable pulse 2 + suggesting a slightly more diminished pulse than normal 3 + is a normal pulse 4 + bounding pulse |
The following short video includes a demonstration of how to perform the CRT and rubor dependency test.
Special topic: What is dependent rubor and how is it tested at the bedside?[8]
Dependent rubor (also known as erythromelalgia chronic rubor, reactionary rubor, induced rubor, and hyperemic response) is a physiological sign associated with PVD.[13] It is a dusky-red discolourisation of the lower leg and foot which occurs when the extremity is placed in a dependent position below the heart. It occurs because the arterioles in that extremity are maximally dilated as a compensatory response to ischaemia. The arterioles fail to constrict despite the hydrostatic pressure being high when the extremity is in the dependent position, resulting in red discolourisation.[14]
Moving a healthy foot into a dependent position decreases capillary blood flow, and elevation produces no changes in blood flow. However, the same positioning in patients with PVD increases capillary blood flow in the dependent position and decreases capillary blood flow with elevation.[13] This change in physiology is the basis of the rubor dependency testing.
'The Buerger test is classically performed by:
- Placing the patient in supine
- Elevating the leg to 90 degrees to the horizontal plane until pallor is noted
- The leg is then slowly lowered, and the angle at which colour returns is recorded. This angle is known as the angle of circulatory sufficiency.
'The rubor dependency test (variation of the Buerger test) is performed by:
- Placing the patient in supine
- Elevating the leg to 60 degrees from the horizontal plane for 2 minutes, note any appearance of pallor
- The leg is then moved into the dependent position for another 2 minutes, note any change in colour. The dependent positioning of the leg can be achieved by asking the patient to sit at the bed of the examination surface with legs dangling over the side.[15]
Limb pallor during this test indicates peripheral artery disease, as does rubor in the dependent position.[13]
Other modifications to this examination found in the literature include:
- The angle of elevation of the leg when observing for pallor[13][15]
- Addition of exercise, such as ankle pumps, when the leg is elevated[16]
- With legs elevated above the level of the heart, gently ‘milk’ the colour from the patient's feet. Persistent pallor after 30 seconds suggests severe PAD with this technique.[15]
According to Wright et al.,[13] the angle which results in pallor in the leg is likely to be important in identifying the extent of circulatory disturbance and prognosis. However, at the time of publication of Wright and colleague's article, no studies had been completed that correlate specific angles to the degree of arterial occlusion.[13] For example, a textbook published in 2019 teaches that elevating an ischaemic leg 15-30 degrees for 30-60 seconds is enough to cause pallor in the suspected limb.[17] Further research may provide insight into the degree of elevation and its relationship to the severity of arterial occlusion. This would provide rehabilitation professionals with a stronger bedside assessment tool to aid in the creation of effective plans of care and when to initiate a medical referral.
Research has shown that the "Buerger test may be highly sensitive for detecting arterial occlusions below the popliteal fossa but is not specific for arterial occlusion above the popliteal fossa."[13] This strengthens the case that a positive Buerger test indicates probable PVD.[13]
Other tests that may be considered are the (1) toe-brachial index, (2) transcutaneous oxygen pressure, or (3) segmental perfusion pressure. The gold standard to diagnose PAD is contrast angiography, which is an invasive exam.[1]
PAD Risk Factors[edit | edit source]
Risk factors for PAD and arterial ulcers:
- Smoking. Cigarette smoking doubles the risk of PAD. The risk increases cumulatively with the number of cigarettes smoked and the number of years spent smoking.[1]
- Age above 60 years
- 5-10% of those aged 50 to 80 years has PAD.
- 20-30% of those over 80 years have PAD.[1]
- Diabetes. The risk of PAD in patients with diabetes is increased by two to three times.[1]
- Hypertension
- High cholesterol
- Atherosclerosis. However, it is important to note that not all PAD is caused by atherosclerosis.[3] Health screening and referral to the appropriate healthcare provider can assist with a formal diagnosis.
- Sedentary lifestyle
- Family history
Both sexes are affected by PAD. However, biological males are more likely to present with claudication symptoms and biological females are more likely to be asymptomatic.[1]
PAD Differential Diagnosis[edit | edit source]
Spinal stenosis, a condition commonly treated in rehabilitation clinics, can present with symptoms similar to peripheral arterial disease. It is important to be able to differentiate between the symptoms of these conditions, but also to be aware that they can both occur simultaneously.[1]
- Ischaemic claudication pain associated with PAD:[1]
- In the early stages, can be relieved with rest.
- In the later stages, pain is present at rest and does not change except when the limb is placed in a dependent position.
- Spinal stenosis claudication pain:[1]
- Typically relieved with a change in position that reduces the compression at the spine, such as moving from standing to sitting; sitting to lying; extension into flexion.
- Looking at the other signs and symptoms of PAD will also help to differentiate between the two.
Arterial Wound Characteristics[edit | edit source]
- Occur on the lower third of the leg.
- Often seen on the lateral side and distally, ie: the mid-tibia region, the lateral malleolus, the toes, the web spaces, and the heels.
- Wound bed tends to be pale with well-defined edges or a punched out appearance.
- Wound bed is typically dry and has minimal drainage. It usually does not bleed.
- Necrotic tissue is common, especially black eschar.
- The skin is pale, darkened, or cyanotic.
- The area of skin around the wound is commonly shiny, brittle, and hairless.
- May observe slow-growing, brittle, or rigid toenails.
- The posterior tibial and/or dorsalis pedis pulses are diminished or absent.
- The lower leg is often cool to the touch and muscle atrophy can be observed in the calves or feet.
- Arterial wounds are typically quite painful, pain is often worse with elevation. In the later stages of PAD, pain at rest and burning in the toes and soles of the feet are common.
Symptoms of PAD and arterial wounds:[1]
- Slow healing wounds
- Feet usually feel "cold, tingly or numb"
- Muscle cramping is common, especially with exercise or exertion in daily activities such as stair climbing
How PAD pain can effect rehabilitation assessments:[1]
- Pain symptoms are often reported unilaterally. However, approximately 80% of patients have significant bilateral disease. If one side is more severe, it may be masking symptoms on the contralateral side.
- Pain is commonly relieved with a dependency position which can result in oedema in the limb. This is significant for differential diagnosis with venous disease.
- Ambulation tolerance is limited by pain, cramping, or weakness after a few blocks distance. Watch for expected patterns of pain improving with rest to differentiate from other types of walking pain.
Arterial Wound Management[edit | edit source]
The three most important factors in arterial wound management:[1]
- Perfusion. Tissue perfusion needs to be restored as soon as possible and must be addressed before any wound healing can occur. Avoid compression and elevation in these patients. If screening tests indicate poor perfusion, the patient should receive an ankle-brachial index test and a referral back to a vascular specialist.
- Smoking cessation. This is the largest modifiable risk factor for arterial ulcers. Smoking cessation has been shown to restore the tissue microenvironment and cellular functions within approximately four weeks time and continues the longer the individual can abstain from smoking. Please see additional resources section for more information.
- Nutrition. In general, adequate hydration and reducing trans fats and inflammatory foods will all help to manage blood pressure, cholesterol, and inflammation.[18] Ideally, each patient should work with a dietitian to develop a customised nutrition plan.
Venous Ulcers[edit | edit source]
Venous ulcers (also known as venous stasis ulcers, venous insufficiency ulcers, or varicose ulcers) are caused by malfunctioning valves in the veins which increase venous hypertension. This results in blood pooling and decreases the ability of the circulatory system to efficiently pump blood back towards to heart causing venous insufficiency. Blood pooling and venous hypertension also result in blood cells and proteins leaching out into the surrounding subcutaneous tissues, causing oedema and the eventual tissue breakdown and wound formation due to lack of oxygen and nutrients.[19]
- Venous ulcers are the most common type of chronic wound, accounting for more than 70% of all leg ulcers.
- Approximately one-third of adults have venous insufficiency, the prevalence increases with age.
- Chronic venous insufficiency (CVI) is approximately three times more common in biological females than biological males primarily due to the effect oestrogen and progesterone have on vein function.
- Approximately 25% of patients with CVI will have concomitant arterial disease. Use the PAD screening tests listed above to screen for a mixed symptom presentation.[1]
Venous Wound Characteristics[edit | edit source]
- Occur on the lower third of the leg in the gaiter area.
- More common on the medial side of the leg.
- Venous wounds tend to be shallow with uneven edges and a granular or a gelatinous fibrotic base.
- Yellow slough may be seen, but black or brown eschar is rare.
- Venous wounds tend to be wet due to the often copious amount of serous exudate which seeps from the wound and sometimes weeps from the surrounding skin.
- Venous wounds have an insidious onset and are often proceeded by changes in skin colour and texture. The skin may appear inflamed, thickened, crusty, scaled, shiny or tight.
- Stasis dermatitis may occur: redness is seen in lighter skin tones and a purple-grey or ashen tone is seen in darker skin tones.
- Varicose veins
- Haemosiderin staining may occur: brownish speckled staining of the skin.
- Atrophie blanche may occur: whitish discolouration of the skin. This can be seen in the skin with healed ulcers or may be a precursor to future ulceration.
- Pulses are present but can be difficult to palpate if the patient has severe oedema.
- The lower leg is typically warm to the touch.
- Venous wounds are less painful than arterial wounds, and patients often report feeling "aches" in their entire lower extremity.
Chronic oedema and venous wounds:[1]
- Common symptoms in CVI.
- Chronic oedema is worse after prolonged standing.
- Initially, oedema is pitting, meaning a finger intention will stay visible after pressing on the skin.
- In more advanced disease, oedema may become firm and have a 'woody' consistency. This presents as a dark, discoloured, firm, nonpitting oedema.
- Late stages of the disease may present with a 'champagne bottle' shape of the lower leg.
- For differential diagnosis: CVI oedema is generally only observed below the knee, if it extends up into the thigh it is more likely to be due to lymphoedema.
- For differential diagnosis: CVI oedema is also likely to be unilateral, if oedema is bilateral and equal, it is more likely due to medications or another systemic condition such as congestive heart failure.
Symptoms of CVI and venous ulcers:[1]
- Common for wounds to improve and regress multiple times. 60-70% of patients who have had a venous wound will have a recurrence within 10 years.
- Aching or cramping in the leg.
- Patient reports the leg feeling "heavy or tired".
- Itching or tingling of the skin is common, especially with stasis dermatitis.
- Discomfort is relieved with elevation and worsened with dependency or prolonged standing.
- Frequent urination at night.
- Achey lower legs.
CVI screening and examination[edit | edit source]
- Skin assessment: looking for visible varicose veins, oedema, and any skin changes that are commonly seen with CVI
- Assess arterial circulation with palpation of the posterior tibial and dorsalis pedis pulses
- If pulses are not palpable, check capillary refill. If it is intact, the lack of pulses is more likely due to venous oedema rather than arterial insufficiency occluding the vessels.
- Brodie-Trendelenberg's and Perthe's tests can be used clinically to test for venous backflow.[1] Please see the additional resources section for optional reading about these tests.
Please view the following optional video for a quick demonstration of a peripheral venous examination as performed by a medical doctor, including the Brodie-Trendelenburg and Perthe's tests.
Venous Wound Management[edit | edit source]
The three most important factors for venous wound management:
- Compression. Oedema management is vital for proper wound healing. Compression must be worn 24 hours a day and kept dry. For patients with an open wound, compression dressings are changed regularly as the circumference changes with oedema fluid loss. Once the wounds have healed and the oedema is stable, the limb should be measured for custom compression stockings. These should be worn all day when the patient's leg would be in a dependent position but can be removed for sleep. The patient may continue to use old compression stockings if they are in good shape and provide the appropriate amount of compression. Patients should not continue to wear compression stockings that have holes or runs. Stockings typically need to be replaced every six months. And if possible, the patient should have two pairs so that they have something to wear while one of them is being washed.[1] Do not put compression stockings in the dryer.
- Prior to applying any compression, you need to ensure that the patient has adequate tissue perfusion and that the level of compression is appropriate for them. This is determined with ABI testing.[1]
- Nutrition. As with arterial ulcers, a patient with venous wounds will require adequate hydration and reduced intake of foods that can cause inflammation of the blood vessels.[18]
- Exercise. Encourage exercises that activate muscle pump action in the lower extremities to assist with venous return, examples include: a walking programme, bicycling, ankle pumps, ankle circumduction, ankle alphabet, heel-toe raises in both sitting and standing positions, and ankle rocker board exercises. Include soleus stretches and ankle mobility to optimise ankle joint range of motion. Whenever possible, combine exercises with supine positioning and elevate the legs above the level of the heart to have gravity assist with venous return.[1]
Resources[edit | edit source]
Clinical resources for patient education:
- World Health Organization (WHO) resources for smoking cessation
Optional additional reading on Brodie-Trendelenberg and Perthes screening tests:
- Kim J, Richards S, Kent PJ. Clinical examination of varicose veins--a validation study. Annals of the Royal College of Surgeons of England. 2000 May;82(3):171.
- Krishnan S, Nicholls SC. Chronic venous insufficiency: clinical assessment and patient selection. InSeminars in Interventional Radiology 2005 Sep (Vol. 22, No. 03, pp. 169-177). Copyright© 2005 by Thieme Medical Publishers, Inc., 333 Seventh Avenue, New York, NY 10001, USA..
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 1.23 1.24 1.25 1.26 1.27 Palmer, D. Characteristics and Identification of Wound Types. Physiotherapy Wound Care Programme. Plus. 2022.
- ↑ Wound Source. Arterial Ulcers. Available from: https://www.woundsource.com/patientcondition/arterial-ulcers (accessed 10/09/2022).
- ↑ 3.0 3.1 Centers for Disease Control and Prevention. Peripheral Arterial Disease (PAD). Available from: https://www.cdc.gov/heartdisease/PAD.htm (accessed 10/09/2022).
- ↑ Crawford F, Welch K, Andras A, Chappell FM. Ankle brachial index for the diagnosis of lower limb peripheral arterial disease. Cochrane Database of Systematic Reviews. 2016(9).
- ↑ Verywell Health. Anatomy of the Dorsalis Pedis Artery. Available from: https://www.verywellhealth.com/dorsalis-pedis-artery-5097663 (accessed 11/09/2022).
- ↑ Verywell Health. The Anatomy of the Posterior Tibial Artery. Available from: https://www.verywellhealth.com/posterior-tibial-artery-anatomy-4707725#:~:text=The%20posterior%20tibial%20artery%20plays,connects%20to%20the%20femoral%20artery. (accessed 11/09/2022).
- ↑ McGuire D, Gotlib A, King J. Capillary Refill Time. InStatPearls [Internet] 2022 Apr 21. StatPearls Publishing.
- ↑ 8.0 8.1 Hamm, RL. Text and atlas of wound diagnosis and treatment, (2nd ed). 2019. McGraw Hill.126044046X
- ↑ 9.0 9.1 Woundcare Advisor. What’s causing your patient’s lower-extremity redness? Available from: https://woundcareadvisor.com/whats-causing-your-patients-lower-extremity-redness_vol2-no4/#:~:text=Dependent%20rubor%20is%20a%20fiery,is%20cool%20to%20the%20touch. (accessed 11/09/2022).
- ↑ Lapum JL, Verkuyl M, Garcia W. Vital Sign Measurement Across the Lifespan–1st Canadian Edition. OpenStax Anatomy and Physiology; 2017.
- ↑ Hill RD, Smith RB. Chapter 30: Examination of the extremities: pulses, bruits, and phlebitis. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd ed. Boston, MA: Butterworths. 1990.
- ↑ YouTube. Capillary Refill & Rubor of Dependency - Vascular Test | Klose Training. Available from: https://www.youtube.com/watch?v=eJWbJ4pzX18 [last accessed 11/09/2022]
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 13.6 13.7 Wright WF, Rajachandran M. Buerger Test for erythromelalgia revisited. Journal of Osteopathic Medicine. 2017 Feb 1;117(2):124-6.
- ↑ Ijaz S, Mazhar M, Ali I, Latif F. Every red is not cellulitis: dependent rubor rare but classical finding of severe arterial insufficiency. Hospital Medicine 2018; 2018 April 8-11; Orlando, FL, USA.
- ↑ 15.0 15.1 15.2 Bartholomew JR. From the Masters: Lessons learned about the vascular medicine history and physical examination from the past and present. Vascular Medicine. 2021 Aug;26(4):361-6.
- ↑ Insall RL, Davies RJ, Prout WG. Significance of Buerger's test in the assessment of lower limb ischaemia. Journal of the Royal Society of Medicine. 1989 Dec;82(12):729-31.
- ↑ Sacchidanand S, Eswari L, Shilpa K. Leg Ulcers: Diagnosis & Management. Jaypee Brothers Medical Publishers; 2019 Sep 30.
- ↑ 18.0 18.1 Hart MJ, Torres SJ, McNaughton SA, Milte CM. Dietary patterns and associations with biomarkers of inflammation in adults: a systematic review of observational studies. Nutrition journal. 2021 Dec;20(1):1-4.
- ↑ Wound Source. Venous Ulcers. Available from: https://www.woundsource.com/patientcondition/venous-ulcers (accessed 10/14/2022).
- ↑ YouTube. Examination of the Peripheral Venous System. Available from: https://www.youtube.com/watch?v=veeEgFHmz4M [last accessed 14/09/2022]