Central Sensitisation: Difference between revisions
No edit summary |
No edit summary |
||
| Line 244: | Line 244: | ||
= Management of Central Sensitization = | = Management of Central Sensitization = | ||
{| width="40%" cellspacing="1" cellpadding="1" border="0" align="right" | |||
|- | |||
| {{#ev:youtube|dlSQLUE4brQ|250}} | |||
| <ref>Pain-Ed.com. Prof Peter O'Sullivan - Back pain - separating fact from fiction. Available from: http://www.youtube.com/watch?v=dlSQLUE4brQ[last accessed 22/11/15]</ref> | |||
|} | |||
<br> | |||
== Patient Education == | == Patient Education == | ||
| Line 264: | Line 271: | ||
The second session can be used to correct misunderstandings, and to facilitate the transition from knowledge to adaptive pain coping during daily life. Pain physiology education is a continuous process initiated during the educational sessions and continued within both the active treatment and during the longer term rehabilitation program<ref name="Nijs 2010">Nijs J, Van Houdenhove B, Oostendorp RAB. Recognition of central sensitization in patients with musculoskeletal pain: application of pain neurophysiology in manual therapy practice. Manual Therapy 2010;15:135-41</ref>. <br> | The second session can be used to correct misunderstandings, and to facilitate the transition from knowledge to adaptive pain coping during daily life. Pain physiology education is a continuous process initiated during the educational sessions and continued within both the active treatment and during the longer term rehabilitation program<ref name="Nijs 2010">Nijs J, Van Houdenhove B, Oostendorp RAB. Recognition of central sensitization in patients with musculoskeletal pain: application of pain neurophysiology in manual therapy practice. Manual Therapy 2010;15:135-41</ref>. <br> | ||
<br> | <br> | ||
= Resources = | = Resources = | ||
Revision as of 19:48, 29 February 2016
Original Editor - Nathan Benson as part of the PPA Pain Project.
Top Contributors - Alberto Bertaggia, Nathan Benson, Laura Ritchie, Jo Etherton, Shaimaa Eldib, Jess Bell, Bruno Serra, Uchechukwu Chukwuemeka, Kim Jackson, Lucinda hampton, Admin, Michelle Lee, Melissa Coetsee, Evan Thomas, WikiSysop and Claire Knott
Central Sensitisation[edit | edit source]
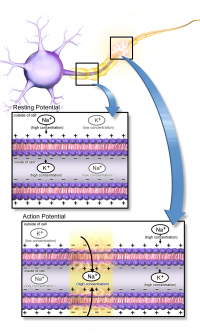
Nociception is described by IASP as the neural process of encoding noxious stimuli. Central sensitisation describes the circumstances in which there is an enhancement of the function of neurons involved in nociception [1] resulting in
- hypersensitivity to stimuli[2],
- responsiveness to non-noxious stimuli[3]
- and an increased pain response evoked by stimuli outside the area of injury, an expanded receptive field[4].
The International Association for the Study of Pain (IASP) describes central sensitization as
“Increased responsiveness of nociceptive neurons in the central nervous system to their
normal or subthreshold afferent input.”[3]
Neural plasticity plays a role in cellular changes with a demonstrable increase in both membrane excitability and synaptic efficacy. The effect of this process is the recruitment of additional, sub-threshold synaptic inputs to nociception resulting in a greater field of receptivity and an increased output of nociception.The effects of this process may persist beyond the duration of the initial noxious input resulting in pain hypersensitivity to normally innocuous stimuli.
It is also thought to play a role in affecting pain facilitation and inhibition; inhibiting descending pathways[5] and over-activation of the ascending, pain facilitatory pathways[6]. Which, simplifed, means too many messages going in and not enough coming out.
The use of the term "central sensitisation" varies sometimes referring solely to the neural plastic changes only and sometimes to the the complex and multiple processes and systems which contribute to changes in the elicitation and perception of pain[7][8][9]. A discussion about the various descriptions and defintion s can be found on the Body in MInd website. The term was first used in a study of pain hypersensitivity in rats following repeated noxious stimuli to describe the use dependant neural plasticity demonstrated[10][7]. These central changes due to peripheral noxious stimuli have been referred to as "activity-dependant central sensitisation"[2].
Activity Dependent Central sensitization[edit | edit source]
Latremoliere and Woolf describe the changes demonstrated in their group's 1983 study as "activity dependent central sensitization". This describes the mechanism of functional synaptic plasticity evoked by in the dorsal horn neurons by input from nociceptors [2]. They found to invoke sensitization the noxious stimuli had to be sustained, intense and repeated. The changes can be divided into two, time dependent phases: an early, short duration phase which is phosphorylation-dependant/transcription-independent, and a longer lasting transcription-dependant phase[11].
Activation of the NMDA receptor is an essential step in initiating and maintaining the sensitization (N-Methyl-D-Aspartate is a glutamate receptor. Glutamate is a widespread excitatory neurotransmitter in aht enwevious system). Under normal circumstances this receptor channel is blocked by Mg2+ ions[12]. Sustained release by nociceptors of glutamate, substance P and CGRP leads to membrane de-polarization, forcing the Mg2+ from the NMDA receptor[12]. This rapidly boosts synaptic efficacy and allows Ca2+ in to the neuron, activating intracellular pathways and maintaining central sensitization[2].
Central vs Peripheral Sensitization[edit | edit source]
While descriptively central sensitization and Peripheral sensitisation may appear to be comparable processes, they represent quite distinct and processes and clinical features[2].
Peripheral sensitisation is described by the IASP as
"Increased responsiveness and reduced threshold of nociceptive neurons in the periphery to
the stimulation of their receptive fields."[13]
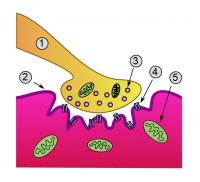
It is initiated when the peripheral terminus of nociceptors are exposed to noxious stimulus, for example inflammatory mediators in damaged tissue. On going stimulation results in a lowering of the activation threshold and thus and increase in responsiveness of nociceptors [14].
As a result of this it generally requires on going peripheral pathology for the sensitization to be maintained and is generally localised to the site of injury[14]. It has a role in altered heat sensation, but not in mechanical sensitivity[2].
In the process of central sensitisation novel inputs are recruited to the nociceptive pathways such as large, low-threshold mechanoreceptors classified as Aß fibres. This results in hypersensitivity in non-inflamed tissue and to touch.
| [15] | [16] |
Features of Central Sensitization[edit | edit source]
A survey of expert clinicians in a Delphi-derived survey found the following characteristics to describe central sensitisation in the clinical setting [1].
Subjective features[edit | edit source]
| [17] |
- Disproportionate, non-mechanical, unpredictable pattern of pain provocation in response to multiple/non-specific aggravating/easing factors.
- Pain persisting beyond expected tissue healing/pathological recovery times.
- Pain disproportionate to the nature and extent of injury or pathology.
- Widespread, non-anatomical distribution of pain.
- History of failed interventions (medical/surgical/therapeutic).
- Strong association with maladaptive psychosocial factors (e.g. negative emotions, poor self-efficacy, maladaptive beliefs, and pain behaviours, altered family/work/social life, medical conflict).
- Unresponsive to NSAIDs and/or more responsive to anti-epileptic (e.g. Lyrica) /anti-depressants (e.g. Amitriptyline) medication.
- Reports of spontaneous (i.e. stimulus independent) pain and/or paroxysmal pain (i.e. sudden recurrences and intensification of pain).
- Pain in association with high levels of functional disability.
- More constant/unremitting pain.
- Night pain/disturbed sleep.
- Pain in association with other dysesthesias (e.g. burning, coldness, crawling).
- Hyperpathia or pain of high severity and irritability (i.e. easily provoked, taking a long time to settle).
Clinical features[edit | edit source]
- Disproportionate, inconsistent, non-mechanical/non-anatomical pattern of pain provocation in response to movement/mechanical testing.
- Positive findings of hyperalgesia (primary, secondary) and/or allodynia and/or hyperpathia within the distribution of pain.
- Diffuse/non-anatomical areas of pain/tenderness on palpation.
- Positive identification of various psychosocial factors (e.g. catastrophisation, fear-avoidance behaviour, distress).
Identification in the Clinical Setting[edit | edit source]
In 2009 Schäfer et al.[18] proposed a classification of low back-related leg pain using an examination protocol which incorporates first the subjective assessment, including the Leeds Assessment of Neuropathic Symptoms and Sign (LANSS) scale [19], and second the physical examination (neurological examination, assessment of active movements, neural tissue provocation tests). Based on this comprehensive assessment, a LANSS score ≥ 12 is indicative of central sensitization in their classification algorithm.
In 2010 Nijs et al.[20] provided guidelines to aid the recognition of central sensitization on musculoskeletal patients.
In their paper they suggest that a patient's medical diagnosis can offer insight into the likelihood of the presence of central sensitization (fig 1) and this in conjunction with observable features (fig 2) can inform the therapist as to the presence of central sensitization.
| Medical Diagnosis | Central sensitization is a characteristic of this disorder | Central Sensitisation is present as a subgroup |
|---|---|---|
| Chronic lower back pain | X | |
| Chronic Whiplash associated disorders | X | |
| (Sub)acute whiplash associated disorders | X | |
| Tempromandibular disorders | X | |
| Myofascial pain syndrome | X | |
| Osteoarthritis | X | |
| Rheumatoid arthritis | X | |
| Fibromyalgia | X | |
| Chronic fatigue syndrome | X | |
| Chronic headache | X | |
| Irritable bowel syndrome | X |
| Symptom | Characteristic of central sensitization | Might be related to Central sensitization |
|---|---|---|
| Hypersensitivity to bright light | X | |
| Hypersensitivity to touch | X | |
| Hypersensitivity to noise | X | |
| Hypersensitivity to pesticides | X | |
| Hypersensitivity to mechanical pressure | X | |
| Hypersensitivity to medication | X | |
| Hypersensitivity to temperature (high or low) | X | |
| Fatigue | X | |
| Sleep disturbances | X | |
| Unrefreshing sleep | X | |
| Concentration difficulties | X | |
| Swollen feeling (e.g. in limbs) | X | |
| Tingling | X | |
| Numbness | X |
In 2012 Mayer et al.[21] proposed the Central Sensitization Inventory (CSI). The clinical goal of this screening instrument is to help better assess symptoms thought to be associated with CS in order to aid physicians and other clinicians in syndrome categorization, sensitivity, severity identification, and treatment planning, to help minimize, or possibly avoid, unnecessary diagnostics and treatment procedures. CSI has showed good psychometric strength, the clinical utility, and the initial construct validity.
Management of Central Sensitization[edit | edit source]
| [22] |
Patient Education[edit | edit source]
In cases of central sensitization it is important to:
- change maladaptive illness perceptions,
- alter maladaptive pain cognitions,
- reconceptualise pain.
This can be accomplished with pain physiology education, which is indicated when:
- the clinical picture is characterized and dominated by central sensitization;
- maladaptive illness perceptions are present.
Face-to-face sessions of pain physiology education, in conjunction with written educational material, are effective for changing pain cognitions and improving health status in patients with various chronic musculoskeletal pain disorders (i.e. chronic low back pain, chronic whiplash, fibromyalgia and chronic fatigue syndrome).
After biopsychosocial assessment pain physiology education comprises of a first face-to-face session explaining basic pain physiology and contrasting acute nociception versus chronic pain (Session 1). Written information about pain physiology should be provided as homework in between session 1 and 2.
The second session can be used to correct misunderstandings, and to facilitate the transition from knowledge to adaptive pain coping during daily life. Pain physiology education is a continuous process initiated during the educational sessions and continued within both the active treatment and during the longer term rehabilitation program[20].
Resources[edit | edit source]
"How to explain central sensitisation to patients with ‘unexplained’ chronic musculoskeletal pain: Practice guideline" - open access article can be found here.
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1RIspYzP7yk4pbK3U806M4LBHEmQhSRy29rApnG1uIHyHURUAg|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
- ↑ 1.0 1.1 Smart KM, Blake C,Staines A, Doody C. Clinical Indicators of "Nociceptive", "peripheral neuropathic", and "central sensitisation" as mechanisms based classifications of musculoskeletal pain. A Delphi survey of expert clinicians. Manual Therapy 2010;15:80-7
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Woolf CJ, Latremoliere A. Central Sensitization: A generator of pain hypersensitivity by central neural plasticity. The Journal of Pain 2009; 10(9):895-926
- ↑ 3.0 3.1 Loeser JD, Treede RD. The Kyoto protocol of IASP basic pain terminology. Pain 2008;137: 473–7.
- ↑ Dhal JB, Kehlet H. Postoperative pain and its management. In:McMahon SB, Koltzenburg M, editors. Wall and Melzack's Textbook of pain. Elsevier Churchill Livingstone;2006. p635-51.
- ↑ Meeus M, Nijs J, Van der Wauwer N, Toeback L, Truijen S. Diffuse noxious inhibitory control is delayed in chronic fatigue syndrome: an experimental study. Pain 2008;139:439-48
- ↑ Meeus M, Nijs J. Central Sensitization: a biopyschosocial explanation for chronic widespread pain in patients with fibromyalgia and chronic fatigue syndrome. Clinical Rheumatology 2007; 26:465-73
- ↑ 7.0 7.1 Woolf CJ. What to call the amplification of nociceptive signals in the central nervous system that contribute to widespread pain? Pain 2014. Article in Press.
- ↑ Hansson P. PAIN 2014. http://dx.doi.org/10.1016/j.pain.2014.07.016. pii: S0304-3959(14)00335-2
- ↑ Body in Mind. Everything you wanted to know about CENTRAL SENSITISATION http://www.bodyinmind.org/central-sensitisation/ (accessed 10 June 2014)
- ↑ Woolf CJ.Evidence of a central component of post-injury pain hypersensitivity. Nature 1983;306;686-688.
- ↑ Woolf CJ, Saltar MW. Neuronal plasticity:increasing the gain in pain. Science 2000;288:1765-69.
- ↑ 12.0 12.1 Mayer ML, Westbroke GL, Guthrie, PB. Voltage-dependant block by Mg2+ of NMDA responses in spinal cord neurones. Nature 1984;309:261-263.
- ↑ International Association for the Study of Pain. Pain Terms: A Current List with Definitions and Notes on Usage. http://iasp.files.cms-plus.com/Content/ContentFolders/Publications2/ClassificationofChronicPain/Part_III-PainTerms.pdf(accessed 12 July 2014
- ↑ 14.0 14.1 Hucho T, Levine JD. Signalling pathways in sensitization: Towards a nociceptor cell biology. Neuron 2007;55:365-376
- ↑ Mayo Clinic. Dr. Sletten Discussing Central Sensitization Syndrome (CSS). Available from: http://www.youtube.com/watch?v=8defN4iIbho [last accessed 22/11/15]
- ↑ Danny Orchard. Peripheral and central sensitisation. Available from: http://www.youtube.com/watch?v=YwDMmSwUOOU [last accessed 22/11/15]
- ↑ Pain-Ed.com. Prof Peter O'Sullivan - Back pain - separating fact from fiction. Available from: http://www.youtube.com/watch?v=dlSQLUE4brQ[last accessed 22/11/15]
- ↑ Schäfer A, Hall T, Briffa K. Classification of low back-related leg pain—A proposed patho-mechanism-based approach. Manual Therapy. 2009 Apr 1;14(2):222–30.
- ↑ Bennett M. The LANSS Pain Scale: the Leeds assessment of neuropathic symptoms and signs. Pain. 2001 May;92(1-2):147–57.
- ↑ 20.0 20.1 20.2 20.3 Nijs J, Van Houdenhove B, Oostendorp RAB. Recognition of central sensitization in patients with musculoskeletal pain: application of pain neurophysiology in manual therapy practice. Manual Therapy 2010;15:135-41
- ↑ Mayer TG, Neblett R, Cohen H, Howard KJ, Choi YH, Williams MJ, et al. The Development and Psychometric Validation of the Central Sensitization Inventory (CSI). Pain Pract. 2012 Apr;12(4):276–85.
- ↑ Pain-Ed.com. Prof Peter O'Sullivan - Back pain - separating fact from fiction. Available from: http://www.youtube.com/watch?v=dlSQLUE4brQ[last accessed 22/11/15]