Cardiac Rehabilitation: Difference between revisions
Evan Thomas (talk | contribs) mNo edit summary |
(Content) |
||
| Line 6: | Line 6: | ||
== Introduction == | == Introduction == | ||
“Cardiac Rehabilitation is the process by which patients with cardiac disease, in partnership with a multidisciplinary team of health professionals are encouraged to support and achieve and maintain optimal physical and psychosocial health. The involvement of partners, other family members and carers is also important” '''(SIGN, 2002)''' | |||
Cardiac rehabilitation is an accepted form of management for people with cardiac disease. Initially, rehabilitation was offered mainly to people recovering from a myocardial infraction (MI), but now encompasses a wide range of cardiac problems. <ref name="cardiac">Pryor JA, Prasad SA. Physiotherapy for Respiratory and Cardiac Problems. Philadelphia: Elsevier Ltd, 4th Edition, 2008: 14 (470 - 494).</ref><br> | Cardiac rehabilitation is an accepted form of management for people with cardiac disease. Initially, rehabilitation was offered mainly to people recovering from a myocardial infraction (MI), but now encompasses a wide range of cardiac problems. <ref name="cardiac">Pryor JA, Prasad SA. Physiotherapy for Respiratory and Cardiac Problems. Philadelphia: Elsevier Ltd, 4th Edition, 2008: 14 (470 - 494).</ref><br> | ||
| Line 16: | Line 18: | ||
Cardiac rehabilitation should be offered to all cardiac patients who would benefit.<ref name="cardiac" /> CR is mainly prescribed to patients with ischemic heart disease, with myocardial infarction, after coronary angioplasty, after coronaro-aortic by-pass graft surgery and to patients with chronic heart failure. CR begins as soon as possible in intensive care units, only if the patient is in stable medical condition. Intensity of rehabilitation depends on patient´s condition and complications in acute phase of disease.<ref name="ref">Cardiac rehabilitation. Available from: http://www.pnmedycznych.pl/spnm.php?ktory=369 (accessed 22.12.2013)</ref><br> | Cardiac rehabilitation should be offered to all cardiac patients who would benefit.<ref name="cardiac" /> CR is mainly prescribed to patients with ischemic heart disease, with myocardial infarction, after coronary angioplasty, after coronaro-aortic by-pass graft surgery and to patients with chronic heart failure. CR begins as soon as possible in intensive care units, only if the patient is in stable medical condition. Intensity of rehabilitation depends on patient´s condition and complications in acute phase of disease.<ref name="ref">Cardiac rehabilitation. Available from: http://www.pnmedycznych.pl/spnm.php?ktory=369 (accessed 22.12.2013)</ref><br> | ||
== Goals of Cardiac Rehabilitation == | |||
'''(IACR, 2013)''' | |||
The main goal of cardiac rehabilitation is to promote secondary prevention and to enhance quality of life among cardiac patients '''(WHO, 1993)''' | |||
{| class="wikitable" | |||
|'''Medical Goals''' | |||
|'''Social Goals''' | |||
|'''Psychological Goals''' | |||
|'''Behavioural Goals''' | |||
|'''Health Service Goals''' | |||
|- | |||
|Improve Cardiac Function | |||
|Return to work if appropriate and/or previous level of functional capacity | |||
|To restore self confidence | |||
|To quit all forms of smoking | |||
|To directly reduce medical costs | |||
|- | |||
|Reduce the risk of sudden death and re-infarcation | |||
|To promote independence in ADLs for those who are compromised | |||
|Relieve anxiety and depression in pt.s and their careers | |||
|To make heart healthy dietary decisions | |||
|To promote early mobilisation and discharge from hospital | |||
|- | |||
|Relieve symptoms such as breathlessness and angina | |||
| | |||
|To relieve or manage stress | |||
|To be physically active | |||
|To reduce cardiac related hospital admission | |||
|- | |||
|Increase Work Capacity | |||
| | |||
|To restore good sexual health | |||
|To adhere to medication regimes | |||
| | |||
|- | |||
|Prevent progression of underlying atherosclerotic process | |||
| | |||
| | |||
| | |||
| | |||
|} | |||
== Individual Risk Assessment == | |||
CR can be tailored to meet individual needs thus a thorough assessment and evaluation of the CV risk factor profile of the patient should be undertaken at the beginning of the programme. This should be accompanied by ongoing assessment and reassessment throughout and upon completion of the programme. | |||
Risk factors should be evaluated using validated measures which take into account other co-morbidities. | |||
''Risk Factors'' | |||
{| class="wikitable" | |||
|'''Non Modifiable''' | |||
|'''Modifiable''' | |||
|- | |||
|Age | |||
|Excessive alcohol intake | |||
|- | |||
|Gender | |||
|Dyslipedemia | |||
|- | |||
|Personal Cardiac History | |||
|Hypertension | |||
|- | |||
|Family History of CVD | |||
|Obesity | |||
|- | |||
|Diabetes (unless prediabetes) | |||
|Smoking | |||
|- | |||
| | |||
|Physical Inactivity | |||
|- | |||
| | |||
|Anxiety/Depression | |||
|- | |||
| | |||
|Hostility | |||
|- | |||
| | |||
|Stress | |||
|} | |||
''Other factors to consider'' | |||
· Family Support | |||
· Social History | |||
· Occupation | |||
== Cardiac Rehabilitation Participation == | |||
· Should be available to all cardiac patients who require it and age should not be considered a barrier. | |||
· Consideration of patient safety at all times led to the formation of the following inclusion and exclusion criteria for phase III of the CR programme; | |||
{| class="wikitable" | |||
|'''Inclusion''' | |||
|'''Exclusion''' | |||
|- | |||
|Medically stable post MI | |||
|Unstable Angina | |||
|- | |||
|Coronary Artery Bypass Surgery | |||
|Ischaemic changes on ECG | |||
|- | |||
|Percutaneous Coronary Intervention | |||
|Resting systolic BP >200mmHg or resting diastolic BP >110 mmHg | |||
|- | |||
|Stable Angina | |||
|Orthostatic BP drop >10mmHg with symptoms | |||
|- | |||
|Stable heart failure (NYHA I-III) | |||
|Critical aortic stenosis (peak pressure gradient >50mmHg with aortic valve orifice <0.75cm2 | |||
|- | |||
|Cardiomyopathy | |||
|Acute systemic illness or fever | |||
|- | |||
|Cardiac Transplantation | |||
|Uncontrolled atrial or ventricular arrhythmias | |||
|- | |||
|Implantable Cardioverter Defibrillator | |||
|Uncontrolled sinus tachycardia (>120bpm) | |||
|- | |||
|Valve Repair/Replacement | |||
|Uncompensated CHF | |||
|- | |||
|Insertion of Cardiac Pacemaker (with one or more other inclusion criteria) | |||
|Acute systemic illness | |||
|- | |||
|Peripheral Arterial Disease | |||
|3<sup>rd</sup> degree AV block with no pacemaker | |||
|- | |||
|Post Cerebral Vascular Disease | |||
|Acute pericarditis/myocarditis | |||
|- | |||
|At risk of coronary artery disease with diagnosis of diabetes, dyslipedemia, hypertension | |||
|Recent embolism | |||
|- | |||
| | |||
|Thromobophlebitis | |||
|- | |||
| | |||
|Uncontrolled diabetes | |||
|- | |||
| | |||
|Severe orthopediac problems | |||
|- | |||
| | |||
|Other metabolic problems such as acute thyroiditis, hypo-hyperkalaemia, hypovolemia | |||
|} | |||
'''(AACPVR, 2004)''' | |||
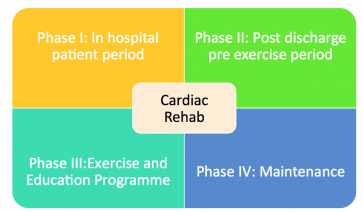
== Phases == | == Phases == | ||
Appropriate referral pathways should be set up so appropriate patients can be identified and invited to attend. Referrals should be invited by cardiologist/physician, cardiothoracic surgeon, cardiac team, cardic rehab co-ordinator, G.P., CCU nurses or members of the MDT. All referrals should include the following; | |||
· Patients name, age, address and contact number | |||
· Type of cardiac event and date of event | |||
· Cardiac history, complications and meds | |||
· Reason for referral | |||
· Referring persons name and contact number, date of request | |||
· Clinically relevant information – results of exercise stress test, echo, fasting lipid profile and fasting glucose profile | |||
[[File:Screen Shot 2017-09-27 at 10.32.43.png|thumb|363x363px|Phases of Cardiac Rehabilitation]] | |||
=== Phase I: In hospital patient period === | |||
2-5 days | |||
Member of CRT should visit the patient to | |||
· Give support and information to them and their families re: heart disease | |||
· Assist the patient to identify personal CV risk factors | |||
· Discuss lifestyle modifications of personal risk factors and help provide an individual plan to support these lifestyle changes | |||
· Gain support from family members to assist the patient in maintaining the necessary progress | |||
· Plan a personal discharge activity programme and encourage the patient to adhere to this and commence daily walks | |||
· Inform patients regarding phase II and phase III programs if available and encourage their attendance | |||
At this stage emphasis is on counteracting the negative effects of a cardiac event not promoting training adaptations (Woods, 2010). Activity levels should be progressed using a staged approach which should be based on the patient’s medical condition. Patient should be closely monitored for any signs of cardiac decompensation. | |||
Educational sessions should be commenced providing information re: | |||
· The cardiac event | |||
· Psychological reactions to the event | |||
· Cardiac pain/symptom management | |||
· Correction of cardiac misconceptions | |||
The use of educational materials such as the heart manual and leaflets from the Irish Heart Foundation should be considered. | |||
Patient should be provided with an individual plan for self care and lifestyle changes based on their clinical assessment and identified risk factors. A discharge plan including exercise instructions should also be formulated. | |||
Patient should also have some form of psychosocial assessment either via interview or use of a self reporting questionnaire such as HADS, Health Realted QoL. | |||
Referrals to other members of the MDT and follow up visits should also be made during this time. | |||
=== Phase II: Post discharge period === | |||
Goals: | |||
· Reinforce cardiac risk factor modification | |||
· Provide education and support to patient and family | |||
· Promote continuing adherence to lifestyle recommendations. | |||
SIGN 2002 – state the importance of addressing any psychological distress or poor social support issues as these two factors have been identified as being powerful predictors of outcome post MI irrespective of the degree of physical impairment. | |||
Support and education can be provided through | |||
· Home visits | |||
· Phone calls | |||
· Outpatient reviews | |||
· Provision of educational classes (individual/group) | |||
· Use of the heart manual | |||
Could also look into establishing links with GP, practice nurses, primary care team and chest pain services. | |||
Gradual activity and low level exercise regime may commence once stable. Intensity will increase over a varying period of time depending on diagnosis and procedure and is done under guidance of the cardiologist | |||
- <2 weeks post uncomplicated PCI | |||
- 2 weeks post MI | |||
- 3 weeks post cardiac surgery '''(Parker et al., 2011; Williams, 2006)''' | |||
ACSM suggest 4-6 weeks post MI and post sternotomy unless otherwise directed by cardiologist/cardiothoracic surgeon | |||
Phase III: Cardiac Rehabilitation and secondary prevention | |||
Structured exercise training with continual educational and psychological support and advice on risk factors '''(SIGN, 2002)''' | |||
Should take a menu based approach and be individually tailored. | |||
Typically lasts at least 6 weeks with patients exercising 2/7 minimum. | |||
Exercise class will consist of warm up, exercise class, cool down – may also include resistance training with active recovery stations where appropriate. | |||
=== Phase III compromises of all the following; === | |||
· Exercise prescription based on | |||
o Clinical status | |||
o Risk Stratification | |||
o Previous activity | |||
o Future needs | |||
· Education for patient and family re: | |||
o Cardiac anatomy and physiology | |||
o Recognition of cardiac pain and symptom management | |||
o Risk factor identification and management | |||
o Benefits of PA | |||
o Energy conservation techniques/graded return to ADLs | |||
o Cardio protective healthy eating | |||
o Benefits and entitlements | |||
· Stress management and relaxation techniques | |||
· Counselling and behaviour modification | |||
· Smoking cessation | |||
· Vocational counselling '''(IACR, 2013)''' | |||
<br> | |||
=== Phase IV: Maintenance === | |||
Goal: facilitate long term maintenance of lifestyle changes, monitoring risk factor changes and secondary prevention. | |||
Options: | |||
- Educational sessions | |||
- Support groups | |||
- Telephone follow up | |||
- Review in clinics | |||
- Outreach programmes | |||
- Phase IV exercise programme organised by qualified phase IV gym instructor | |||
- Links with GP and primary health care team | |||
- Ongoing involvement of partners/spouses/family | |||
== Resources == | == Resources == | ||
Revision as of 11:35, 27 September 2017
Original Editor Rachael Lowe
Top Contributors - Magdalena Hytros, Garima Gedamkar, Adam Vallely Farrell, Admin, Kim Jackson, Vidya Acharya, Lucinda hampton, Rachael Lowe, WikiSysop, Simisola Ajeyalemi, Karen Wilson, Olajumoke Ogunleye, Evan Thomas, Naomi O'Reilly and Tarina van der Stockt
Introduction[edit | edit source]
“Cardiac Rehabilitation is the process by which patients with cardiac disease, in partnership with a multidisciplinary team of health professionals are encouraged to support and achieve and maintain optimal physical and psychosocial health. The involvement of partners, other family members and carers is also important” (SIGN, 2002)
Cardiac rehabilitation is an accepted form of management for people with cardiac disease. Initially, rehabilitation was offered mainly to people recovering from a myocardial infraction (MI), but now encompasses a wide range of cardiac problems. [1]
Description[edit | edit source]
Indication[edit | edit source]
Cardiac rehabilitation should be offered to all cardiac patients who would benefit.[1] CR is mainly prescribed to patients with ischemic heart disease, with myocardial infarction, after coronary angioplasty, after coronaro-aortic by-pass graft surgery and to patients with chronic heart failure. CR begins as soon as possible in intensive care units, only if the patient is in stable medical condition. Intensity of rehabilitation depends on patient´s condition and complications in acute phase of disease.[3]
Goals of Cardiac Rehabilitation[edit | edit source]
(IACR, 2013) The main goal of cardiac rehabilitation is to promote secondary prevention and to enhance quality of life among cardiac patients (WHO, 1993)
| Medical Goals | Social Goals | Psychological Goals | Behavioural Goals | Health Service Goals |
| Improve Cardiac Function | Return to work if appropriate and/or previous level of functional capacity | To restore self confidence | To quit all forms of smoking | To directly reduce medical costs |
| Reduce the risk of sudden death and re-infarcation | To promote independence in ADLs for those who are compromised | Relieve anxiety and depression in pt.s and their careers | To make heart healthy dietary decisions | To promote early mobilisation and discharge from hospital |
| Relieve symptoms such as breathlessness and angina | To relieve or manage stress | To be physically active | To reduce cardiac related hospital admission | |
| Increase Work Capacity | To restore good sexual health | To adhere to medication regimes | ||
| Prevent progression of underlying atherosclerotic process |
Individual Risk Assessment[edit | edit source]
CR can be tailored to meet individual needs thus a thorough assessment and evaluation of the CV risk factor profile of the patient should be undertaken at the beginning of the programme. This should be accompanied by ongoing assessment and reassessment throughout and upon completion of the programme.
Risk factors should be evaluated using validated measures which take into account other co-morbidities.
Risk Factors
| Non Modifiable | Modifiable |
| Age | Excessive alcohol intake |
| Gender | Dyslipedemia |
| Personal Cardiac History | Hypertension |
| Family History of CVD | Obesity |
| Diabetes (unless prediabetes) | Smoking |
| Physical Inactivity | |
| Anxiety/Depression | |
| Hostility | |
| Stress |
Other factors to consider
· Family Support
· Social History
· Occupation
Cardiac Rehabilitation Participation[edit | edit source]
· Should be available to all cardiac patients who require it and age should not be considered a barrier.
· Consideration of patient safety at all times led to the formation of the following inclusion and exclusion criteria for phase III of the CR programme;
| Inclusion | Exclusion |
| Medically stable post MI | Unstable Angina |
| Coronary Artery Bypass Surgery | Ischaemic changes on ECG |
| Percutaneous Coronary Intervention | Resting systolic BP >200mmHg or resting diastolic BP >110 mmHg |
| Stable Angina | Orthostatic BP drop >10mmHg with symptoms |
| Stable heart failure (NYHA I-III) | Critical aortic stenosis (peak pressure gradient >50mmHg with aortic valve orifice <0.75cm2 |
| Cardiomyopathy | Acute systemic illness or fever |
| Cardiac Transplantation | Uncontrolled atrial or ventricular arrhythmias |
| Implantable Cardioverter Defibrillator | Uncontrolled sinus tachycardia (>120bpm) |
| Valve Repair/Replacement | Uncompensated CHF |
| Insertion of Cardiac Pacemaker (with one or more other inclusion criteria) | Acute systemic illness |
| Peripheral Arterial Disease | 3rd degree AV block with no pacemaker |
| Post Cerebral Vascular Disease | Acute pericarditis/myocarditis |
| At risk of coronary artery disease with diagnosis of diabetes, dyslipedemia, hypertension | Recent embolism |
| Thromobophlebitis | |
| Uncontrolled diabetes | |
| Severe orthopediac problems | |
| Other metabolic problems such as acute thyroiditis, hypo-hyperkalaemia, hypovolemia |
(AACPVR, 2004)
Phases[edit | edit source]
Appropriate referral pathways should be set up so appropriate patients can be identified and invited to attend. Referrals should be invited by cardiologist/physician, cardiothoracic surgeon, cardiac team, cardic rehab co-ordinator, G.P., CCU nurses or members of the MDT. All referrals should include the following;
· Patients name, age, address and contact number
· Type of cardiac event and date of event
· Cardiac history, complications and meds
· Reason for referral
· Referring persons name and contact number, date of request
· Clinically relevant information – results of exercise stress test, echo, fasting lipid profile and fasting glucose profile
Phase I: In hospital patient period[edit | edit source]
2-5 days
Member of CRT should visit the patient to
· Give support and information to them and their families re: heart disease
· Assist the patient to identify personal CV risk factors
· Discuss lifestyle modifications of personal risk factors and help provide an individual plan to support these lifestyle changes
· Gain support from family members to assist the patient in maintaining the necessary progress
· Plan a personal discharge activity programme and encourage the patient to adhere to this and commence daily walks
· Inform patients regarding phase II and phase III programs if available and encourage their attendance
At this stage emphasis is on counteracting the negative effects of a cardiac event not promoting training adaptations (Woods, 2010). Activity levels should be progressed using a staged approach which should be based on the patient’s medical condition. Patient should be closely monitored for any signs of cardiac decompensation.
Educational sessions should be commenced providing information re:
· The cardiac event
· Psychological reactions to the event
· Cardiac pain/symptom management
· Correction of cardiac misconceptions
The use of educational materials such as the heart manual and leaflets from the Irish Heart Foundation should be considered.
Patient should be provided with an individual plan for self care and lifestyle changes based on their clinical assessment and identified risk factors. A discharge plan including exercise instructions should also be formulated.
Patient should also have some form of psychosocial assessment either via interview or use of a self reporting questionnaire such as HADS, Health Realted QoL.
Referrals to other members of the MDT and follow up visits should also be made during this time.
Phase II: Post discharge period[edit | edit source]
Goals:
· Reinforce cardiac risk factor modification
· Provide education and support to patient and family
· Promote continuing adherence to lifestyle recommendations.
SIGN 2002 – state the importance of addressing any psychological distress or poor social support issues as these two factors have been identified as being powerful predictors of outcome post MI irrespective of the degree of physical impairment.
Support and education can be provided through
· Home visits
· Phone calls
· Outpatient reviews
· Provision of educational classes (individual/group)
· Use of the heart manual
Could also look into establishing links with GP, practice nurses, primary care team and chest pain services.
Gradual activity and low level exercise regime may commence once stable. Intensity will increase over a varying period of time depending on diagnosis and procedure and is done under guidance of the cardiologist
- <2 weeks post uncomplicated PCI
- 2 weeks post MI
- 3 weeks post cardiac surgery (Parker et al., 2011; Williams, 2006)
ACSM suggest 4-6 weeks post MI and post sternotomy unless otherwise directed by cardiologist/cardiothoracic surgeon
Phase III: Cardiac Rehabilitation and secondary prevention
Structured exercise training with continual educational and psychological support and advice on risk factors (SIGN, 2002)
Should take a menu based approach and be individually tailored.
Typically lasts at least 6 weeks with patients exercising 2/7 minimum.
Exercise class will consist of warm up, exercise class, cool down – may also include resistance training with active recovery stations where appropriate.
Phase III compromises of all the following;[edit | edit source]
· Exercise prescription based on
o Clinical status
o Risk Stratification
o Previous activity
o Future needs
· Education for patient and family re:
o Cardiac anatomy and physiology
o Recognition of cardiac pain and symptom management
o Risk factor identification and management
o Benefits of PA
o Energy conservation techniques/graded return to ADLs
o Cardio protective healthy eating
o Benefits and entitlements
· Stress management and relaxation techniques
· Counselling and behaviour modification
· Smoking cessation
· Vocational counselling (IACR, 2013)
Phase IV: Maintenance[edit | edit source]
Goal: facilitate long term maintenance of lifestyle changes, monitoring risk factor changes and secondary prevention.
Options:
- Educational sessions
- Support groups
- Telephone follow up
- Review in clinics
- Outreach programmes
- Phase IV exercise programme organised by qualified phase IV gym instructor
- Links with GP and primary health care team
- Ongoing involvement of partners/spouses/family
Resources[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 Pryor JA, Prasad SA. Physiotherapy for Respiratory and Cardiac Problems. Philadelphia: Elsevier Ltd, 4th Edition, 2008: 14 (470 - 494).
- ↑ Cardiac Rehabilitation Program. Available from: http://www.youtube.com/watch?v=famkb_dtAF0 (accessed 20 Oct 2013).
- ↑ Cardiac rehabilitation. Available from: http://www.pnmedycznych.pl/spnm.php?ktory=369 (accessed 22.12.2013)