Calf Strain
'Original Editors ' Kim De Maeght, Bettina Vansintjan, Maite Van Roozendael , Rewan aloush and Lenka Pé
Definition/Description[edit | edit source]
Calf strain is a common muscle injury. It is a tear of the muscle fibres of the muscles at the back of the lower leg. Strains are the result of excessive stretching or over stretching while the muscle is being activated. Strains may be referred to as a “pulled muscle”.
Clinically Relevant Anatomy[edit | edit source]
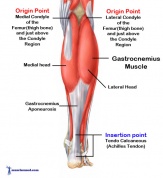
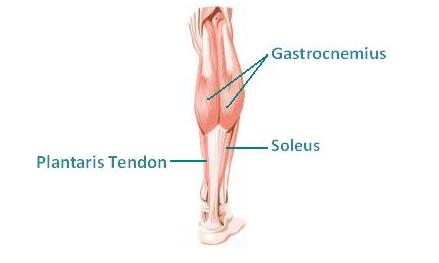
The calf muscle, on the back of the lower leg, is composed of three muscles: the gastrocnemius, the soleus and the plantaris, which together constitute the triceps surae. These muscles come together as the achilles tendon and all three muscles insert into the calcaneus.
Gastrocnemius is part of the posterior compartment of the leg and comprises of two parts, the medial head and the lateral head. The medial head arises from the medial condyle of the femur and the lateral head originates from the lateral condyle of the femur. [1] The gastrocnemius provides primarily plantar flexion and flexion at knee joint. [2] Gastrocnemius is innervated by the tibial nerve, a branch of the sciatic nerve, passing through the popliteal fossa where the nerve gives off a branch to the gastrocnemius.
Soleus is located beneath the gastrocnemius muscle in the superficial posterior compartment of the lower leg. The muscle originates from the upper 1/3 of the posterior aspect of the tibia, from the back of the head of the fibula and the upper part of the posterior surface of the fibular shaft and the fibrous arch that lies between the tibia and the fibula. [3] Its main function is plantar flexion of the ankle and stabilising the tibia on the calcaneus limiting forward sway. [2] The soleus is innervated by the tibial nerve, which passes behind the muscle through the fibrous arch of the soleus.
Plantaris is located in the posterosuperficial compartment of the calf. The muscle originates from the lateral supracondylar line of the femur (superior and medial to the lateral head of gastrocnemius) and from the oblique popliteal ligament. It is a long, small muscle with a long thin tendon. The plantaris is also innervated by the tibial nerve. Functionally, plantaris is not a major contributor and acts with gastrocnemius, as both a flexor of the knee and a plantarflexor of the ankle. [4]
Epidemiology/Etiology[edit | edit source]
Muscle strains most commonly occur in bi-articular muscles such as the hamstrings, rectus femoris and gastrocnemius. During sporting activities such as sprinting, these long, bi-articular muscles have to cope with high internal forces and rapid changes in muscle length and mode of contraction. However, muscle strains have also been reported to occur during slow-lengthening muscle actions such as those performed by ballet dancers, but also during common daily activities. [5] Gastrocnemius is considered at high risk for strains because it crosses two joints (the knee and ankle) and has a high density of type two fast twitch muscle fibres. [2] A tear of the medial head of the gastrocnemius muscle is due to an eccentric force being applied to the muscle when the knee is extended and the ankle is dorsiflexed. The gastrocnemius muscle attempts to contract in the already lengthened state leading to tear of the muscle. [6] The soleus muscle on the other hand is injured while the knee is in flexion. Strains of the proximal medial musculotendinous junction are the most common type of soleus muscle injuries. Unlike gastrocnemius, soleus is considered low risk for injury. It crosses only the ankle and is largely comprised of type one slow twitch muscle fibres. Soleus strains also tend to be less dramatic in clinical presentation and more subacute when compared to injuries of gastrocnemius. [2] This condition frequently occurs in the middle-aged, poorly conditioned and/or physically active patient. [7]
Symptoms[edit | edit source]
Symptoms of a calf strain can vary significantly but usually involve a sudden sharp pain at the back of the lower leg. The calf muscle will often be tender to touch at the point of injury and swelling and bruising may appear within hours or days.
Depending on how bad the calf injury is, the athlete may be able to continue exercising although he/she will often have some discomfort / tightness during or after the session. When injuries are more severe the athlete can recall when the injury occurred and or they may be unable to walk due to severe pain.
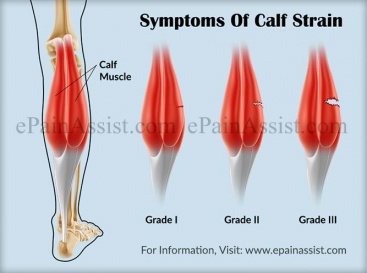
A calf muscle tear is graded from 1 to 3, with grade 3 being the most severe. A grade 1 will not normally need professional treatment whereas grade 2 or 3 injuries, depending on their severity, may require more specialist treatment and rehabilitation advice from a sports injury professional.
Grade 1 symptoms
A Grade 1 calf strain is a minor tear with up to 25% of the muscle fibres affected. The athlete may feel either a twinge of pain in the back of the lower leg or a feeling of "tightness". They may be able to carry on playing or competing without pain or with only mild discomfort in the calf. However, after exercises finishes there is likely to be "tightness" and/or aching in the calf muscles which can take up to 24 hours to develop.
Grade 2 symptoms
Symptoms of a Grade 2 strain will be more severe than a grade one, with up to 90% of the muscle fibres torn. There will be a sharp pain at the back of the lower leg and usually significant pain on walking afterwards. There is likely to be swelling in the calf muscle with mild to moderate bruising, however this may take hours or days to be visible. On strength testing the muscle, pain will be felt on resisted plantar flexion (pushing the toes and foot downwards towards the floor) against resistance. Tightness and aching may be present in the calf muscle for a week or more before subsiding.
Grade 3 symptoms
Grade 3 injuries involve 90-100% of the muscle fibres and are often referred to as "ruptures". The athlete will definitely be able to recall exactly when the injury occurred and this will be associated with severe immediate pain at the back of the lower leg. In these situations, the athlete will be unable to continue/finish exercising and will often be unable to walk due to weakness and pain. This level of injury also presents with considerable bruising and swelling although this may take hours to be visible. On strength testing, the athlete will be unable to even contract the calf muscle at all and in the case of a full rupture, a gap in the muscle can usually be felt. This is due to a deformity where the muscle is torn and the top part of the muscle may bunch up towards the top of the calf which is clearly visible.
Characteristics/Clinical Presentation[edit | edit source]
It is important to differentiate between muscle strains within the calf complex in order to formulate a correct prognosis, an appropriate treatment programme and prevention of recurrent injury. [8]
Gastrocnemius strains
Calf strains are most commonly found in the medial head of the gastrocnemius. [2] In an effort to contract, the forces of the eccentric movement on the already lengthened gastrocnemius muscle lead to injury at the myotendinous junction. The physical examination immediately after the injury reveals a palpable defect in the medial belly of the gastrocnemius just above the musculotendinous junction. [9] A sudden pain is felt in the calf, and the patient often reports an audible or palpable "pop" in the medial aspect of the posterior calf, or they have a feeling as though someone has kicked them in the back of the leg. Substantial pain and swelling usually develop during the following 24 hours. [1] Strains in the gastrocnemius are also referred to as a “tennis leg” as the classic presenttaion was a middle aged tennis player who suddenly extends the knee [2]
Soleus strains
Soleus is considered low risk for injury in contrast to the gastrocnemius asit crosses only the ankle and is largely composed of type one slow twitch muscle fibres. [2] Soleus strains tend to be less dramatic in clinical presentation and more subacute when compared to injuries of the gastrocnemius. Injury of the soleus muscle may be under reported due to a misdiagnosis of thrombophlebitis or lumping of soleus strains with strains of the gastrocnemius. [2] A soleus strain causes pain when activating the calf muscle or when applying pressure on the achilles tendon approximately 4 cm above the insertion point on the heel bone or higher up in the calf muscle. Stretching the tendon and walking on tip-toe will also aggravate pain. [10]
Plantaris strains
Plantaris is considered largely vestigial and rarely involved in calf strains, although it crosses both the knee and the ankle joint as well. [2] Rupture of the plantaris muscle may occur at the myotendinous junction with or without an associated hematoma or partial tear of the medial head of the gastrocnemius muscle or soleus. [4] Injury to the plantaris muscle can present with similar clinical features as those of the gastrocnemius and soleus muscle. [11]
Differential Diagnosis[edit | edit source]
Strains are most common during sporting activity, but pain in the lower leg could indicate medial tibial stress syndrome, achilles tendinitis, plantar fasciitis, muscles strains and/or joint sprains which can be caused by lack of extensibility of the plantar-flexors and decrease in ankle dorsiflexion. [12] The different degrees of muscle strains are discussed above. Other lower leg injuries related to sports with the same symptoms and treatment as a calf strain are discussed below.
Runners often complain about lower leg pain along the posteromedial border of the tibia. [13] This is medial tibial stress syndrome (MTSS) or commonly known as shin splints. [14] The pain is described as tenderness located a few centimetres proximal to the medial malleolus, spreading proximally about 4 to 10 centimetres. The cause of MTSS may be associated with repetitive stress or an overuse injury.
Pain located anterior or anteromedial of the tibia could indicate a tibial stress fracture, a typical injury seen in runners and footballers [14] [13] It can occur following abrupt changes in intensity, duration and frequency of training, but other personal and environmental factors can also contribute to this injury. Radiographs are initially negative, but with time fracture lines become visible. Operative treatment may occasionally be necessary, but it can be treated the same way as a calf strain: rest, restriction from aggravating activity, strengthening of the lower extremity musculature, NSAIDs and appropriate footwear.[11]
Repetitive exercise without adequate rest for recovery can cause chronic exertional compartment syndrome (CECS). [14] CECS begins with mild pain during periods of training and can disappear after training. In the latter stages, pain presents earlier, becoming more painful and of a greater duration forcing a halt in activity. Common complaints are; cramps, paraesthesia, numbness and weakness in the lower leg. CECS is caused by the increased intramuscular blood flow during exercise so compartmental pressure arises, capillaries become compressed and ischemia develops.
Leg pain around the same area as a gastrocnemius strain can be caused by Popliteal Artery Entrapment Syndrome (PAES), an abnormal course of the popliteal artery. Medial and cranial migration of the medial head of the gastrocnemius can catch the popliteal artery and swipe it medially. This is called anatomical PAES, an abnormal relationship between the popliteal artery and the surrounding myofascial structures. Functional PAES is caused by muscle contraction, often active plantarflexion of the ankle that compresses the artery between the muscle and underlying bone. [15] See http://www.physio-pedia.com/Posterior_Knee_Pain
See also:
Achilles tendinopathy
Plantar fasciitis
Diagnostic Procedures[edit | edit source]
A thorough clinical examination and history may be enough to conclude a diagnosis, but it is often difficult to reach an accurate diagnosis due to the clinical being shared with other pathological conditions. Diagnostic imaging is usually necessary and ultrasound (US) is considered to be the gold standard. It can also be used to evaluate the degree and extent of the muscular lesion and to exclude other pathologies such as ruptured Baker's cyst and deep vein thrombosis. [16]
Ruptures are usually associated with the presence of fluid collection between the soleus muscle and the medial head of the gastrocnemius. This can occur with or without hemorrhage. The measurement of fluid collection gives us information about the extent of the lesion. The degree of the lesion (partial or complete rupture) can be defined by the distance between the two muscles. Axial US scans are the most useful for differentiating between partial and complete rupture, as it is possible to depict the whole muscle belly in one single image. [1]
A calf muscle tear is a most common injury in sports such as running, volleyball, tennis, etc. These sports require quick acceleration of changes in direction and are more susceptible for a calf strain injury. Muscle strains are graded as mild, moderate and severe. The more severe the strain, the longer the recovery time. Typical symptoms are stiffness, discoloration and bruising around the strained muscle. [10]
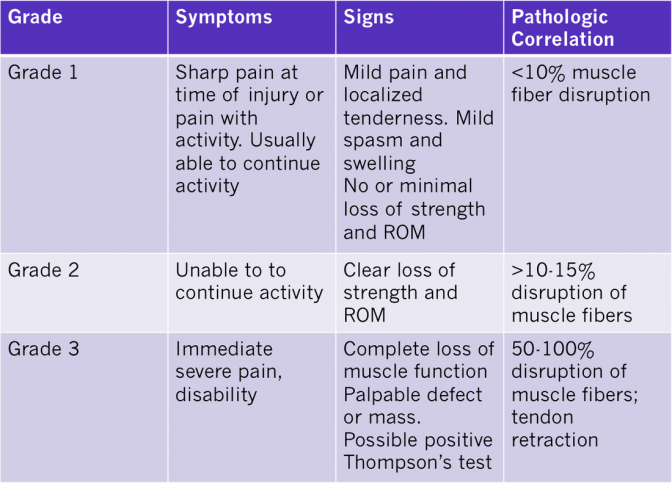
Grade I:
A first degree or mild injury is the most common and the most minor. A sharp pain is felt at the time of injury or pain with activity. There is little to no loss of strength and range-of-motion with muscle fibre disruption of less than 10%. A return to sport would be expected within 1 to 3 weeks. [13]
Grade II:
A second degree or moderate injury is a partial muscle tear halting activity. There is a clear loss of strength and range of motion. [13] with marked pain, swelling and often bruising. Muscle fibre disruption between 10 and 50%. 3 to 6 weeks is a usual recovery period for a return to full activity. [10]
Grade III:
A third degree or severe injury results in a complete rupture of the muscle and is often concomitant with a hematoma. [13] Pain, swelling, tenderness and bruising are usually present. Recovery is highly individualised and can take months before you are fully recovered for a full return to activity. [10]
Outcome Measures[edit | edit source]
- LEFS: Lower Extremity Functional Scale
- VAS: Visual Analogue Scale
- NPRS: Numeric Pain Rating Scale
- Muscle Strength testing: grade 0 is the lowest grade where the patient isn’t capable of doing any contraction of the muscle. Grade 5 is the highest grade where the patient is able to move his leg against a maximum resistance given by the therapist.
Examination[edit | edit source]
The physical exam isolates the site and severity of the injury. A combination of palpation, strength testing, and passive and active range of motion is necessary to help distinguish between strains of the soleus and gastrocnemius muscle.
Palpation of the calf should occur along the entire length of the muscles and the aponeuroses. This is required to identify swelling, thickening, tenderness, defects and masses if present. Strains of the gastrocnemius muscle usually present with tenderness in the medial belly or musculotendinous junction, while soleus strains often occur with lateral pain.
There are multiple techniques that exist to assess calf strains.
Considering that the origin of the gastrocnemius is situated above the knee (epicondylus lateralis and medialis femoris) and the origin of the soleus finds itself below the knee (caput fibulae), it allows the therapist to isolate the activation of the muscles by varying the degree of knee flexion. The soleus becomes the main source of force in plantar flexion, with the knee in maximal flexion. On the contrary, when the knee is in full extension, it is the gastrocnemius who provides most strength. This relationship allows for more accurate strength testing of the individual calf muscles and enables the examiner to describe which muscle has been injured.
Another similar method is used to test flexibility and pain during stretching and passive ankle movements. This technique determines the site of injury by isolating the gastrocnemius and soleus muscle. During the test, the knee is placed in maximal extension and thereafter in flexion while the ankle is passively dorsiflexed. This causes isolated stretch of the gastrocnemius and the soleus otherwise.
Additional testing that can be used includes the Thompson test for complete disruption of the achilles tendon. Simultaneous tears of the gastrocnemius and soleus are possible, which can complicate the clinical picture. [17] [18]
Observation[edit | edit source]
- Observation is usually the first point of any injury assessment.
- The therapist usually observes the patient in both standing and laying positions, looking closely for swelling, bruising and deformity, as well as postural issues such as overpronation
- https://www.youtube.com/watch?v=sn6a0X8oXhg&feature=youtu.be
Medical Management[edit | edit source]
Calf strains rarely require surgery, but is carried out in extreme cases. such as in a complete rupture. Recommended conservative management includes RICE, injection of local anesthetic and cortisone in and around the area [3] and graded and active recovery treatment. Where a hematoma is present, its removal as quickly as possible is essential, otherwise complications may occur such as myositis ossificans.
Prevention:
Regular stretching ensures that good joint mobility is maintained. [1] Under extension, a greater force can also be delivered and the muscles are less tense, improving blood flow. [19] [4] Stretching is easy to perform and has a low risk of side effects. [1]
Self Help Treatment[edit | edit source]
Applying P.R.I.C.E. (Protection Rest, Ice, Compression, Elevation) is essential. Apply a cold therapy and compression wrap as soon as possible to help stop any internal bleeding. Cold therapy can be applied for 10 to 15 minutes every hour initially reducing frequency as pain and swelling goes down. Do not apply ice directly to the skin as it can cause ice burns. Read more about P.R.I.C.E.
It is advised to use a compression bandage, calf support or sleeve. A compression bandage can be applied immediately to help stop swelling but it should only be applied for 10 minutes at a time as restricting blood flow completely to the tissues could cause more damage, whereas the calf supports can be applied for longer.
We also advise wearing a heel pad to raise the heel and shorten the calf muscle hence taking some of the strain off the muscle. It is a good idea to put heel pads in both shoes because otherwise one leg will become longer than the other due to the raised heel thereby creating an imbalance and possibly leading to other associated injuries / pain (e.g. in the back).
For more comprehensive treatment and to minimise the risk of re-injury, Sportsinjuryclinic.net advise seeing a professional therapist (such as physiotherapist, sports therapist, osteopath or chiropractor) who can also devise a full calf strain rehabilitation program including stretching and strengthening exercises.
Calf Strain Rehabilitation[edit | edit source]
A structured rehabilitation program is important for optimum recovery from a calf strain. We outline an example of a calf strain rehab schedule below for grade 1,2 and 3 injuries.
This rehabilitation programme is intended as a guide only. We recommed seeking professional advice before carrying out any form of exercise. All timelines are given as an indication only.
Grade 1 calf strain[edit | edit source]
(A minor tear with up to 10% of the muscle fibres involved)
Stage 1: Days 0 from time of injury
Rest as much as possible. Ice - this should be applied for 15 minutes every 2-3 hours. Make sure you wrap the ice in a wet towel to prevent skin burns. Compression - apply a compression bandage, calf support or elastic tubi-grip type bandage to help reduce swelling and bleeding.
Elevation - put your feet up and read about treatment and rehabilitation of your injury. Elevating the leg will help swelling and blood run away from the injured muscle.
Stage 2: Days 3 since injury
If it is comfortable do Calf strain stretching exercises very gently, 3-5 times a day.
Start with active stretching and if an exercise is painful do not do it. Visit a sports massage therapist who can perform calf strain sports massage techniques. Electrotherapy such as ultrasound may also be beneficial in reducing swelling and relaxing the muscle. Continue to rest from any aggravating activities. Continue to wear a compression bandage or calf support.
Stage 3: Days 7 since injury
Continue to stretch on a daily basis. A calf stretcher is a useful piece of kit to aid the stretching the calf muscle in the later stages of rehabilitation. Continue with sports massage as necessary.
As the muscle gets stronger then massage techniques will become deeper and the time between treatments longer. Begin calf strain strengthening exercises.
Resistance bands can be used initially, followed by calf raises and then eventually single leg calf raises. Remember not to do any exercises if they are painful. Once you can acheive 3 sets of 20 single leg calf raises, pain-free gradually incorporate running into the rehab program. Eventually plyometrics or hopping exercises should be done to return to full match fitness and prevent the injury recurring.
Grade 2 injury[edit | edit source]
(A more severe tear involving up to 90% of the muscle fibres)
Stage 1: Days 0
Rest as much as possible - use crutches if necessary. Ice - this should be applied for 15 minutes every 2-3 hours. Make sure you wrap the ice in a wet towel to prevent skin burns. Compression - apply a compression bandage or tubi-grip bandage to help reduce swelling and bleeding.
Elevation - put you feet up and read about treatment and rehabilitation of your injury. Elevating the leg will help swelling and blood run away from the injured muscle. Once it is comfortable to do so, perform some active stretches - pull your toes towards you, hold for 2-3 seconds and then relax and repeat 10-20 times. If you are walking, try using heel pads to temporarily shorten the calf muscles and take the strain off them.
Stage 2: Days 7
Continue to wear the compression bandage. Continue to rest from any aggravating activities.
If it is comfortable to do so try to gently stretch both calf muscles 3-5 times a day. Instead of icing, try alternating hot and cold for 5 minutes each, for 20-30 minutes 3 times a day. Visit a sports injury professional for a sports massage. Electrotherapy may also be beneficial.
Stage 3: Days 14
Start to gently strengthen the calf muscles if it is comfortable to do so. Start with resistance band plantarflexion and progress to calf raises and then single leg calf raises. Continue to stretch regularly. Continue with sports massage if necessary. Gradually incorporate some running into your program once you can acheive 3 sets of 20 single leg calf raises, pain-free!
Grade 3 injury[edit | edit source]
(Usually a very severe strain or complete rupture of the muscle)
Stop playing and rest immediately. If you are concerned that the muscle may be ruptured, go straight to a Doctor or Hospital. If the muscle is ruptured or there is considerable damage the usual treatment involves an operation to repair the muscle. If the muscle is not completely torn,follow a grade 2 program.
Physical Therapy Management[edit | edit source]
Treatment aims to:
- Reduce pain
- Restore flexibility
- Restore strength
The principal treatment of a calf strain consists of rest and allowing adequate healing time, but in severe cases, surgery is necessary. Conservative treatment includes passive stretching, isometric then concentric exercises. [3] In the latter stages, teatment can move onto massage and electrotherapy. [4]
Initial treatment aims to limit bleeding, pain and to prevent complications, such as rest, ice, compression and elevation. [2]Cryotherapy can be used to decrease inflammation, pain and cell metabolism. Tape or a compressive wrap can be applied and the leg elevated. [3] If major bleeding had occurred, the use of NSAIDs has to be carefully controlled as they have an antiplatelet effect which can increase bleeding, just as the premature application of heat and massage also can. [2]
Gentle passive stretching exercises without pain promote range of motion of the plantar flexors, which is limited by shortnening and contractures. [19] Applying superficial heat simultaneously with a low load static stretch improves the flexibility of muscles. [3]
Isotonic exercises for the antagonists tibialis anterior, and the peronei are recommended as well as light exercises for the injured muscle. The process of stretching and exercises is carried out 2 to 3 times in the first 3 days after injury. [3] Lack of extensibility of the plantar flexors can cause decreases in ankle dorsiflexion and disturbances in gait. Shoes with a low heel are recommended to encourage improved heel-toe gait. [19]
After 48 hours, ice is no longer an effective analgesic. short wave diathermy can be used as an alternative. A strain with abnormal swelling and bruising can be treated with interferential therapy. The aim is to relieve pain and to stimulate the muscle fibres. [3]
When the calf muscles can be fully extended, the switch from passive stretching to a standing stretch can be made, either in a flexed knee position (soleus) or a straightened knee position (gastrocnemius). [3]
After approximately 10 days isometric, isotonic and dynamic exercises to improve tensile strength can be performed. [2] Alternative treatments consist of vibration therapy (VT). Vibration therapy is applied specifically to the area of injury and treats muscle strains and other myo-tendinous injuries which involve trigger points. [4] Broadbent et al. suggested that VT stimulates the sensory receptors, but it also causes a decrease in inflammatory cells and receptors like IL6 and histamine. [20] The aim of this therapy is an increase in muscle strength, flexibility and extensibility. After a VT treatment, however, jumping and running are not permitted for at least 3 to 6 weeks and NSAIDS are discouraged, but other treatment routines can be continued. An advantage compared with other therapies like sound wave therapy and ESWT treatments, is that VT can be applied more frequently. [21]
Strains may cause long lasting pain, despite an adequate early treatment. The average time of treatment is nine days. Treatment outcome is successfully when: pain is resolved, the calf muscle can be fully extended, strength is back to normal, knee and ankle ROM are normal and when excessive tenderness has disappeared. [3]
Key Research[edit | edit source]
Millar, A. P., “Strains of the posterior calf musculature ("tennis leg")*.”The American Journal of Sports Medicine, vol. 7, no. 3, 1979, pp. 172-174.
Ellen, Mark I., Jeffrey L. Young, and James L. Sarni. "3. Knee and lower extremity injuries." Archives of physical medicine and rehabilitation 80.5 (1999): S59-S67.
Bryan Dixon J. Gastrocnemius vs. soleus strain: how to differentiate and deal with calf muscle injuries. Current Reviews in Musculoskeletal Medicine. 2009;2(2):74-77.
Clinical Bottom Line[edit | edit source]
Pain in the calf muscle is often due to a strain, however, there are other conditions which could cause similar symptoms, including deep vein thrombosis and contusions. Treatment of muscle injuries usually has good outcome. Healing time is hugely variable depending on the severity of the strain. Conservative management of stretching and exercises usually have the required outcome, but surgery may be required in the case of a rupture. Massage of the calf muscles, ultrasound and electrical stimulation are also effective treatments.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Kwak H-S, Han Y-M, Lee S-Y, Kim K-N, Chung GH. Diagnosis and Follow-up US Evaluation of Ruptures of the Medial Head of the Gastrocnemius (“Tennis Leg”). Korean Journal of Radiology. 2006;7(3):193-198.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 Bryan Dixon J. Gastrocnemius vs. soleus strain: how to differentiate and deal with calf muscle injuries. Current Reviews in Musculoskeletal Medicine. 2009;2(2):74-77.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 Pedret C, Rodas G, Balius R, et al. Return to Play After Soleus Muscle Injuries. Orthopaedic Journal of Sports Medicine. 2015;3(7)
- ↑ 4.0 4.1 4.2 4.3 4.4 Spina AA. The plantaris muscle: anatomy, injury, imaging, and treatment. The Journal of the Canadian Chiropractic Association. 2007;51(3):158-165.
- ↑ Marc Roig Pull and Craig Ranson, Eccentric muscle actions: Implications for injury prevention and rehabilitation, Physical Therapy in Sport 8 (2007), no. 2, 88 – 97.
- ↑ Watura C, Harries W. Isolated tear of the tendon to the medial head of gastrocnemius presenting as a painless lump in the calf. BMJ Case Reports. 2009
- ↑ Flecca D, Tomei A, Ravazzolo N, Martinelli M, Giovagnorio F. US evaluation and diagnosis of rupture of the medial head of the gastrocnemius (tennis leg). Journal of Ultrasound. 2007;10(4):194-198.
- ↑ Bryan Dixon J. Gastrocnemius vs. soleus strain: how to differentiate and deal with calf muscle injuries. Current Reviews in Musculoskeletal Medicine. 2009;2(2):74-77. doi:10.1007/s12178-009-9045-8. [L1b]
- ↑ Nsitem V. Diagnosis and rehabilitation of gastrocnemius muscle tear: a case report. The Journal of the Canadian Chiropractic Association. 2013;57(4):327-333.`
- ↑ 10.0 10.1 10.2 10.3 Ellen, Mark I., Jeffrey L. Young, and James L. Sarni. "3. Knee and lower extremity injuries." Archives of physical medicine and rehabilitation 80.5 (1999): S59-S67.
- ↑ 11.0 11.1 Meininger, Alexander K., and Jason L. Koh. "Evaluation of the injured runner." Clinics in sports medicine 31.2 (2012): 203-215.
- ↑ Knight CA., et al. (juni 2001). “Effect of Superficial Heat, Deep Heat, and Active Exercise Warm-up on the Extensibility of the Plantar Flexors.” Physical Therapy, Vol 81 (6), pp. 1206-1214.
- ↑ 13.0 13.1 13.2 13.3 13.4 Nsitem V. Diagnosis and rehabilitation of gastrocnemius muscle tear: a case report. The Journal of the Canadian Chiropractic Association. 2013;57(4):327-333.`
- ↑ 14.0 14.1 14.2 Ellen, Mark I., Jeffrey L. Young, and James L. Sarni. "3. Knee and lower extremity injuries." Archives of physical medicine and rehabilitation 80.5 (1999): S59-S67.
- ↑ Stager, Andrew, and Douglas Clement. "Popliteal artery entrapment syndrome." Sports Medicine 28.1 (1999): 61-70.
- ↑ Flecca D, Tomei A, Ravazzolo N, Martinelli M, Giovagnorio F. US evaluation and diagnosis of rupture of the medial head of the gastrocnemius (tennis leg). Journal of Ultrasound. 2007;10(4):194-198
- ↑ Marc Roig Pull and Craig Ranson, Eccentric muscle actions: Implications for injury prevention and rehabilitation, Physical Therapy in Sport 8 (2007), no. 2, 88 – 97.
- ↑ Bryan Dixon J. Gastrocnemius vs. soleus strain: how to differentiate and deal with calf muscle injuries. Current Reviews in Musculoskeletal Medicine. 2009;2(2):74-77.
- ↑ 19.0 19.1 19.2 Bartholdy, Cecilie, et al. "Local and Systemic Changes in Pain Sensitivity After 4 Weeks of Calf Muscle Stretching in a Nonpainful Population: A Randomized Trial." Pain Practice (2015).
- ↑ Broadbent, Suzanne, et al. "Vibration therapy reduces plasma IL6 and muscle soreness after downhill running." British journal of sports medicine 44.12 (2010): 888-894.
- ↑ Saxena, Amol, Marie St Louis, and Magali Fournier. "Vibration and pressure wave therapy for calf strains: a proposed treatment." Muscles, ligaments and tendons journal 3.2 (2013): 60. [L1a]