Breathing Pattern Disorders
Original Editor - Your name will be added here if you created the original content for this page.
Top Contributors - Rachael Lowe, Leon Chaitow, Admin, Kim Jackson, Jess Bell, Ewa Jaraczewska, Wanda van Niekerk, Khloud Shreif, Tarina van der Stockt, Fasuba Ayobami, WikiSysop, Lucinda hampton, 127.0.0.1, Ajay Upadhyay, Marleen Moll, Olajumoke Ogunleye, Evan Thomas, Scott Buxton and Venus Pagare
Introduction[edit | edit source]
Breathing Pattern Disorders (BPD) (or Dysfunctional Breathing) are abnormal respiratory patterns in relation to overbreathing which ranges from simple upper chest breathing to, at the extreme end of the scale, hyperventilation. Dysfunctional breathing (DB) is defined as chronic or recurrent changes in breathing pattern that cannot be attributed to a specific medical diagnosis, causing respiratory and non-respiratory complaints. This is not a disease process, simply alterations in breathing patterns that interfere with normal respiratory processes. They can however, co-exist with disease such as COPD or heart disease.
BPDs are whole person problems, especially in long term conditions where dysfunctional breathing can destabilise mind and muscles, mood and metabolism[1]. They can play a part in, for instance, chronic fatigue[2], pain, fibromyalgia and some aspects of anxiety and depression.
Clinically Relevant Anatomy[edit | edit source]
add text here relating to clinically relevant anatomy of the condition
Epidemiology[edit | edit source]
It is often reported that around 10% of patients in a population are diagnosed hyperventilation syndrome[3]. However, far more people have a more subtle, yet likely clinically significant, breathing pattern disorder. Dysfunctional breathing is more prevalent in women (14%) than in men (2%)[3]
Etiology
[edit | edit source]
Breathing pattern disorders involve being in a constant state of inhalation. This leads to hypocapnia - the deficiency of carbon dioxide in the blood due to hyperventilation - leading to respiratory alkalosis, and eventually hypoxia or the reduction of oxygen to tissue.[4] [5] This is commonly seen in chest breathers, that essentially never fully exhale in order to utilise full lung capacity.
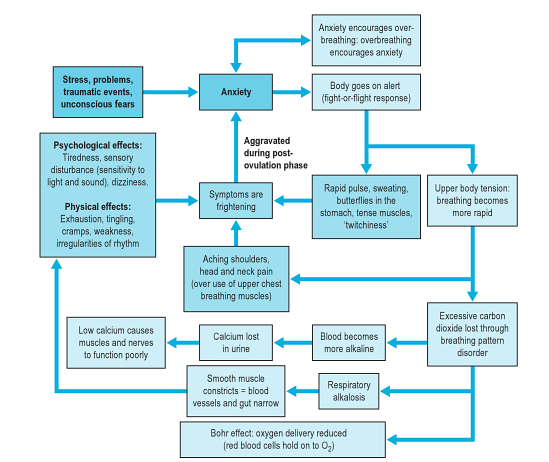
As well as having a marked effect on the biochemistry of the body BPD can influence emotions, circulation, digestive function as well as musculoskeletal structures involved in the respiratory process. Essentially a sympathetic state and a subtle, yet fairly constant state of fight-or-flight becomes prevalent. This can lead to changes in anxiety, blood pH, muscle tone, pain threshold, and many central and peripheral nervous system symptoms. So, despite not being a disease, BPDs are capable of producing symptoms that mimic pathological processes. For example, overuse of accessory breathing muscles can lead to neck and shoulder pain/dysfunction. Some even mimic cardiac and gastrointestinal problems.
This diagram (from [6]) shows the stress-anxiety-breathing flow chart demonstrating multiple possible effects and influences of breathing pattern disorders.
Clinical Presentation[edit | edit source]
There are a wide variety of symptoms, the most extreme as shown in the diagram below:
Typical symptoms can include:
- Frequent sighing and yawning
- Breathing discomfort
- Disturbed sleep
- Erratic heartbeats
- Feeling anxious and uptight
- Pins and needles
- Upset gut/nausea
- Clammy hands
- Chest Pains
- Shattered confidence
- Tired all the time
- Achy muscles and joints
- Dizzy spells or feeling spaced out
- Irritability or hypervigilance
- Feeling of 'air hunger'
- Breathing discomfort
Diagnostic Procedures[edit | edit source]
Nijmegan questionnaire[edit | edit source]
High scores on the Nijmegan questionnaire have been shown to be both sensitive and specific for detecting people with tendencies consistent with breathing pattern disorders. The sensitivity of the Nijmegen Questionnaire in relation to the clinical diagnosis was 91% and the specificity 95%[7]
Assessment of breathing patterns
[edit | edit source]
- Breath Holding – People can normally hold their breath between 25 and 30 seconds. If less than 15 seconds may mean low tolerance to carbon dioxide.
- Breathing Hi-Low Test (seated or supine) – Hands on chest and stomach, breathe normal – what moves first? What moves most? Looking for lateral expansion and upward hand pivot.
- Breathing Wave – Lay prone, breathe normal, spine should flex in a wave-like pattern towards head. Segments that rise as a group may represent thoracic restrictions.
- Seated Lateral Expansion – Place hands on lower thorax and monitor motion while breathing. Looking for symmetrical lateral expansion.
Assessment of musculoskeletal system[edit | edit source]
- elevated and depressed ribs and clavicle.
- muscle tone and length especially psoas, QL, latissimus, upper trap, scalene, and SCM.
- alterations in mobility of thoracic and rib articulations.
Assessment of respiratory function[edit | edit source]
- Oximetry - to measure oxygen saturation (SpO2)
- Capnography - to measure end tidal CO2 levels in exhaled air
- Peak expiratory flow rate - the highest flow of air out of the lungs from peak inspiration in a fast single forced breath out
Outcome Measures[edit | edit source]
- Nijmegen Questionnaire
- Rowley Breathing Self-Efficacy Scale (RoBE)
- Self Evaluation of Breathing Questionnaire )SEBQ)
- Hospital Anxiety and Depression Questionnaire (HAD)
Management / Interventions
[edit | edit source]
Management commonly requires the removal of causative factors and the rehabilitation of habitual acquired dysfunctional breathing patterns. In order to achieve this most efficiently it may be necessary to restore normal function of the respiratory system such as thoracic mobility and muscle tone and length.
Manual Therapy Techniques[edit | edit source]
Based on your assessment, there are several manual therapy techniques that can be performed to treat muscles that have increased tone or activity, elevated and depressed ribs and alterations in mobility of thoracic articulations. These techniques include muscle energy techniques (MET), positional release, trigger point release and integrated neuromuscular inhibition techniques[6].
Breathing Retraining[edit | edit source]
- Awareness of faulty breathing patterns
- Relaxation of the jaw, upper chest, shoulderss and accesssory muscles
- Abdominal/low-chest nose breathing pattern reeducation
- Awareness of normal brething rates and rhythms, both at rest, during speech and activity.
Respiratory Techniques[edit | edit source]
- Pursed lip breathing has been shown to relieve dysponia, slow respiratory rate, increase tidal volume, and restore diaphragmatic function.
- Dynamic Neuromuscular Stabilisation - to optimise a postural respiratory pattern[6]
Complimentary methods[edit | edit source]
- Sleep retraining
- Relaxation
- Nutrition
- Capnography
Differential Diagnosis
[edit | edit source]
BPDs can often mimic more serious conditions such as cardiac, neurological and gastrointestinal conditions which must all be ruled out by the medical team.
Key Evidence[edit | edit source]
Breathing pattern disorders and functional movement. Bradley H, Dr Esformes J. Int J Sports Phys Ther. 2014 Feb;9(1):28-39.
Breathing exercises for dysfunctional breathing/hyperventilation syndrome in children. Barker NJ, Jones M, O'Connell NE, Everard ML.
Cochrane Database Syst Rev. 2013 Dec 18;12:CD010376.
Breathing exercises for dysfunctional breathing/hyperventilation syndrome in adults. Jones M, Harvey A, Marston L, O'Connell NE.
Cochrane Database Syst Rev. 2013 May 31;5:CD009041.
Related pages[edit | edit source]
Low Back Pain and Breathing Pattern Disorders
Resources[edit | edit source]
- Leon Chaitow's website
- Website containing videos to go with the book - Recognizing and Treating Breathing Pattern Disorders[6]
- Clinical interest group for physiotherapists interested in hyperventilation
| Reconizing and Treating Breathing Disorders
This book is all about Breathing Pattern Disorders. It is intended to help practitioners understand the causes and effects of disordered breathing and to provide strategies and protocols to help restore normal function. It is the perfect complimentary reading to this page. Purchase with discount |
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1-ohVP9Y35PejK1jrUNpTuyNlOE7GEihimykUGaQZ8jTQ14ETo|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
- ↑ Peters, D. Foreword In: Recognizing and Treating Breathing Disorders. Chaitow, L., Bradley, D. and Gilbert, C. Elsevier, 2014
- ↑ Nixon P, Andrews J. 1996 A study of anaerobic threshold in chronic fatigue syndrome (CFS). Biol Psychol. 43:264
- ↑ 3.0 3.1 Thomas M1, McKinley RK, Freeman E, Foy C, Price D.The prevalence of dysfunctional breathing in adults in the community with and without asthma. Prim Care Respir J. 2005 Apr;14(2):78-82. Cite error: Invalid
<ref>tag; name "Thomas" defined multiple times with different content - ↑ Biff F. Palmer 2012 Evaluation and Treatment of Respiratory Alkalosis Am J Kidney Dis. 60(5):834-838.
- ↑ Jensen F 2004 Red blood cell pH, the Bohr effect, and other oxygenation-linked phenomena in blood O2 and CO2 transport Acta Physiologica Scandinavica 182(3):215-227
- ↑ 6.0 6.1 6.2 6.3 Chaitow, L., Bradley, D. and Gilbert, C. Recognizing and Treating Breathing Disorders. Elsevier, 2014
- ↑ van Dixhoorn J, Duivenvoorden HJ. Efficacy of Nijmegen Questionnaire in recognition of the hyperventilation syndrome. J Psychosom Res. 1985;29(2):199-206.