Breathing Pattern Disorders
Original Editor - Your name will be added here if you created the original content for this page.
Top Contributors - Rachael Lowe, Leon Chaitow, Admin, Jess Bell, Ewa Jaraczewska, Kim Jackson, Khloud Shreif, Tarina van der Stockt, Wanda van Niekerk, Fasuba Ayobami, Lucinda hampton, 127.0.0.1, Ajay Upadhyay, WikiSysop, Marleen Moll, Olajumoke Ogunleye, Evan Thomas, Scott Buxton and Venus Pagare
Introduction[edit | edit source]
Breathing Pattern Disorders (BPD) are abnormal respiratory patterns. They range from simple upper chest breathing to, at the extreme end of the scale, hyperventilation. This is not a disease process, simply alterations in breathing patterns that interfere with normal respiratory processes. They can however, co-exist with disease such as COPD or heart disease.
BPDs are whole person problems, especially in long term conditions where dysfunctional breathing can destabilise mind and muscles, mood and metabolism[1]. They can play a part in, for instance, chronic fatigue, pain, fibromyalgia and some aspects of anxiety and depression.
Clinically Relevant Anatomy[edit | edit source]
add text here relating to clinically relevant anatomy of the condition
Epidemiology[edit | edit source]
It is often reported that around 10% of patients in a population are diagnosed hyperventilation syndrome. However, far more people have a more subtle, yet likely clinically significant, breathing pattern disorder. Dysfunctional breathing is more prevalent in women (14%) than in men (2%)[2]
Etiology
[edit | edit source]
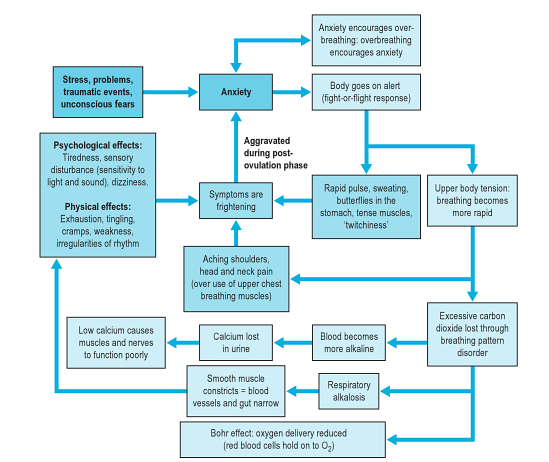
Breathing pattern disorders involve being in a constant state of inhalation. This leads to hypocapnia - the deficiency of carbon dioxide in the blood due to hyperventilation - leading to respiratory alkalosis, and eventually hypoxia or the reduction of oxygen to tissue. As well as having a marked effect on the biochemistry of the body BPD can influence emotions, circulation, digestive function as well as musculoskeletal structures involved in the respiratory process. This diagram (from [3]) shows the stress-anxiety-breathing flow chart demonstrating multiple possible effects and influences of breathing pattern disorders.
Despite not being a disease, BPDs are capable of producing symptoms that mimic pathological processes. For example, overuse of accessory breathing muscles can lead to neck and shoulder pain/dysfunction.
Clinical Presentation[edit | edit source]
There are a wide variety of symptoms, the most extreme
Diagnostic Procedures[edit | edit source]
add text here relating to diagnostic tests for the condition
Outcome Measures[edit | edit source]
Nijmegen Questionnaire
Management / Interventions
[edit | edit source]
Management commonly requires the removal of causative factors and the rehabilitation of habitual acquired dysfunctional breathing patterns. In order to achieve this most efficiently it may be necessary to restore normal function of the respiratory system such as thoracic mobility and muscle tone and length.
Differential Diagnosis
[edit | edit source]
add text here relating to the differential diagnosis of this condition
Key Evidence[edit | edit source]
add text here relating to key evidence with regards to any of the above headings
Resources
[edit | edit source]
add appropriate resources here
Case Studies[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
Recent Related Research (from Pubmed)[edit | edit source]
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ Peters, D. Foreword In: Recognizing and Treating Breathing Disorders. Chaitow, L., Bradley, D. and Gilbert, C. Elsevier, 2014
- ↑ Thomas, M., McKinley, R.K., Freeman, E., et al. The prevalence of dysfunctional breathing in adults in the community with and without asthma. Prim Care Respir J, 2005, 14, 78-82
- ↑ Chaitow, L., Bradley, D. and Gilbert, C. Recognizing and Treating Breathing Disorders. Elsevier, 2014