Breathing Pattern Disorders: Difference between revisions
Rachael Lowe (talk | contribs) No edit summary |
Rachael Lowe (talk | contribs) No edit summary |
||
| Line 94: | Line 94: | ||
== Differential Diagnosis<br> == | == Differential Diagnosis<br> == | ||
BPDs can often mimic more serious conditions such as cardiac conditions, gastrointestinal co<br> | |||
== Key Evidence == | == Key Evidence == | ||
Revision as of 12:45, 25 March 2014
Original Editor - Your name will be added here if you created the original content for this page.
Top Contributors - Rachael Lowe, Leon Chaitow, Admin, Kim Jackson, Jess Bell, Ewa Jaraczewska, Tarina van der Stockt, Wanda van Niekerk, Khloud Shreif, Fasuba Ayobami, WikiSysop, Lucinda hampton, 127.0.0.1, Ajay Upadhyay, Marleen Moll, Olajumoke Ogunleye, Evan Thomas, Scott Buxton and Venus Pagare
Introduction[edit | edit source]
Breathing Pattern Disorders (BPD) are abnormal respiratory patterns. They range from simple upper chest breathing to, at the extreme end of the scale, hyperventilation. This is not a disease process, simply alterations in breathing patterns that interfere with normal respiratory processes. They can however, co-exist with disease such as COPD or heart disease.
BPDs are whole person problems, especially in long term conditions where dysfunctional breathing can destabilise mind and muscles, mood and metabolism[1]. They can play a part in, for instance, chronic fatigue, pain, fibromyalgia and some aspects of anxiety and depression.
Clinically Relevant Anatomy[edit | edit source]
add text here relating to clinically relevant anatomy of the condition
Epidemiology[edit | edit source]
It is often reported that around 10% of patients in a population are diagnosed hyperventilation syndrome. However, far more people have a more subtle, yet likely clinically significant, breathing pattern disorder. Dysfunctional breathing is more prevalent in women (14%) than in men (2%)[2]
Etiology
[edit | edit source]
Breathing pattern disorders involve being in a constant state of inhalation. This leads to hypocapnia - the deficiency of carbon dioxide in the blood due to hyperventilation - leading to respiratory alkalosis, and eventually hypoxia or the reduction of oxygen to tissue. This is commonly seen in chest breathers, that essentially never fully exhale and utilise all of their lung capacity.
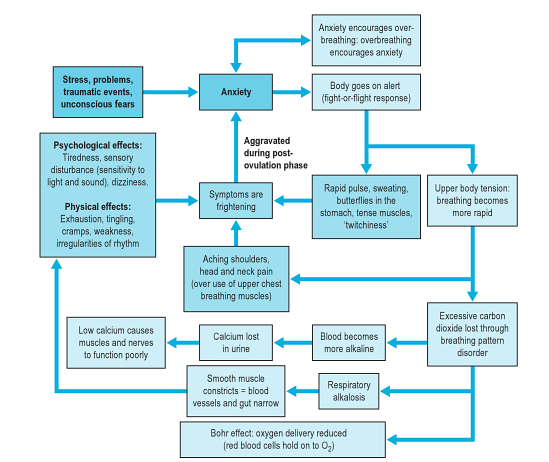
As well as having a marked effect on the biochemistry of the body BPD can influence emotions, circulation, digestive function as well as musculoskeletal structures involved in the respiratory process. Essentially a sympathetic state and a subtle, yet fairly constant state of fight-or-flight becomes prevalent. This can lead to changes in anxiety, blood pH, muscle tone, pain threshold, and many central and peripheral nervous system symptoms. So, despite not being a disease, BPDs are capable of producing symptoms that mimic pathological processes. For example, overuse of accessory breathing muscles can lead to neck and shoulder pain/dysfunction. Some even mimic cardiac and gastrointestinal problems.
This diagram (from [3]) shows the stress-anxiety-breathing flow chart demonstrating multiple possible effects and influences of breathing pattern disorders.
Clinical Presentation[edit | edit source]
There are a wide variety of symptoms, the most extreme as shown in the diagram below:
Diagnostic Procedures[edit | edit source]
Nijmegan questionnaire[edit | edit source]
High scores on the Nijmegan questionnaire have been shown to be both sensitive and specific for detecting people with tendencies consistent with breathing pattern disorders.
Assessment of breathing patterns
[edit | edit source]
- Breath Holding – People can normally hold their breath between 25 and 30 seconds. If less than 15 seconds may mean low tolerance to carbon dioxide.
- Breathing Hi-Low Test (seated or supine) – Hands on chest and stomach, breathe normal – what moves first? What moves most? Looking for lateral expansion and upward hand pivot.
- Breathing Wave – Lay prone, breathe normal, spine should flex in a wave-like pattern towards head. Segments that rise as a group may represent thoracic restrictions.
- Seated Lateral Expansion – Place hands on lower thorax and monitor motion while breathing. Looking for symmetrical lateral expansion.
Assessment of musculoskeletal system[edit | edit source]
- elevated and depressed ribs and clavicle.
- muscle tone and length especially psoas, QL, latissimus, upper trap, scalene, and SCM.
- alterations in mobility of thoracic and rib articulations.
Assessment of respiratory function[edit | edit source]
- Oximetry - to measure oxygen saturation (SpO2)
- Capnography - to measure end tidal CO2 levels in exhaled air
- Peak expiratory flow rate - the highest flow of air out of the lungs from peak inspiration in a fast single forced breath out
Outcome Measures[edit | edit source]
- Nijmegen Questionnaire
- Rowley Breathing Self-Efficacy Scale (RoBE)
- Self Evaluation of Breathing Questionnaire )SEBQ)
- Hospital Anxiety and Depression Questionnaire (HAD)
Management / Interventions
[edit | edit source]
Management commonly requires the removal of causative factors and the rehabilitation of habitual acquired dysfunctional breathing patterns. In order to achieve this most efficiently it may be necessary to restore normal function of the respiratory system such as thoracic mobility and muscle tone and length.
Manual Therapy Techniques[edit | edit source]
Based on your assessment, there are several manual therapy techniques that can be performed to treat muscles that have increased tone or activity, elevated and depressed ribs and alterations in mobility of thoracic articulations. These techniques include muscle energy techniques (MET), positional release, trigger point release and integrated neuromuscular inhibition techniques[3].
Breathing Retraining[edit | edit source]
- Awareness of faulty breathing patterns
- Relaxation of the jaw, upper chest, shoulderss and accesssory muscles
- Abdominal/low-chest nose breathing pattern reeducation
- Awareness of normal brething rates and rhythms, both at rest, during speech and activity.
Respiratory Techniques[edit | edit source]
- Pursed lip breathing has been shown to relieve dysponia, slow respiratory rate, increase tidal volume, and restore diaphragmatic function.
- Dynamic Neuromuscular Stabilisation - to optimise a postural respiratory pattern[3]
Complimentary methods[edit | edit source]
- Sleep retraining
- Relaxation
- Nutrition
- Capnography
Differential Diagnosis
[edit | edit source]
BPDs can often mimic more serious conditions such as cardiac conditions, gastrointestinal co
Key Evidence[edit | edit source]
add text here relating to key evidence with regards to any of the above headings
Resources
[edit | edit source]
add appropriate resources here
Case Studies[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1-ohVP9Y35PejK1jrUNpTuyNlOE7GEihimykUGaQZ8jTQ14ETo|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
- ↑ Peters, D. Foreword In: Recognizing and Treating Breathing Disorders. Chaitow, L., Bradley, D. and Gilbert, C. Elsevier, 2014
- ↑ Thomas, M., McKinley, R.K., Freeman, E., et al. The prevalence of dysfunctional breathing in adults in the community with and without asthma. Prim Care Respir J, 2005, 14, 78-82
- ↑ 3.0 3.1 3.2 Chaitow, L., Bradley, D. and Gilbert, C. Recognizing and Treating Breathing Disorders. Elsevier, 2014