Basic Foot and Ankle Anatomy - Bones and Ligaments: Difference between revisions
(added caption to image of bones of the foot) |
No edit summary |
||
| (24 intermediate revisions by 5 users not shown) | |||
| Line 6: | Line 6: | ||
</div> | </div> | ||
== Description == | == Description == | ||
Ankle and foot injuries are common musculoskeletal injuries with a high prevalence among professional athletes but also in recreational sports and as a result of routine daily activities.<ref>Vuurberg G, Hoorntje A, Wink LM, Van Der Doelen BF, Van Den Bekerom MP, Dekker R, Van Dijk CN, Krips R, Loogman MC, Ridderikhof ML, Smithuis FF. Diagnosis, treatment and prevention of ankle sprains: update of an evidence-based clinical guideline. British journal of sports medicine. 2018 Aug 1;52(15):956-.</ref> Typical injuries include [[Ankle Sprain|sprains]], [[Fracture|fractures]], tears, and [[Inflammation Acute and Chronic|inflammation.]] A good understanding of | Ankle and foot injuries are common musculoskeletal injuries with a high prevalence among professional athletes, but they also occur in recreational sports and as a result of routine daily activities.<ref>Vuurberg G, Hoorntje A, Wink LM, Van Der Doelen BF, Van Den Bekerom MP, Dekker R, Van Dijk CN, Krips R, Loogman MC, Ridderikhof ML, Smithuis FF. Diagnosis, treatment and prevention of ankle sprains: update of an evidence-based clinical guideline. British journal of sports medicine. 2018 Aug 1;52(15):956-.</ref> Typical injuries include [[Ankle Sprain|sprains]], [[Fracture|fractures]], tears, and [[Inflammation Acute and Chronic|inflammation.]] A good understanding of foot and ankle anatomy is necessary for the proper diagnosis and treatment of injuries. | ||
== Structure == | == Structure == | ||
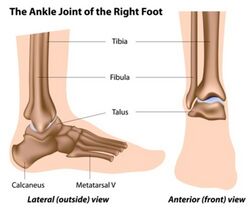
The ankle is formed by three bones: the talus, tibia and fibula. The anatomical structure of the foot consists of the hindfoot, midfoot and forefoot | The ankle is formed by three bones: the talus, tibia and fibula. The anatomical structure of the foot consists of the hindfoot, midfoot and forefoot. Each part of the foot is composed of several bones. | ||
=== Ankle Bones === | === Ankle Bones === | ||
The lower leg and | The lower leg and foot constitute the ankle. The following bony elements of the ankle joint are part of this structure: [[File: Shutterstock Image - Talocrural Joint - ID 89870980.jpeg|thumb|Ankle bones|alt=|250x250px]] | ||
* Distal [[tibia]] | * Distal [[tibia]] | ||
| Line 19: | Line 19: | ||
=== Foot Bones === | === Foot Bones === | ||
[[File:Bigstock_Image_-Anatomy_Bones_Of_The_Foot_-ID_404217734.jpg|alt=|right|frameless|450x450px|Bones of the Foot]] | [[File:Bigstock_Image_-Anatomy_Bones_Of_The_Foot_-ID_404217734.jpg|alt=|right|frameless|450x450px|Bones of the Foot]] | ||
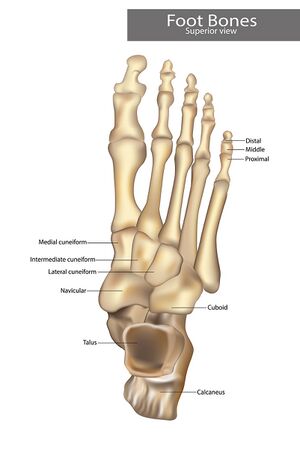
The talus and [[calcaneus]] | |||
The talus and [[calcaneus]] form the posterior aspect of the foot, which is called the ''hindfoot''. The ''midfoot'' (located between the hindfoot and forefoot) is made up of five tarsal bones: the [[navicular]], [[cuboid]], and medial, intermediate, and lateral [[cuneiforms]]. The most anterior aspect of the foot including the [[metatarsals]], phalanges, and sesamoid bones is called the ''forefoot''. Each digit, except for the great toe, consists of a metatarsal and three phalanges. The great toe has only two phalanges. | |||
== Function == | == Function == | ||
The foot and ankle provide various important functions which include bodyweight support, balance maintenance, shock absorption, response to ground reaction forces, or substitution for hand function in individuals with upper extremity [[Amputations|amputation.]]<ref>Houglum PA, Bertotti DB. Brunnstrom's clinical kinesiology. FA Davis; 2012</ref> | The foot and ankle provide various important functions which include bodyweight support, balance maintenance, shock absorption, response to ground reaction forces, or substitution for hand function in individuals with upper extremity [[Amputations|amputation.]]<ref>Houglum PA, Bertotti DB. Brunnstrom's clinical kinesiology. FA Davis; 2012</ref> The foot and ankle have a crucial role in [[gait]] and [[posture]] and malalignment can cause other problems such as back pain or mobility limitations.<ref>Menz HB, Dufour AB, Riskowski JL, Hillstrom HJ, Hannan MT. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3828513/ Foot posture, foot function and low back pain: the Framingham Foot Study.] Rheumatology (Oxford). 2013 Dec;52(12):2275-82. </ref><ref>Menz HB, Dufour AB, Katz P, Hannan MT. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4833542/ Foot Pain and Pronated Foot Type Are Associated with Self-Reported Mobility Limitations in Older Adults: The Framingham Foot Study]. Gerontology. 2016;62(3):289-95. </ref> | ||
=== Ankle and | === Ankle and Foot Articulations === | ||
[[File:Foot-Ankle-Toe-Treatment.png|thumb|Basic Ankle and Foot Motion]] | [[File:Foot-Ankle-Toe-Treatment.png|thumb|Basic Ankle and Foot Motion]] | ||
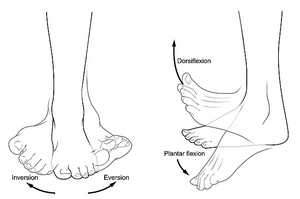
[[Foot and Ankle Structure and Function| | The [[Foot and Ankle Structure and Function|talocrural joint]] (TC or sometimes called a tibiotalar joint) is referred to as the ''ankle joint''. The joint is framed laterally and medially by the lateral and the medial malleolus and from the top by the tibia and the talus.<ref name=":0" /> Sagittal plane dorsiflexion and plantarflexion are the primary movements in this joint. | ||
The ''hindfoot'' has a [[talus]] and calcaneus articulation called | The ''hindfoot'' has a [[talus]] and calcaneus articulation called the [[Foot and Ankle Structure and Function|subtalar joint]] (ST, also known as the talocalcaneal joint). Three facets of the talus and of the calcaneus are part of this joint. The main motions are inversion and eversion of the ankle and hindfoot. | ||
The talonavicular and calcaneocuboid joints are known as | The talonavicular and calcaneocuboid joints are known as Chopart's joint (MT, [[Foot and Ankle Structure and Function|midtarsal]] or [[Foot and Ankle Structure and Function|transverse tarsal joint]]), which is located between the ''hindfoot and midfoot''. This joint allows forefoot rotation. The navicular articulates with all three cuneiform bones distally.<ref name=":0" /> In addition to the navicular and cuneiforms bones, the cuboid bone has a distal articulation with the base of the fourth and fifth metatarsal bones. | ||
The [[Foot and Ankle Structure and Function|tarsometatarsal joint]] (TMT or Lisfranc joint) | The [[Foot and Ankle Structure and Function|tarsometatarsal joint]] (TMT or Lisfranc's joint) connects the ''midfoot with the forefoot'' and originates from the lateral, intermediate and medial cuneiforms articulating with the bases of the three metatarsal bone (1st, 2nd, and 3rd). The small movement that occurs in the joint is described as dorsal and plantarflexion.<ref>Bähler A. [http://www.oandplibrary.org/cpo/pdf/1986_01_008.pdf The Biomechanics of the Foot.] CPO 1986;10(1):8-14.</ref> The bases of the remaining metatarsal bones (4th and 5th) connect with the cuboid bone.<ref name=":0">Ficke J, Byerly DW. [https://www.ncbi.nlm.nih.gov/books/NBK546698/ Anatomy, Bony Pelvis and Lower Limb, Foot.] [Updated 2021 Aug 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: <nowiki>https://www.ncbi.nlm.nih.gov/books/NBK546698/</nowiki></ref> | ||
The five rays, metatarsal and corresponding phalanges create ''forefoot'' medial and lateral columns where rays 1,2, and 3 belong to the middle column, rays 4 and 5 to the lateral column. | The five rays, metatarsal and corresponding phalanges create the ''forefoot'' medial and lateral columns where rays 1,2, and 3 belong to the middle column, rays 4 and 5 to the lateral column. The metatarsophalangeal joints (MTP joints) are the main components of the forefoot.<ref name=":0" /> Each toe, except for the great toe, has proximal and distal interphalangeal joints (IP joints). The latter has only one IP joint. | ||
Below is | Below is a summary of the ankle and foot articulations | ||
{| border="1" cellpadding="1" cellspacing="1" | {| border="1" cellpadding="1" cellspacing="1" | ||
|- | |- | ||
| Line 47: | Line 48: | ||
| Hinge | | Hinge | ||
| Sagittal | | Sagittal | ||
| Dorsiflexion | | Dorsiflexion and Plantarflexion | ||
|- | |- | ||
| ST joint | | ST joint | ||
| Line 57: | Line 58: | ||
| | | | ||
Inversion | Inversion and Eversion | ||
Dorsiflexion | Dorsiflexion and Plantarflexion | ||
|- | |- | ||
| Line 74: | Line 75: | ||
| | | | ||
Inversion | Inversion and Eversion | ||
Flexion | Flexion and Extension | ||
Forefoot rotation | Forefoot rotation | ||
| Line 94: | Line 95: | ||
| | | | ||
Flexion | Flexion and Extension | ||
Abduction | Abduction and Adduction | ||
|- | |- | ||
| Line 102: | Line 103: | ||
| Hinge | | Hinge | ||
| Sagittal | | Sagittal | ||
| Flexion | | Flexion and Extension | ||
|} | |} | ||
=== Ligaments === | === Ligaments === | ||
Acute and chronic ankle | Acute and chronic ankle pain are often associated with either [[Ligament Sprain|ligament injury]] or ligament laxity.<ref name=":1">Golanó P, Vega J, de Leeuw PA, Malagelada F, Manzanares MC, Götzens V, van Dijk CN. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2855022/pdf/167_2010_Article_1100.pdf Anatomy of the ankle ligaments: a pictorial essay]. Knee Surg Sports Traumatol Arthrosc. 2010 May;18(5):557-69. </ref> The ligaments of the ankle consist of the medial ligaments (the deltoid ligament), the lateral ligaments, and the ligaments connecting the distal epiphyses of the tibia and fibula called the tibiofibular syndesmosis.<ref name=":1" /> | ||
There are 4 main ligaments of the foot | There are 4 main ligaments of the foot: the plantar fascia, the plantar calcaneonavicular ligament (known as a spring ligament), the calcaneocuboid ligament, and the Lisfranc ligaments. | ||
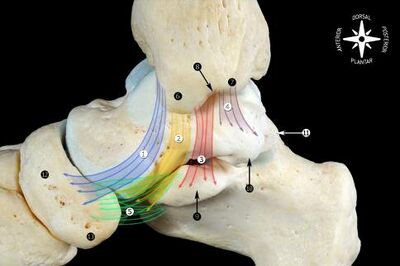
[[File:Medial collateral ligament.fcgi.jpeg| | ==== Medial Collateral Ligament (Deltoid Ligament) ==== | ||
[[File: Medial collateral ligament.fcgi.jpeg|Main components of the medial collateral ligament: 1. Tibionavicular ligament; 2. tibiospring ligament; 3. tibiocalcaneal ligament; 4. deep posterior tibiotalar ligament; 5. spring ligament complex (plantar and superomedial calcaneonavicular ligaments)<ref name=":3">Golanó P, Vega J, De Leeuw PA, Malagelada F, Manzanares MC, Götzens V, Van Dijk CN. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2855022/ Anatomy of the ankle ligaments: a pictorial essay.] Knee Surgery, Sports Traumatology, Arthroscopy. 2010 May;18(5):557-69.</ref> |alt=|border|thumb|400x400px]]There are various descriptions of the medial collateral ligament (MCL), but the definition provided by Milner and Soames<ref name=":4">Milner CE, Soames RW. Anatomy of the collateral ligaments of the human ankle joint. Foot Ankle Int. 1998 Nov;19(11):757-60. </ref> is the most commonly accepted. The authors divide the MCL into two layers: superficial and deep. The ligaments consist of bands that are either always present or sometimes present (bands that are always present are shown in ''italics''):<ref name=":4" /> | |||
There are various descriptions of the medial collateral ligament(MCL), but the definition provided by Milner and Soames | |||
* Superficial: ''tibiospring ligament, tibionavicular ligament'', superficial posterior tibiotalar ligament, tibiocalcaneal ligament. | * Superficial: ''tibiospring ligament, tibionavicular ligament'', superficial posterior tibiotalar ligament, tibiocalcaneal ligament. | ||
* Deep: ''deep posterior tibiotalar ligament'', deep anterior tibiotalar ligament. | * Deep: ''deep posterior tibiotalar ligament'', deep anterior tibiotalar ligament. | ||
<blockquote>It is important to mention that the dissection revealed the continuous nature of these ligaments and individual bands were impossible to distinguish.<ref name=":1" /></blockquote>The | <blockquote>It is important to mention that the dissection revealed the continuous nature of these ligaments and individual bands were impossible to distinguish.<ref name=":1" /></blockquote>The MCL has the following characteristics: | ||
* multifascicular | * multifascicular | ||
| Line 124: | Line 122: | ||
* tendon sheath of the posterior tibial muscle covers the posterior and middle part of the deltoid ligament | * tendon sheath of the posterior tibial muscle covers the posterior and middle part of the deltoid ligament | ||
* tendons cover most of the MCL as it inserts at the foot.<ref name=":1" /> | * tendons cover most of the MCL as it inserts at the foot.<ref name=":1" /> | ||
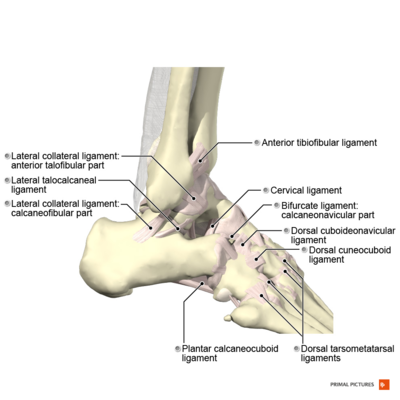
==== Lateral Collateral Ligament ==== | ==== Lateral Collateral Ligament ==== | ||
The lateral collateral ligament complex (LCL) is composed of three ligaments: anterior talofibular, calcaneofibular, and posterior talofibular ligaments. | The lateral collateral ligament complex (LCL) is composed of three ligaments: the anterior talofibular, calcaneofibular, and posterior talofibular ligaments. | ||
* ''Anterior talofibular ligament (ATFL):'' | * ''Anterior talofibular ligament (ATFL):'' | ||
** is made up of two bands | ** is made up of two bands[[File:Ligaments of the ankle lateral aspect Primal.png|alt=|thumb|400x400px|Lateral ankle ligament]] | ||
** originates at the anterior margin of the lateral malleolus and inserts on the talus | ** originates at the anterior margin of the lateral malleolus and inserts on the talus | ||
** lays horizontally to the ankle | ** lays horizontally to the ankle | ||
| Line 143: | Line 139: | ||
** allows talocrural joint flexion and extension and subtalar movement. | ** allows talocrural joint flexion and extension and subtalar movement. | ||
* ''Posterior | * ''Posterior talofibular ligament (PTFL):'' | ||
** originates from the malleolar fossa and inserts in the posterolateral talus | ** originates from the malleolar fossa and inserts in the posterolateral talus | ||
** some fibres become involved in forming the tunnel for the flexor hallucis longus tendon | ** some fibres become involved in forming the tunnel for the [[flexor hallucis longus]] tendon | ||
** runs almost horizontally | ** runs almost horizontally | ||
** | ** the ligament is relaxed in a neutral ankle position and during plantarflexion, and it is taut in dorsiflexion. | ||
<blockquote>Interconnections between the ATFL, CFL, and PTFL via medial connecting fibres lead to the formation of an anatomical and functional lateral fibulotalocalcaneal ligament complex.<ref name=":2" /> <ref>Dalmau-Pastor M, Malagelada F, Calder J, Manzanares MC, Vega J. The lateral ankle ligaments are interconnected: the medial connecting fibres between the anterior talofibular, calcaneofibular and posterior talofibular ligaments. Knee Surg Sports Traumatol Arthrosc. 2020 Jan;28(1):34-39. </ref> </blockquote> | <blockquote>Interconnections between the ATFL, CFL, and PTFL via medial connecting fibres lead to the formation of an anatomical and functional lateral fibulotalocalcaneal ligament complex.<ref name=":2" /> <ref>Dalmau-Pastor M, Malagelada F, Calder J, Manzanares MC, Vega J. The lateral ankle ligaments are interconnected: the medial connecting fibres between the anterior talofibular, calcaneofibular and posterior talofibular ligaments. Knee Surg Sports Traumatol Arthrosc. 2020 Jan;28(1):34-39. </ref> </blockquote> | ||
==== Tibiofibular Syndesmosis ==== | ==== Tibiofibular Syndesmosis ==== | ||
[[Distal Tibiofibular Syndesmosis| | The [[Distal Tibiofibular Syndesmosis|tibiofibular syndesmosis]] articulation allows medial rotation of the fibula during maximum ankle dorsiflexion and inversion of the fibula during ankle plantarflexion. In addition, it provides stability between the tibia and the fibula at their distal ends.<ref>Yammine K, Jalloul M, Assi C.Distal tibiofibular syndesmosis: A meta-analysis of cadaveric studies. Morphologie, 2021.</ref> It includes: | ||
* ''Anteroinferior tibiofibular ligament'' | * ''Anteroinferior tibiofibular ligament'' | ||
| Line 160: | Line 156: | ||
** has two independent parts: superficial and deep | ** has two independent parts: superficial and deep | ||
** superficial component (a true posteroinferior tibiofibular ligament) originates at the posterior edge of the lateral malleolus and is inserted in the posterior tibial tubercle | ** superficial component (a true posteroinferior tibiofibular ligament) originates at the posterior edge of the lateral malleolus and is inserted in the posterior tibial tubercle | ||
** deep component (transverse ligament) originates in the proximal malleolar fossa and inserts in the posterior edge of the tibia | ** deep component (transverse ligament) originates in the proximal malleolar fossa and inserts in the posterior edge of the tibia | ||
** provides talocrural joint stability and prevents posterior talar translation. | ** provides talocrural joint stability and prevents posterior talar translation. | ||
* ''Interosseous tibiofibular ligament'' | * ''Interosseous tibiofibular ligament'' | ||
** short fibres running between tibia and fibula | ** short fibres running between the tibia and fibula | ||
** distal continuation of the interosseous membrane | ** distal continuation of the interosseous membrane | ||
** responsible for maintaining ankle stability.<ref name=":1" /><ref>Hoefnagels EM, Waites MD, Wing ID, Belkoff SM, Swierstra BA. Biomechanical comparison of the interosseous tibiofibular ligament and the anterior tibiofibular ligament. Foot Ankle Int. 2007 May;28(5):602-4.</ref> | ** responsible for maintaining ankle stability.<ref name=":1" /><ref>Hoefnagels EM, Waites MD, Wing ID, Belkoff SM, Swierstra BA. Biomechanical comparison of the interosseous tibiofibular ligament and the anterior tibiofibular ligament. Foot Ankle Int. 2007 May;28(5):602-4.</ref> | ||
<blockquote>A fatty synovial fringe located distal to the ligament insertion is also part of this structure. Its upward and downward movement occurs during ankle movement and alters its placement between the tibia and the fibula. This adipose tissue is considered a cause of a syndesmotic impingement following an ankle sprain.</blockquote> | <blockquote>A fatty synovial fringe located distal to the ligament insertion is also part of this structure. Its upward and downward movement occurs during ankle movement and alters its placement between the tibia and the fibula. This adipose tissue is considered a cause of a syndesmotic impingement following an ankle sprain.</blockquote> | ||
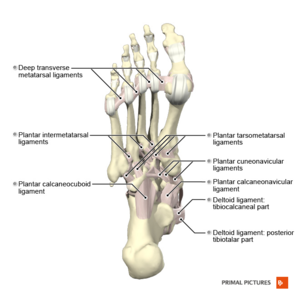
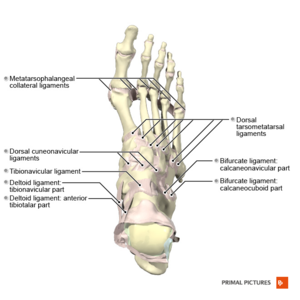
==== Ligaments of the Foot ==== | ==== Ligaments of the Foot ==== | ||
The main function of the short and long plantar ligaments and the calcaneonavicular ligament (spring ligament) is to assist in the passive maintenance of the arch. | The main function of the short and long plantar ligaments and the calcaneonavicular ligament (spring ligament) is to assist in the passive maintenance of the arch. | ||
* ''[[Plantar Fasciitis|Plantar fascia]] | *[[File: Ligaments of the foot plantar aspect Primal.png|thumb|Ligaments of the foot-plantar surface|alt=]]''[[Plantar Fasciitis|Plantar fascia]]'' | ||
** originates in the medial calcaneal tubercle and ends at the five metatarsal bones | ** originates in the medial calcaneal tubercle and ends at the five metatarsal bones | ||
** | ** considered the primary passive plantar tissue that supports the medial longitudinal arch | ||
** extremely strong ligament | ** extremely strong ligament | ||
** absorbs the impact of ground reaction force in running or jumping | ** absorbs the impact of the ground reaction force in running or jumping | ||
** | ** maintains and stores energy in the foot | ||
** disperses stress throughout the metatarsus | |||
** dysfunction of plantar fascia affects the height and shape of the medial longitudinal arch<ref>Peng Y, Wai-Chi Wong D, Wang Y, Lin-Wei Chen T, Zhang G, Yan F, Zhang M.[https://reader.elsevier.com/reader/sd/pii/S2590093520300242?token=2134B955ADDD421151E9A8C822104D3090BA52EBE3157B0051DC515AE64D84168DFD670C4D6BD6630D6F3FD9A3B4936F&originRegion=eu-west-1&originCreation=20211219210130 Computational models of flatfoot with three-dimensional fascia and bulk soft tissue interaction for orthosis design]. Medicine in Novel Technology and Devices,2021;9. | ** dysfunction of plantar fascia affects the height and shape of the medial longitudinal arch<ref>Peng Y, Wai-Chi Wong D, Wang Y, Lin-Wei Chen T, Zhang G, Yan F, Zhang M.[https://reader.elsevier.com/reader/sd/pii/S2590093520300242?token=2134B955ADDD421151E9A8C822104D3090BA52EBE3157B0051DC515AE64D84168DFD670C4D6BD6630D6F3FD9A3B4936F&originRegion=eu-west-1&originCreation=20211219210130 Computational models of flatfoot with three-dimensional fascia and bulk soft tissue interaction for orthosis design]. Medicine in Novel Technology and Devices,2021;9. | ||
</ref> | </ref> | ||
** any morphological or mechanical changes in the plantar fascia will produce lesions.<ref>Wang K, Liu J, Wu J, Qian Z, Ren L and Ren L. [https://ieeexplore.ieee.org/abstract/document/8681551 Noninvasive in Vivo Study of the Morphology and Mechanical Properties of Plantar Fascia Based on Ultrasound]. IEEE Access 2019; 7: 53641-53649. </ref> | ** any morphological or mechanical changes in the plantar fascia will produce lesions.<ref>Wang K, Liu J, Wu J, Qian Z, Ren L and Ren L. [https://ieeexplore.ieee.org/abstract/document/8681551 Noninvasive in Vivo Study of the Morphology and Mechanical Properties of Plantar Fascia Based on Ultrasound]. IEEE Access 2019; 7: 53641-53649. </ref> | ||
* ''Plantar calcaneonavicular ligament (SL, spring ligament)'' | * ''Plantar calcaneonavicular ligament (SL, spring ligament)'' [[File: Ligaments of the foot dorsal aspect Primal.png|thumb|Ligaments of the foot-dorsal surface]] | ||
** a passive | ** a passive stabiliser of the plantar arch in the talocalcaneal joint | ||
** supports compression forces | ** supports compression forces | ||
** the strongest medial ligament | ** the strongest medial ligament | ||
** | ** assists with preventing talus medial rotation and plantar flexion | ||
** limits navicular | ** limits navicular dorsiflexion, eversion, and abduction | ||
** pes planus may be produced by isolated SL injuries.<ref>Casado-Hernández I, Becerro-de-Bengoa-Vallejo R, Losa-Iglesias ME, Santiago-Nuño F, Mazoteras-Pardo V, López-López D, Rodríguez-Sanz D, Calvo-Lobo C. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7719946/pdf/qims-11-01-84.pdf Association between anterior talofibular ligament injury and ankle tendon, ligament, and joint conditions revealed by magnetic resonance imaging]. Quant Imaging Med Surg. 2021 Jan;11(1):84-94. </ref> | ** pes planus may be produced by isolated SL injuries.<ref>Casado-Hernández I, Becerro-de-Bengoa-Vallejo R, Losa-Iglesias ME, Santiago-Nuño F, Mazoteras-Pardo V, López-López D, Rodríguez-Sanz D, Calvo-Lobo C. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7719946/pdf/qims-11-01-84.pdf Association between anterior talofibular ligament injury and ankle tendon, ligament, and joint conditions revealed by magnetic resonance imaging]. Quant Imaging Med Surg. 2021 Jan;11(1):84-94. </ref> | ||
* ''Calcaneocuboid ligament'' | * ''Calcaneocuboid ligament'' | ||
** consists of the medial calcaneocuboid ligament(a component of the bifurcate ligament), the dorsolateral calcaneocuboid ligament, the plantar calcaneocuboid ligament (SPL or short plantar ligament), and the long plantar ligament (LPL) | ** consists of the medial calcaneocuboid ligament (a component of the bifurcate ligament), the dorsolateral calcaneocuboid ligament, the plantar calcaneocuboid ligament (SPL or short plantar ligament), and the long plantar ligament (LPL) | ||
** LPL originates on the inferior surface of the calcaneus and inserts into the bases of the second to fourth metatarsals (MTs) and not the distal cuboid. | ** LPL originates on the inferior surface of the calcaneus and inserts into the bases of the second to fourth metatarsals (MTs) and not the distal cuboid. | ||
** SPL originates at the anterior tubercle of the calcaneus and attaches to the plantar surface of the cuboid | ** SPL originates at the anterior tubercle of the calcaneus and attaches to the plantar surface of the cuboid | ||
| Line 203: | Line 197: | ||
** maintains the stability of the medial column and axial column of the foot arch.<ref>Ablimit A, Ding HY, Liu LG. [https://link.springer.com/content/pdf/10.1186/s13018-018-0968-x.pdf Magnetic resonance imaging of the Lisfranc ligament]. J Orthop Surg Res 2018; 13 (282). </ref> | ** maintains the stability of the medial column and axial column of the foot arch.<ref>Ablimit A, Ding HY, Liu LG. [https://link.springer.com/content/pdf/10.1186/s13018-018-0968-x.pdf Magnetic resonance imaging of the Lisfranc ligament]. J Orthop Surg Res 2018; 13 (282). </ref> | ||
You can now watch this short video on how to palpate important | You can now watch this short video on how to palpate important anatomical structures of the foot and the ankle. | ||
{{#ev:youtube|aJRemQbNPhk|350}}<ref>Ankle and foot palpation. 2012 Available from: https://www.youtube.com/watch?v=aJRemQbNPhk [last accessed 18/12/2021]</ref> | {{#ev:youtube|aJRemQbNPhk|350}}<ref>Ankle and foot palpation. 2012 Available from: https://www.youtube.com/watch?v=aJRemQbNPhk [last accessed 18/12/2021]</ref> | ||
| Line 209: | Line 203: | ||
== Clinical Relevance == | == Clinical Relevance == | ||
# Ankle fractures affect | # Ankle fractures mainly affect two groups: young active males and older females. In the first group, fractures occur as a consequence of sporting activities, whereas in the latter group it is an osteoporotic injury.<ref>McKeown R, Ellard DR, Rabiu AR. et al. [https://jpro.springeropen.com/track/pdf/10.1186/s41687-019-0159-5.pdf A systematic review of the measurement properties of patient-reported outcome measures used for adults with an ankle fracture]. J Patient Rep Outcomes 2019; 3 (70) </ref> | ||
# Injuries to the ankle are painful and cause significant mobility limitations. | # Injuries to the ankle are painful and cause significant mobility limitations. | ||
# Patient-reported outcome measures (PROM) are used in clinical trials to measure the effect of treatment after lower limb fracture. | # Patient-reported outcome measures (PROM) are used in clinical trials to measure the effect of treatment after lower limb fracture. | ||
# | # One third of all ankle fractures can result in tibiotalar joint dislocations.<ref>Lawson KA, Ayala AE, Morin ML, Latt LD, Wild JR. [https://journals.sagepub.com/doi/pdf/10.1177/2473011418765122 Ankle Fracture-Dislocations: A Review]. Foot & Ankle Orthopaedics. July 2018. </ref> | ||
# Chronic ankle | # Chronic ankle ligament injury is difficult to diagnose, but using ultrasound showed high diagnostic accuracy.<ref>Cao S, Wang C, Ma X. et al. [https://link.springer.com/content/pdf/10.1186/s13018-018-0811-4.pdf Imaging diagnosis for chronic lateral ankle ligament injury: a systemic review with meta-analysis]. J Orthop Surg Res 2018; 13 (122).</ref> | ||
# Chronic ankle instability may be a result of poorly managed acute ankle | # Chronic ankle instability may be a result of poorly managed acute ankle ligament injury. | ||
# After 1 to 5 years post-acute ligament sprain, the individual can still suffer from pain, functional instability, mechanical instability or recurrent sprain. <ref>Thompson JY, Byrne C, Williams MA. et al. [https://link.springer.com/content/pdf/10.1186/s12891-017-1777-9.pdf Prognostic factors for recovery following acute lateral ankle ligament sprain: a systematic review]. BMC Musculoskelet Disord 2017; 18 (421). </ref> | # After 1 to 5 years post-acute ligament sprain, the individual can still suffer from pain, functional instability, mechanical instability or recurrent sprain.<ref>Thompson JY, Byrne C, Williams MA. et al. [https://link.springer.com/content/pdf/10.1186/s12891-017-1777-9.pdf Prognostic factors for recovery following acute lateral ankle ligament sprain: a systematic review]. BMC Musculoskelet Disord 2017; 18 (421). </ref> | ||
== Resources == | == Resources == | ||
[https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2855022/pdf/167_2010_Article_1100.pdf Anatomy of the Ankle Ligaments: A Pictorial Essay] - In this pictorial essay, the ligaments around the ankle are grouped, depending on their anatomic orientation, and each of the ankle ligaments is discussed in detail. | [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2855022/pdf/167_2010_Article_1100.pdf Anatomy of the Ankle Ligaments: A Pictorial Essay]<ref name=":3" /> - In this pictorial essay, the ligaments around the ankle are grouped, depending on their anatomic orientation, and each of the ankle ligaments is discussed in detail. | ||
= References | == References == | ||
<references /> | <references /> | ||
| Line 229: | Line 223: | ||
[[Category:Foot - Anatomy]] | [[Category:Foot - Anatomy]] | ||
[[Category:Ankle - Anatomy]] | [[Category:Ankle - Anatomy]] | ||
[[Category: | [[Category:Plus Content]] | ||
Latest revision as of 09:19, 23 November 2022
Original Editor - Ewa Jaraczewska
Top Contributors - Ewa Jaraczewska, Wanda van Niekerk, Jess Bell, Tarina van der Stockt, Niha Mulla, Kim Jackson and Olajumoke Ogunleye
Description[edit | edit source]
Ankle and foot injuries are common musculoskeletal injuries with a high prevalence among professional athletes, but they also occur in recreational sports and as a result of routine daily activities.[1] Typical injuries include sprains, fractures, tears, and inflammation. A good understanding of foot and ankle anatomy is necessary for the proper diagnosis and treatment of injuries.
Structure[edit | edit source]
The ankle is formed by three bones: the talus, tibia and fibula. The anatomical structure of the foot consists of the hindfoot, midfoot and forefoot. Each part of the foot is composed of several bones.
Ankle Bones[edit | edit source]
The lower leg and foot constitute the ankle. The following bony elements of the ankle joint are part of this structure:
Foot Bones[edit | edit source]
The talus and calcaneus form the posterior aspect of the foot, which is called the hindfoot. The midfoot (located between the hindfoot and forefoot) is made up of five tarsal bones: the navicular, cuboid, and medial, intermediate, and lateral cuneiforms. The most anterior aspect of the foot including the metatarsals, phalanges, and sesamoid bones is called the forefoot. Each digit, except for the great toe, consists of a metatarsal and three phalanges. The great toe has only two phalanges.
Function[edit | edit source]
The foot and ankle provide various important functions which include bodyweight support, balance maintenance, shock absorption, response to ground reaction forces, or substitution for hand function in individuals with upper extremity amputation.[2] The foot and ankle have a crucial role in gait and posture and malalignment can cause other problems such as back pain or mobility limitations.[3][4]
Ankle and Foot Articulations[edit | edit source]
The talocrural joint (TC or sometimes called a tibiotalar joint) is referred to as the ankle joint. The joint is framed laterally and medially by the lateral and the medial malleolus and from the top by the tibia and the talus.[5] Sagittal plane dorsiflexion and plantarflexion are the primary movements in this joint.
The hindfoot has a talus and calcaneus articulation called the subtalar joint (ST, also known as the talocalcaneal joint). Three facets of the talus and of the calcaneus are part of this joint. The main motions are inversion and eversion of the ankle and hindfoot.
The talonavicular and calcaneocuboid joints are known as Chopart's joint (MT, midtarsal or transverse tarsal joint), which is located between the hindfoot and midfoot. This joint allows forefoot rotation. The navicular articulates with all three cuneiform bones distally.[5] In addition to the navicular and cuneiforms bones, the cuboid bone has a distal articulation with the base of the fourth and fifth metatarsal bones.
The tarsometatarsal joint (TMT or Lisfranc's joint) connects the midfoot with the forefoot and originates from the lateral, intermediate and medial cuneiforms articulating with the bases of the three metatarsal bone (1st, 2nd, and 3rd). The small movement that occurs in the joint is described as dorsal and plantarflexion.[6] The bases of the remaining metatarsal bones (4th and 5th) connect with the cuboid bone.[5]
The five rays, metatarsal and corresponding phalanges create the forefoot medial and lateral columns where rays 1,2, and 3 belong to the middle column, rays 4 and 5 to the lateral column. The metatarsophalangeal joints (MTP joints) are the main components of the forefoot.[5] Each toe, except for the great toe, has proximal and distal interphalangeal joints (IP joints). The latter has only one IP joint.
Below is a summary of the ankle and foot articulations
| Joint | Type of Joint | Plane of Movement | Motion |
|---|---|---|---|
| TC joint | Hinge | Sagittal | Dorsiflexion and Plantarflexion |
| ST joint | Condyloid |
Mainly transverse Some sagittal |
Inversion and Eversion Dorsiflexion and Plantarflexion |
| MT joint |
TN joint - Ball and socket CC joint - Modified saddle |
Largely in transverse Some sagittal |
Inversion and Eversion Flexion and Extension Forefoot rotation |
| TMT joint | Planar | ||
| MTP joint | Condyloid |
Sagittal Some Transverse |
Flexion and Extension Abduction and Adduction |
| IP joint | Hinge | Sagittal | Flexion and Extension |
Ligaments[edit | edit source]
Acute and chronic ankle pain are often associated with either ligament injury or ligament laxity.[7] The ligaments of the ankle consist of the medial ligaments (the deltoid ligament), the lateral ligaments, and the ligaments connecting the distal epiphyses of the tibia and fibula called the tibiofibular syndesmosis.[7]
There are 4 main ligaments of the foot: the plantar fascia, the plantar calcaneonavicular ligament (known as a spring ligament), the calcaneocuboid ligament, and the Lisfranc ligaments.
Medial Collateral Ligament (Deltoid Ligament)[edit | edit source]
There are various descriptions of the medial collateral ligament (MCL), but the definition provided by Milner and Soames[9] is the most commonly accepted. The authors divide the MCL into two layers: superficial and deep. The ligaments consist of bands that are either always present or sometimes present (bands that are always present are shown in italics):[9]
- Superficial: tibiospring ligament, tibionavicular ligament, superficial posterior tibiotalar ligament, tibiocalcaneal ligament.
- Deep: deep posterior tibiotalar ligament, deep anterior tibiotalar ligament.
It is important to mention that the dissection revealed the continuous nature of these ligaments and individual bands were impossible to distinguish.[7]
The MCL has the following characteristics:
- multifascicular
- originates from the medial malleolus and inserts in the talus
- tendon sheath of the posterior tibial muscle covers the posterior and middle part of the deltoid ligament
- tendons cover most of the MCL as it inserts at the foot.[7]
Lateral Collateral Ligament[edit | edit source]
The lateral collateral ligament complex (LCL) is composed of three ligaments: the anterior talofibular, calcaneofibular, and posterior talofibular ligaments.
- Anterior talofibular ligament (ATFL):
- is made up of two bands
- originates at the anterior margin of the lateral malleolus and inserts on the talus
- lays horizontally to the ankle
- limits anterior displacement of the talus and ankle plantarflexion
- the weakest part of the LCL.[10]
- Calcaneofibular ligament (CFL):
- originates from the anterior part of the lateral malleolus and attaches to the posterior region of the lateral calcaneal surface
- located below the lower band of the anterior talofibular ligament
- runs obliquely downwards and backwards
- bridges the talocrural joint and subtalar joint
- allows talocrural joint flexion and extension and subtalar movement.
- Posterior talofibular ligament (PTFL):
- originates from the malleolar fossa and inserts in the posterolateral talus
- some fibres become involved in forming the tunnel for the flexor hallucis longus tendon
- runs almost horizontally
- the ligament is relaxed in a neutral ankle position and during plantarflexion, and it is taut in dorsiflexion.
Interconnections between the ATFL, CFL, and PTFL via medial connecting fibres lead to the formation of an anatomical and functional lateral fibulotalocalcaneal ligament complex.[10] [11]
Tibiofibular Syndesmosis[edit | edit source]
The tibiofibular syndesmosis articulation allows medial rotation of the fibula during maximum ankle dorsiflexion and inversion of the fibula during ankle plantarflexion. In addition, it provides stability between the tibia and the fibula at their distal ends.[12] It includes:
- Anteroinferior tibiofibular ligament
- originates in the anterior tubercle of the tibia and inserts in the anterior margin of the lateral malleolus
- made up of several fascicles
- when damaged can cause ankle instability.
- Posteroinferior tibiofibular ligament
- has two independent parts: superficial and deep
- superficial component (a true posteroinferior tibiofibular ligament) originates at the posterior edge of the lateral malleolus and is inserted in the posterior tibial tubercle
- deep component (transverse ligament) originates in the proximal malleolar fossa and inserts in the posterior edge of the tibia
- provides talocrural joint stability and prevents posterior talar translation.
- Interosseous tibiofibular ligament
A fatty synovial fringe located distal to the ligament insertion is also part of this structure. Its upward and downward movement occurs during ankle movement and alters its placement between the tibia and the fibula. This adipose tissue is considered a cause of a syndesmotic impingement following an ankle sprain.
Ligaments of the Foot[edit | edit source]
The main function of the short and long plantar ligaments and the calcaneonavicular ligament (spring ligament) is to assist in the passive maintenance of the arch.
- Plantar fascia
- originates in the medial calcaneal tubercle and ends at the five metatarsal bones
- considered the primary passive plantar tissue that supports the medial longitudinal arch
- extremely strong ligament
- absorbs the impact of the ground reaction force in running or jumping
- maintains and stores energy in the foot
- disperses stress throughout the metatarsus
- dysfunction of plantar fascia affects the height and shape of the medial longitudinal arch[14]
- any morphological or mechanical changes in the plantar fascia will produce lesions.[15]
- Plantar calcaneonavicular ligament (SL, spring ligament)
- a passive stabiliser of the plantar arch in the talocalcaneal joint
- supports compression forces
- the strongest medial ligament
- assists with preventing talus medial rotation and plantar flexion
- limits navicular dorsiflexion, eversion, and abduction
- pes planus may be produced by isolated SL injuries.[16]
- Calcaneocuboid ligament
- consists of the medial calcaneocuboid ligament (a component of the bifurcate ligament), the dorsolateral calcaneocuboid ligament, the plantar calcaneocuboid ligament (SPL or short plantar ligament), and the long plantar ligament (LPL)
- LPL originates on the inferior surface of the calcaneus and inserts into the bases of the second to fourth metatarsals (MTs) and not the distal cuboid.
- SPL originates at the anterior tubercle of the calcaneus and attaches to the plantar surface of the cuboid
- Supports the medial and lateral longitudinal arches
- Can be damaged during inversion injury of the foot.[17]
- Lisfranc ligament
- originates from the lateral side of the medial cuneiform bone and inserts at the medial side of the base of the second metatarsal bone
- maintains the stability of the medial column and axial column of the foot arch.[18]
You can now watch this short video on how to palpate important anatomical structures of the foot and the ankle.
Clinical Relevance[edit | edit source]
- Ankle fractures mainly affect two groups: young active males and older females. In the first group, fractures occur as a consequence of sporting activities, whereas in the latter group it is an osteoporotic injury.[20]
- Injuries to the ankle are painful and cause significant mobility limitations.
- Patient-reported outcome measures (PROM) are used in clinical trials to measure the effect of treatment after lower limb fracture.
- One third of all ankle fractures can result in tibiotalar joint dislocations.[21]
- Chronic ankle ligament injury is difficult to diagnose, but using ultrasound showed high diagnostic accuracy.[22]
- Chronic ankle instability may be a result of poorly managed acute ankle ligament injury.
- After 1 to 5 years post-acute ligament sprain, the individual can still suffer from pain, functional instability, mechanical instability or recurrent sprain.[23]
Resources[edit | edit source]
Anatomy of the Ankle Ligaments: A Pictorial Essay[8] - In this pictorial essay, the ligaments around the ankle are grouped, depending on their anatomic orientation, and each of the ankle ligaments is discussed in detail.
References[edit | edit source]
- ↑ Vuurberg G, Hoorntje A, Wink LM, Van Der Doelen BF, Van Den Bekerom MP, Dekker R, Van Dijk CN, Krips R, Loogman MC, Ridderikhof ML, Smithuis FF. Diagnosis, treatment and prevention of ankle sprains: update of an evidence-based clinical guideline. British journal of sports medicine. 2018 Aug 1;52(15):956-.
- ↑ Houglum PA, Bertotti DB. Brunnstrom's clinical kinesiology. FA Davis; 2012
- ↑ Menz HB, Dufour AB, Riskowski JL, Hillstrom HJ, Hannan MT. Foot posture, foot function and low back pain: the Framingham Foot Study. Rheumatology (Oxford). 2013 Dec;52(12):2275-82.
- ↑ Menz HB, Dufour AB, Katz P, Hannan MT. Foot Pain and Pronated Foot Type Are Associated with Self-Reported Mobility Limitations in Older Adults: The Framingham Foot Study. Gerontology. 2016;62(3):289-95.
- ↑ 5.0 5.1 5.2 5.3 Ficke J, Byerly DW. Anatomy, Bony Pelvis and Lower Limb, Foot. [Updated 2021 Aug 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK546698/
- ↑ Bähler A. The Biomechanics of the Foot. CPO 1986;10(1):8-14.
- ↑ 7.0 7.1 7.2 7.3 7.4 Golanó P, Vega J, de Leeuw PA, Malagelada F, Manzanares MC, Götzens V, van Dijk CN. Anatomy of the ankle ligaments: a pictorial essay. Knee Surg Sports Traumatol Arthrosc. 2010 May;18(5):557-69.
- ↑ 8.0 8.1 Golanó P, Vega J, De Leeuw PA, Malagelada F, Manzanares MC, Götzens V, Van Dijk CN. Anatomy of the ankle ligaments: a pictorial essay. Knee Surgery, Sports Traumatology, Arthroscopy. 2010 May;18(5):557-69.
- ↑ 9.0 9.1 Milner CE, Soames RW. Anatomy of the collateral ligaments of the human ankle joint. Foot Ankle Int. 1998 Nov;19(11):757-60.
- ↑ 10.0 10.1 Szaro P, Ghali Gataa K, Polaczek M. et al. The double fascicular variations of the anterior talofibular ligament and the calcaneofibular ligament correlate with interconnections between lateral ankle structures revealed on magnetic resonance imaging. Sci Rep 2020;10: 20801.
- ↑ Dalmau-Pastor M, Malagelada F, Calder J, Manzanares MC, Vega J. The lateral ankle ligaments are interconnected: the medial connecting fibres between the anterior talofibular, calcaneofibular and posterior talofibular ligaments. Knee Surg Sports Traumatol Arthrosc. 2020 Jan;28(1):34-39.
- ↑ Yammine K, Jalloul M, Assi C.Distal tibiofibular syndesmosis: A meta-analysis of cadaveric studies. Morphologie, 2021.
- ↑ Hoefnagels EM, Waites MD, Wing ID, Belkoff SM, Swierstra BA. Biomechanical comparison of the interosseous tibiofibular ligament and the anterior tibiofibular ligament. Foot Ankle Int. 2007 May;28(5):602-4.
- ↑ Peng Y, Wai-Chi Wong D, Wang Y, Lin-Wei Chen T, Zhang G, Yan F, Zhang M.Computational models of flatfoot with three-dimensional fascia and bulk soft tissue interaction for orthosis design. Medicine in Novel Technology and Devices,2021;9.
- ↑ Wang K, Liu J, Wu J, Qian Z, Ren L and Ren L. Noninvasive in Vivo Study of the Morphology and Mechanical Properties of Plantar Fascia Based on Ultrasound. IEEE Access 2019; 7: 53641-53649.
- ↑ Casado-Hernández I, Becerro-de-Bengoa-Vallejo R, Losa-Iglesias ME, Santiago-Nuño F, Mazoteras-Pardo V, López-López D, Rodríguez-Sanz D, Calvo-Lobo C. Association between anterior talofibular ligament injury and ankle tendon, ligament, and joint conditions revealed by magnetic resonance imaging. Quant Imaging Med Surg. 2021 Jan;11(1):84-94.
- ↑ Edama M, Takabayashi T, Yokota H. et al. Morphological characteristics of the plantar calcaneocuboid ligaments. J Foot Ankle Res 2021; 14 (3).
- ↑ Ablimit A, Ding HY, Liu LG. Magnetic resonance imaging of the Lisfranc ligament. J Orthop Surg Res 2018; 13 (282).
- ↑ Ankle and foot palpation. 2012 Available from: https://www.youtube.com/watch?v=aJRemQbNPhk [last accessed 18/12/2021]
- ↑ McKeown R, Ellard DR, Rabiu AR. et al. A systematic review of the measurement properties of patient-reported outcome measures used for adults with an ankle fracture. J Patient Rep Outcomes 2019; 3 (70)
- ↑ Lawson KA, Ayala AE, Morin ML, Latt LD, Wild JR. Ankle Fracture-Dislocations: A Review. Foot & Ankle Orthopaedics. July 2018.
- ↑ Cao S, Wang C, Ma X. et al. Imaging diagnosis for chronic lateral ankle ligament injury: a systemic review with meta-analysis. J Orthop Surg Res 2018; 13 (122).
- ↑ Thompson JY, Byrne C, Williams MA. et al. Prognostic factors for recovery following acute lateral ankle ligament sprain: a systematic review. BMC Musculoskelet Disord 2017; 18 (421).