Baker's Cyst
Original Editor - Agapi Hakobyan
Top Contributors - Claudia Karina, Admin, Sheik Abdul Khadir, Chenoa Morales Caceres, Laura Ritchie, Kaviesha Madurapperuma, Agapi Hakobyan, Kim Jackson, Candace Goh, WikiSysop, Evan Thomas and Scott Buxton
Definition/Description[edit | edit source]
| [1] |
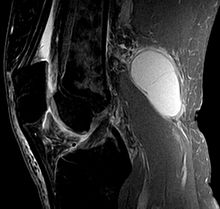
A Baker's cyst, popliteal cyst, is a swelling filled with fluid that is located in the popliteal region because it can be found incidentally during examination of the knee. It is called so after Dr. William Baker who first described this condition in 1877. Ganglia which are benign cystic tumors, originate from synovial tissue. It can occur mostly at the wrist, hand, foot, and knee which is known as popliteal cyst[2][3].
Popliteal cysts (Baker cyst) are commonly seen in children and are different than in adults. They are cystic masses filled with gelatinous material that develop in the popliteal fossa, are usually asymptomatic, and are not related to intra-articular pathology. Spontaneous resolution usually occurs, although the process can take several years.
Clinically Relevant Anatomy[edit | edit source]
A Baker’s cyst is an enlarged bursa that is normally located between the medial head of the gastrocnemius and a capsular reflection of the semimembranousus named oblique popliteal ligament.
The two requirements for cyst formation are the anatomical communication and a chronic effusion . Knee joint effusions may replete the gastrocnemius-semimembranosus bursa with synovial fluid and if the fluid outflow is hindered by a unidirectional mechanism, the gastrocnemius-semimembranosus bursa enlarges giving rise to a pseudocystic cavity referred to as a Baker’s cyst[2].
Epidemiology /Etiology[edit | edit source]
A Baker’s cyst occurs if there is an underlying problem with the knee for example osteoarthritis, rheumatoid arthritis, meniscus pathology, effusion, ACL tears, knee pain and other symptoms[2].
Symptoms can include
- pain,
- swelling and
- tightness behind the knee.
The cyst can vary in size from a very small cyst to a large one. Smaller cysts may be asymptomatic, but change in size is very common. Especially in smaller cysts, a septum may exist separating the semimembranosus and gastrocnemius components. This may function as a flap valve allowing fluid to enter a popliteal cyst and not to exit it. Cyst may range in size from small, from clinically not palpable to large masses causing visible swelling of the patient’s knee .If the cyst is large, it may result in mechanical problems in knee flexion and limiting mobility.
Differential Diagnosis[edit | edit source]
If the popliteal cyst becomes infected, it can mostly lead to a painful mass behind the knee. In such cases it could be difficult to make a diagnosis and the infected cyst can be mistaken for a neoplasm. The cyst can rupture (split open) resulting in severe calf pain, decreased motion at the ankle and cause similar symptoms as a deep vein thrombosis (evident on ultrasound or venogram).
It is important to diagnose a ruptured Baker’s cyst early and to differentiate it from
- thrombophlebitis
- popliteal aneurysm
- inflammatory arthritis
- medial gastrocnemius strain
- soft-tissue tumor or muscle tear
to determine the best treatment and avoid complications such as compartment syndrome[4].
Diagnostic Procedures[edit | edit source]
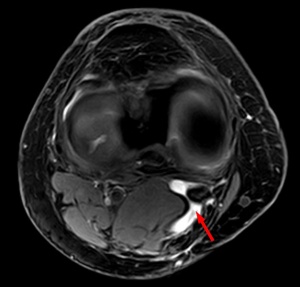
An ultrasound or arthrography scan is the initial derangement method that can diagnose a Baker’s cyst and can exclude deep vein thrombosis. MRI or CT scan are the imaging methods which can not only localize the cyst, but have also the possibility to identify associated internal derangement of the knee[5].
The size of the cyst or pain can cause limitations in range of motion. In rare cases there will be signs and symptoms of a meniscal tear which can be tested by McMurray test[4].
Examination
[edit | edit source]
Medical Management[edit | edit source]
The popliteal cyst often gets better and disappears by itself over time. The cyst can be removed with surgery if it becomes very large or causes symptoms such as discomfort, stiffness or painful swelling[4].
Rest can temper the pain that bursa is causing. Treatment of Baker’s cyst consists taking non-steroidal anti-inflammatory drugs (NSAID) to alleviate the pain, restrict movement, alternate ice.
If the pain persist, an injection with a solution of anaesthetic and steroid can be advised which can relieve pain, but not prevent recurrence of the cyst.
Physical Therapy Management[edit | edit source]
An ice massage of 15 minutes every 4-7 hours will reduce the inflammation. The treatment is based on the principles of R.I.C.E (rest, ice, compression, and elevation) followed by some muscle-conditioning exercises.
Rehabilitation program can improve the control of the knee joint by range of motion exercises. It will increase the motion of the joint as well as increase flexibility. The physiotherapist will give a mobility, a hamstring stretching program and a concurrent quadriceps strengthening program that has to repeated several times a day. This will result in less pain at about 6-8 weeks.
| [6] | [7] |
Resources[edit | edit source]
Jin Hwan Ahn, M.D., Sang Hak Lee, M.D., Jae Chul Yoo, M.D., Moon Jong Chang, M.D., and Yong Serk Park, M.D. Arthroscopic Treatment of Popliteal Cysts: Clinical and Magnetic Resonance Imaging Results. Original Article With Video Illustration. 2010 Oct;26(10):1340-7. Epub 2010 Sep 24. Quality level C1(therapeutically series)
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1b_xvYg-6HNXFKelWXZmLFI2yE_nSm301Kfc6KE8Z4wepON9N4|charset=UTF-8|short|max=10: Error parsing XML for RSS
Read 4 Credit[edit | edit source]
|
Would you like to earn certification to prove your knowledge on this topic? All you need to do is pass the quiz relating to this page in the Physiopedia member area. |
References[edit | edit source]
- ↑ nabil ebraheim. Baker's Cyst - Everything You Need To Know - Dr. Nabil Ebraheim. Available from: http://www.youtube.com/watch?v=kH6of0ipfXw [last accessed 12/09/14]
- ↑ 2.0 2.1 2.2 Peter Larking. Causation Review – Popliteal Cysts/Baker’s Cyst of the knee. Governance, Policy and Research, ACC, 03- 2011. Quality level A2 (causation review)
- ↑ Walter B. Greene, MD - editor. 2nd edition. USA(2001). Essentials of Muscluloskeletal Care. Section 6, Knee and Lower leg - popliteal cyst (p.397-398)fckLRQuality level D (opinion of experts)
- ↑ 4.0 4.1 4.2 WC Torreggiani, K Al-Ismail, PL Munk, C Roche, C Keogh, S Nicolaou, LP Marchinkow. The imaging spectrum of Baker's (Popliteal) cysts. Clinical Radiology. 2002 Aug;57(8):681-91. Quality level A2 (review)
- ↑ Calvisi, Vittorio, Lupparelli, Stefano, Giuliani, Pierandrea. Arthroscopic all-inside suture of symptomatic Baker's cysts: a technical option for surgical treatment in adults. Knee Surgery Sports Traumatology Arthroscopy. 2007 Dec;15(12):1452-60. Epub 2007 Aug 1. Quality level C3 (not strong evidence)
- ↑ Westside-Medical. Baker's Cyst Treatment Feat. Dr. Blake Staker Westside-Medical. Available from: http://www.youtube.com/watch?v=xjX9jBWXLkM [last accessed 12/09/14]
- ↑ TheGVideo. Massaging bakers cyst. Available from: http://www.youtube.com/watch?v=ETorNuyS4JA [last accessed 12/09/14]