Back Education Program: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) No edit summary |
||
| (173 intermediate revisions by 14 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original Editors '''- Hannah Anderson, Dan McCoy, Rebecca Porter and Millie Ware | '''Original Editors ''' - Hannah Anderson, Dan McCoy, Rebecca Porter and Millie Ware | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Introduction == | |||
[[Image:Backpain2.png|right]]Globally, low back pain (along with migraine, age-related and other hearing loss, iron-deficiency anaemia, and major depressive disorder) were the five leading causes of YLDs in 2016, contributing 57·6 million (95% uncertainty interval [UI].<ref>Vos T, Abajobir AA, Abate KH, Abbafati C, Abbas KM, Abd-Allah F, Abdulkader RS, Abdulle AM, Abebo TA, Abera SF, Aboyans V. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet. 2017 Sep 16;390(10100):1211-59.</ref> | |||
|- | |||
Pain is not always a bad thing! Pain is the body's way to receive messages that there is a threat or something is wrong. | |||
The [[Brain Anatomy|brain]] processes this pain message and responds in a way that will reduce the threat. Initially, when tissues are injured, the nerves in the back (which have sensors) send messages of pain to the brain. The brain, very much like a processor in a computer, takes this message or code and decides where it should be stored and which systems should deal with it. Those systems in the brain then send messages back through nerve pathways to the muscles to tell them to move the back gently and carefully so those tissues can heal. It is an amazing system in the brain, influenced by chemicals and the manner in which the pain messages are routed or circuited. Over time tissues heal and the healing process begins immediately. Usually within two weeks any swelling that caused the sensors to light up and send pain messages to the brain has gone away. Most tissues heal completely within four to six weeks. | |||
The brain can be sensitized or desensitized by several things including our beliefs about pain and our understanding of how the body heals. You may have heard stories about how soldiers in war times have stated they felt no pain even with limb amputation. All they remembered feeling was joy, knowing they weren't dead and would get to go home. This is an example of how the brain can interpret pain and desensitize the response It can be sensitized or over-reactive by our emotions, events that occur in our lives that may increase feelings of anxiousness or fear. The amount of pain experienced doesn't always equal the amount of tissue damage. In fact tissues may have healed completely but pain can still be felt.. | |||
The good news is that these processes are normal and there are things that can help calm the nerves down that are sensitized or on call. | |||
= | == Clinically Relevant Anatomy. == | ||
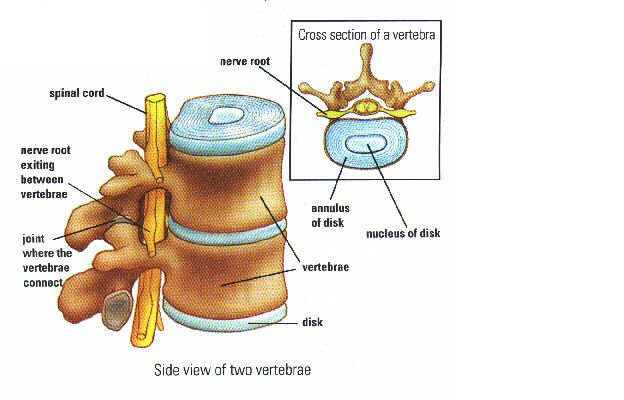
The spine is wonderfully designed to allow movement. It is also designed to help absorb and distribute forces from everyday activities.<ref name="Physicians">Physicians Plus.Vertebrae. http://www.physiciansplus.net (accessed September 16 2013).</ref> | |||
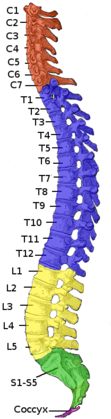
The spine is made up of 33 small bones called vertebrae. Together, they form what is know as the vertebral column. There are 7 vertebrae in the cervical region which is your neck; 12 vertebrae in the thoracic region which is your upper back; 5 vertebrae in the lumbar spine; and 5 sacral vertebrae and 4 coccyx which are located below that. | |||
Between each of the vertebrae is a disc that binds the vertebra together like a very strong ligament. It acts as a cushion and a shock absorber. These intervertebral discs are made up of two parts - the nucleus pulposus and the annulus fibrosis. The nucleus pulposus is in the middle of the disc and is jelly-like due to its large water content; it is composed of up to 80% water! The annulus fibrosis surrounds this nucleus and so forms the outer part of the disc. These discs play an important role in keeping the back healthy! | |||
Other important parts of the spine: | |||
*Facet joint: the joint where the vertebrae connect | |||
*Spinal cord | |||
*Nerves: diverge off of the spinal cord and run to different parts of the body | |||
<div class="flex-row row"> | |||
<div class="col-xs-12 col-md-6 col-lg-6">[[Image:Anatomy1.png|left]] | |||
</div> | |||
<div class="col-xs-12 col-md-6 col-lg-6">[[File:Sagittal section of the cervical spine Primal.png]] | |||
</div> | |||
</div> | |||
The spine has three natural curves that begin to develop from the moment a baby lifts his/her head and gravity begins to work on the body. The curves keep the spine from being completely rigid and help the spine to tolerate a little bit more compression. To understand the normal curves of a spine, there are 2 terms you need to know—lordosis and [[kyphosis]]. Lordosis is when the spine curves inward and a kyphosis is when the spine curves outward. The cervical portion of the spine is in a lordosis, the thoracic portion is in a kyphosis, and the lumbar spine is in a lordosis. The curves of the back increase the load bearing capacity of the spine. | |||
The spine has 4 main motions—forward bending, backward bending, sidebending, and rotation. These motions can also be coupled. For instance, you can have forward bending with rotation or backward bending with sidebending. Below, we demonstrate these motions and report typical lumbar spine active range of motion. | |||
{| width="240" cellspacing="1" cellpadding="1" border="1" align="center" | |||
|- | |||
| Forward Bending 60 degrees | |||
| Backward Bending 25 degrees | |||
| Lateral Flexion 25 degrees | |||
| Rotation 30 degrees | |||
|- | |||
| [[Image:2013 flexion.png|112x170px]] | |||
| [[Image:2013 extension.png|98x170px]] | |||
| [[Image:2013 sidebending.png|102x164px]] | |||
| [[Image:2013 rotation.png|106x175px]] | |||
|} | |||
== Muscles == | |||
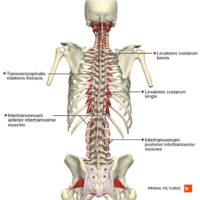
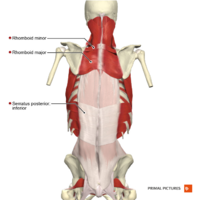
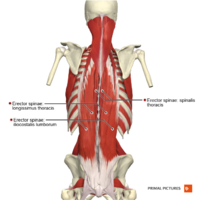
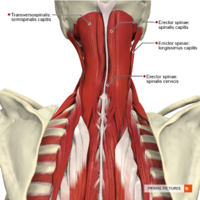
Many muscles work together to help make these spinal motions possible! These back muscles can be classified into three different layers - superficial, intermediate, and deep.<ref name="Tank">Tank P. Grant's Dissector. 15th ed. Little Rock, AR: Wolters Kluwer; 2013.</ref> The muscles produce spinal movements and also help to keep the spine stable. In order to keep these muscles healthy, it is important to stay active. | |||
<div class="row"> | |||
<div class="col-md-4">[[Image:Muscles_of_the_back_transversospinales_group_and_segmental_muscles_Primal.png|200px]]</div> | |||
<div class="col-md-4">[[Image:Muscles_of_the_back_intermediate_layer_Primal.png|200px]] </div> | |||
<div class="col-md-4">[[Image:Muscles_of_the_back_erector_spinae_group_Primal.png|200px]]</div> | |||
</div> | |||
== About Neck Pain == | |||
=== How Common is Neck Pain? === | |||
< | Here are a few statistics on the prevalence of neck pain<ref name="Ahern">Ahern Family Chiropractic. Seizures. http://ahernfamilychiro.com (accessed September 24 2013).</ref>: | ||
*[[Epidemiology of Neck Pain|Neck pain]] reported to be 2nd most common musculoskeletal disorder that leads to disability and injury claims<ref name="Olson">Olson, KA. Manual Physical Therapy of the Spine. St. Louis, MO: Saunders; 2009.</ref> | |||
*2002: 13.8% of population > 18 years old in U.S. reported neck pain<ref name="Olson" /> | |||
*Up to 50% of people with neck pain have ongoing symptoms for > 3 months, therefore are categorised as "Chronic" patients<ref>Mansfield M, Thacker M, Spahr N, Smith T. Factors associated with physical activity participation in adults with chronic cervical spine pain: a systematic review. PHYSIOTHERAPY [Internet]. [cited 2019 Feb 20];104(1):54–60. Available from: <nowiki>http://ezproxy.aut.ac.nz/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=edswsc&AN=000426458600008&site=eds-live</nowiki></ref> | |||
=== Anatomy of the Neck === | |||
[[File:Spine-in-colour.png|thumb|419x419px]] | |||
Just as with low back pain, it is important to understand the anatomy behind neck pain! The neck is anatomically separated into the upper cervical spine and the lower cervical spine. There are 7 vertebrae that make up the cervical spine. | |||
The first cervical vertebra (C1) is called the Atlas. It has no vertebral body or spinous process. This vertebra articulates with the Occiput, which is the base of the skull. This articulation is labeled as the OA joint; its primary motion is flexion and extension at the joint. It also performing side-bending with opposite rotation. | |||
The second cervical vertebra (C2) is called the [[Axis]]; it has a large spinous process. The articulation between the Atlas and Axis is called the AA(atlantoaxial) joint and its primary motion is rotation. | |||
The following pictures demonstrate the motions of the lower cervical spine (C3-C7) and report the typical active range of motion.<ref name="Olson" /> | |||
{| width="260" cellspacing="1" cellpadding="1" border="1" align="center" | |||
{| width=" | |||
|- | |- | ||
| | | Flexion: 54 degrees <br> | ||
| | | Extension: 77 degrees <br> | ||
| | | Sidebending: 45 degrees<br> | ||
| | | Rotation: 70-80 degrees<br> | ||
|- | |- | ||
| | | | ||
[[Image:Cervical flexion.png|169x117px]] | |||
| | | [[Image:2013 cervical extension.png|162x109px]] | ||
| | |||
[[Image:2013 cervical sidebending.png|181x129px]] | |||
| | |||
<br> [[Image:2013 cervical rotation.png|182x133px]] | |||
|} | |} | ||
<br> | |||
=== Muscles === | |||
< | [[Image:Muscles_of_the_cervical_region_intermediate_muscles_Primal.png|right|200px]] | ||
The muscle mentioned in the section ''About Back Pain'' also can play a role in neck pain, especially those muscles of the superficial layer. Also, deep inside the back of the neck are four important muscles called the suboccipital muscles.<ref name="Tank" /> | |||
==== There are certain factors that can increase the risk for neck pain ==== | |||
*Working at a desk that is ill fitting to the body | |||
*Working at a computer for long periods of time | |||
*Sitting with bad posture for long periods of time | |||
*Working on above head activities (i.e. painting) for long periods of time | |||
The [[Neck Pain Tool-kit: Step 1|Cervical Tool Kit]] to help identify or classify patients based on evidence informed interventions. | |||
== Causes of Back Pain == | |||
Back pain is becoming increasingly prevalent in our population. Pain is an indication that the body is working to protect that part of the body. Pain can be a good guide to the best healing behaviors; understanding pain can help to deal with it effectively.<ref name="Butler">Butler D, Moseley. Explain Pain. Adelaide City Way, SA: Noigroup Publications; 2003.</ref> Back pain can be caused by a multitude of structures, but the exact structure causing the pain cannot be identified. This is most likely because of the complex interactions of the brain and spinal nerves often times referred to as the Pain Matrix. | |||
Any structure in the back that has a nerve supply can send messages to the brain if it is injured. Back pain can come from the disc, facet joint, spinal nerve root, ligaments, muscles, bones, fascia or neurogenic claudication. | |||
=== Intervertebral Disc === | |||
The natural lordotic posture decreases the pressure on the disc compared to the straight posture which can put pressure on the disc and can push fluid from the nucleus pulposus into the vertebral body (schmorl’s nodes). It is important to differentiate herniated disc (space occupying) which refers into the leg vs other conditions (inflammation reaction, spasms, strains, facet syndrome) which are more localized in pain. | |||
Functional anatomy of the intervertebral disc:<ref name="Neumann">Neumann, DA. Kinesiology of the Musculoskeletal System: Foundations for Rehabilitation 2nd Edition. St. Louis, MO: Mosby Inc; 2010.</ref> | |||
*In forward bending or flexion, the disc bulges anteriorly/forwards and the nucleus pulposus goes posteriorly | |||
*In backward bending or extension, the disc bulges posteriorly/backwards and the nucleus pulposus goes anteriorly | |||
*In sidebending or lateral flexion, the disco bulges towards the side in which in movement is occurring (eg. right sidebending, right disc bulge) | |||
*If the disc looses height, can put pressure on the facet joints, possibly increasing the risk of arthritis, and put pressure the nerve roots by decreasing the foraminal height | |||
Injury to the disc: | |||
*Protrusion: disc bulge posteriorly without rupture of annulus fibrosis | |||
*Prolapse: outermost fibers of the annulus fibrosis contain the nucleus | |||
*Extrusion: annulus fibrosis is perforated and discal material into the epidural space | |||
*Sequestrated: fragments of annulus and nucleus are outside the disc proper
(can lead to pressure on neurological tissues and cause an inflammatory response) | |||
Anterior disc herniation:<ref name="Neumann" /> | |||
*Occurs when someone is in extension, or leaning backward, which puts pressure on the anterior/front of the disc causing it to herniated/prolapse/bulge. | |||
*This can put pressure on nerves in the lower abdomen causing weakness or numbness, anterior longitudinal ligament, vertebral body, and [[Transversus Abdominis|Transverse Abdominus]] which can all cause pain. | |||
Posterior disc herniation:<ref name="Neumann" /> | |||
*Occurs when some is in flexion, leaning forward, which puts pressure on the posterior/back of the disc causing it to herniate/prolapse/bulge. | |||
*This can put pressure on your spinal cord or nerve root causing pain/weakness/numbness/reduced reflexes and the posterior longitudinal ligament causing pain | |||
The | '''For Physical Therapists''': What information should you be collecting when treating a patient with low back pain? The [http://www.physio-pedia.com/Treatment_Based_Classification_Approach_to_Low_Back_Pain TREATMENT BASED CLASSIFICATION SYSTEM] has been associated with excellent outcomes<ref name="Olson" /> | ||
== Management of Low Back Pain == | |||
Treatment may include; | |||
*Proper posture | |||
*Aerobic conditioning | |||
*[[Traction for Neck Pain CPR|Traction]] | |||
*Manual therapy ([[Mobilization Grades|mobilizations]], [[stretching]]) | |||
*Self-stretching | |||
*Exercise | |||
== Physical Therapy Management of Low Back Pain == | |||
Stanton et al created a treatment based classification based system for low back pain.<ref name="Stanton">Stanton T et al. Evaluation of a Treatment-Based Classification Algorithm for Low Back Pain: A Cross-Sectional Study. Physical Therapy. 2011; 91:496-509.</ref> | |||
Exercise is a significant factor in the rehabilitation process<ref name="Hicks">Hicks GE., Fritz JM., Delitto A., McGill SM. Preliminary development of a clinical prediction rule for determining which patients with low back pain will respond to a stabilization exercise program, Arch Phys Med Rehabilitation 2005; 86; 1753-1762</ref>. Studies have found that exercise is more effective at improving function and decreasing pain than seeing a family physician. <ref name="Hettinga">Hettinga et al. A systematic review and synthesis of higher quality evidence of the effectiveness of exercise interventions for non-specific low back pain of at least 6 weeks' duration. Physical Therapy Reviews [serial online]. September 2007;12(3):221-232. Available from: CINAHL with Full Text, Ipswich, MA. Accessed October 6, 2013.</ref> Goal of exercises: to restore strength and endurance of the Transverse Abdominus and Lumbar Multifidus. | |||
=== Abdominal bracing === | |||
*Abdominal bracing with heel slides | |||
[[Image:Heel slide 2.png|293x155px]] [[Image:Heel slide 1.png|353x155px]] | |||
*Abdominal bracing with leg lifts | |||
[[Image:Straight leg raise.png|239x137px]] | |||
<br> | <br> | ||
*Abdominal bracing with bridges | |||
* | |||
[[Image:Bridge.png|255x135px]] | |||
<br> | |||
* | *Abdominal bracing with standing row exercise | ||
[[Image:Scapular row.png|131x244px]]<br> | |||
<br> | |||
*Abdominal bracing with walking/standing | |||
<br> | |||
=== Erector Spinae/Multifidus === | |||
* | *Quadruped arm lifts and bracing | ||
[[Image:Quadruped with single arm raise.png|300x148px]] | |||
* | *Quadruped leg lifts and bracing | ||
[[Image:Quadruped with single leg raise.png|266x150px]] | |||
<br> | |||
*Quadruped alternate arms and legs with bracing | |||
* | |||
[[Image:Quadruped with single arm and leg raise.png|300x116px]] | |||
<br> | <br> | ||
=== Extension Based Exercises === | |||
[[McKenzie Method|Mckenzie Exercises]] | |||
Cow Stretch | |||
[[Image:Cow stretch.png|215x135px]] | |||
Prone Press Ups | |||
[[Image:Prone press up.png|217x111px]] | |||
<br> | <br> | ||
=== Flexion Based Exercises === | |||
[[Williams Flexion Exercise]] - 1) the pelvic tilt 2) the single knee to chest stretch 3) double knee to chest 4) partial sit-up 5) hamstring stretch 6) hip flexor stretch and 7) squatting. | |||
Cat Stretch<br> | |||
[[Image:Cat stretch.png|218x130px]]<br> | |||
Prayer Stretch | |||
[[Image:Prayer stretch.png|218x90px]]<br> | |||
Single Knee to Chest | |||
[[Image:Single knee to chest.png|220x118px]] | |||
= | === Lumbar Stabilization Exercise === | ||
Hamstring stretch | |||
Pelvic Tilts in supine lying or standing close to the wall | |||
<br> | <br> | ||
=== Specific Exercise Category <ref name="Browder">Browder D, Childs J, Cleland J, Fritz J. Effectiveness of an Extension-Oriented Treatment Approach in a Subgroup of Subjects with Low Back Pain: A Randomized Clinical Trial. Physical Therapy. 2007; 87: 1608-1617.</ref> === | |||
<u>Subjective:</u> | |||
*Symptoms distal to buttocks | |||
<u>Objective:</u> | <u>Objective:</u> | ||
*Pain centralizes with a specific movement (can be flexion or extension) | |||
== Proper Lifting Techniques == | |||
Squat lift<br> | |||
<br> | #Plan The Lift: Know how heavy the object is. Clear a path and know where the object is to be placed. | ||
#Lift Close to the body: This will make the body stronger and more stable. Ensure there is a firm hold on the object and balance it close to the body. | |||
#Feet shoulder width apart: This allows for a solid base of support. | |||
#Bend the knees while keeping the back straight: Avoid any twisting motions. | |||
#Tighten the stomach muscles: This will hold the back in good alignment and prevent excessive force on the spine. Avoid breath holding. | |||
#Lift with the legs: The leg muscles are stronger than the back so use them. | |||
#Avoid straining, get help: Get help if the object is too heavy or it is in an awkward position. <br> | |||
[[Image:Squat 1.png|186x224px]] [[Image:Squat 2.png|186x225px]] [[Image:Squat 3.png|179x225px]] [[Image:Squat 4.png|166x225px]]<br> | |||
Squat - Remember to: | |||
*Keep back straight | |||
*Knees behind toes | |||
*Keep knees parallel | |||
< | <br> Golfer’s Lift | ||
*The Golfer’s lift is another lifting technique that is useful for picking something off the floor | |||
*This works best when using something like a chair or table for support when bending | |||
*Kick out the unsupported leg - This helps to keep the back straight | |||
2 | [[Image:Golfers lift 1.png|188x228px]] [[Image:Golfers lift 2.png|200x230px]] | ||
Diagonal Standing | |||
*Stand with one foot slightly in front of the other and distribute the weight evenly between both legs | |||
*This is a preferred position over straight standing | |||
*Avoid putting all of the weight onto one leg while standing. | |||
< | === Aerobic Activity <ref>Thompson WR, Gordon NF, Pescatello LS, eds. ACSM's Guidelines for Exercise Testing and Prescription. 8th ed. Baltimore: American College of Sports Medicine; 2010.</ref> === | ||
Types: Walking, jogging, running, cycling, swimming, climbers, steppers, elliptical machines, ski machines, aerobic dance<br>Warm up/cool down – low to moderate activity<br> | |||
* | *5-10 minutes of warm up (adjust to demands placed on the body) | ||
* | *5-10 minutes of cool down (recovery of heart rate and BP) | ||
*10 minutes of stretching AFTER the warm up OR cool down<br> | |||
* | |||
ACSM Guidelines:= | |||
*Frequency: 5 days/week | |||
*Duration: 150 minutes per week (minimum) | |||
*Intensity: 40-60% HRmax (HRmax = 220-age) | |||
Benefits of exercise are improved joint health due to low impact exercises, increase bone density due to weight bearing exercises, improving energy, reducing health risks, improving circulation, and reducing stress and improving your mood. Aerobic activity is equally effective at reconditioning muscles as exercise and can also help in decreasing pain, improving your mood, and improving your functional capabilities.<ref>Hettinga D, Jackson A, Moffett J, May S, Mercer C, Woby S. A systematic review and synthesis of higher quality evidence of the effectiveness of exercise interventions for non-specific low back pain of at least 6 weeks' duration. Physical Therapy Reviews [serial online]. September 2007;12(3):221-232. Available from: CINAHL with Full Text, Ipswich, MA. Accessed October 6, 2013.</ref> Lack of exercise increases your risk of obesity and other co-morbidities increases; this can lead to increased pressure on the spine and decreased flexibility. | |||
== Management of Neck Pain? == | |||
There are specific treatments based on each classification of neck pain: <ref name="Olson" /> | |||
== Cervical Hypomobility == | |||
* | *AROM exercises | ||
* | *Cervical and thoracic mobilization/manipulation isometric or thrust manipulation techniques | ||
* | *Nonthrust manipulation | ||
== Cervical Radiculopathy == | |||
* | *Cervical traction (manual/mechanical) | ||
* | *[[Upper Limb Tension Tests (ULTTs)|Upper Limb Tension Tests]] AROM | ||
* | *Thoracic spine manipulation | ||
*Postural exercises | |||
== Cervical Instability == | |||
* | *Postural education | ||
* | *Cervical stabilization exercise program | ||
*Mobilization/manipulation above and below hypermobilities | |||
*Ergonomic corrections | |||
== Acute Pain (Whiplash) == | |||
*Gentle AROM within patient tolerance | |||
*Activity modification to control pain | |||
*Relative rest | |||
*Physical modalities | |||
*Intermittent use of cervical collar | |||
*Gentle manual therapy and exercises, but avoidance of pain-inducing manual therapy techniques or exercises | |||
== Cervicogenic Headache == | |||
*Cervical and thoracic mobilization/manipulation | |||
*Strengthening neck and postural muscles | |||
*Postural education | |||
== Physical Therapy Management of Neck Pain == | |||
Exercise! | |||
1). Pain | Evidence from the literature says that exercise has a significant effect in reducing chronic non-specific neck pain for short term (<1 month) and intermediate term (1-6 months) <ref name="Bertozzi">Bertozzi et. al. Effect of Therapeutic Exercise on Pain and Disability in the Management of Chronic Nonspecific Neck Pain: Systematic Review and Meta-Analysis of Randomized Trials. Phys Ther. 2013; 93:1026-1036</ref> | ||
=== Neck Exercises === | |||
*OA flexion (chin tuck): A slight nod while keeping your head in neutral | |||
[[Image:OA extension.png|178x196px]][[Image:OA chin tuck.png|185x198px]] | |||
*Flexion with chin tuck: While lying on your back tuck in your chin, lift off until your head clears the table and hold for 3-5 seconds maintaining the chin tuck | |||
[[Image:Chin tuck with flexion.png|191x156px]] | |||
*Extension with chin tuck: While laying on your stomach tuck your chin, lift your head off table while maintaining chin tuck and hold 3-5 seconds | |||
[[Image:Chin tuck in extension.png|165x130px]] | |||
*4-way Isometrics: Lightly press into your hand in flexion, extension, side bending, and rotation | |||
[[Image:Cerival flexion isometric.png|170x183px|Flexion Isometric]] [[Image:Cervical extension isometric.png|175x183px|Extension Isometric]] [[Image:Cervical sb isometric.png|183x183px|Sidebending Isometric]] [[Image:Cervical rotation isometric.png|189x179px|Rotation Isometric]]<br> | |||
Exercises for Scapular Stabilizers (muscles attached to your shoulder blade)<br> | |||
*Middle Trapezius: With band or lying on stomach, Thumb pointing in the direction exercise is moving, Pinch shoulder blades | |||
[[Image:Middle trap.png|182x202px]]<br> | |||
*Lower Trapezius: Lying down making a half Y bring your shoulder blade back and down | |||
[[Image:Lower trap.png|188x177px]]<br> | |||
*Seated Row: Upright Sitting Posture, Pull at elbows, Pinch shoulder blades together | |||
[[Image:Seated row.png|196x291px]]<br> | |||
*External Rotation: Elbows at sides, Thumbs pointing out, Shoulders back, Rotate outward | |||
[[Image:Shoulder ER 1.png|158x175px]] [[Image:Shoulder ER 2.png|216x176px]] | |||
<br> | |||
*Scapular Clock: Turn shoulder blade into a clock, Move shoulder blade to each number, retraction and depression are critical, Numbers 9, 8, 7, 6 are important | |||
[[Image:Scapular clock.png|272x219px]] | |||
<br> | |||
=== Stretches === | |||
{| width="100%" cellspacing="1" cellpadding="1" border="0" align="center" | |||
|- | |||
| [[Image:Upper trap.png|thumb|center|200px|Trapezius/Sternocleidomastoid]] | |||
| [[Image:Scalene stretch.png|thumb|center|200px|Scalenes]] | |||
| [[Image:Levator stretch.png|thumb|center|200px|Levator Scapulae]] | |||
|} | |||
== Don't forget the thoracic spine! == | |||
A clinical prediction rule was developed to help classify patients with mechanical neck pain that will experience early success from thoracic spine manipulation. Six variables were found: <ref name="Cleland">Cleland et al. Development of a Clinical Prediction Rule for Guiding Treatment of a Subgroup of Patients with Neck Pain: Use of Thoracic Spine Manipulation, Exercise, and Patient Education. Phys Ther. 2007; 87: 9-23.</ref> | |||
1. Symptoms < 30 days | 1. Symptoms < 30 days | ||
| Line 517: | Line 419: | ||
6. Cervical extension < 30 degrees | 6. Cervical extension < 30 degrees | ||
If | If a patient demonstrates 3 of the 6 variables the chance of experiencing a successful outcome improves from 54% to 86%. If a patient has 4 of the 6 variables the chance of a successful outcome rises to 95%. | ||
== Resources | == Resources == | ||
Chou, MD Lumbar imaging guidelines | Chou, MD Lumbar imaging guidelines | ||
* | *http://www.lni.wa.gov/claimsins/Files/OMD/MedTreat/Imaging/LBchecklist.pdf <br> | ||
APTA Low Back Pain Infographic | APTA Low Back Pain Infographic | ||
* | *http://www.moveforwardpt.com/LowBackPain/Infographic/Default.aspx<br> | ||
Find a PT on the American Physical Therapy Association website | Find a PT on the American Physical Therapy Association website | ||
* | *http://www.apta.org/apta/findapt/index.aspx?navID=10737422525<br> | ||
<br> | |||
Orthopaedic Section - APTA: Clinical Guidelines for Neck Pain<br> | |||
*http://www.orthopt.org/ICF/Neck%20Pain%20Clinical%20Guideline%20-%20JOSPT%20-%20Sept%202008.pdf<br> | |||
Orthopaedic Section - APTA: Clinical Guidelines for Low Back Pain<br> | |||
*http://www.orthopt.org/uploads/content_files/ICF/Updated_Guidelines/Low_Back_Pain_Clinical_Practice_Guidelines___JOSPT_2012.pdf | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Lumbar_Spine]] | |||
[[Category:Interventions]] | |||
[[Category:Lumbar Spine - Interventions]] | |||
[[Category:Pain]] | |||
[[Category:Musculoskeletal/Orthopaedics]] | |||
Latest revision as of 17:19, 29 February 2024
Original Editors - Hannah Anderson, Dan McCoy, Rebecca Porter and Millie Ware
Top Contributors - Rebecca Porter, Hannah Anderson, Elaine Lonnemann, Laura Ritchie, Millie Deason, Kim Jackson, Daniel McCoy, Admin, Evan Thomas, Shreya Pavaskar, WikiSysop, Vidya Acharya, Lucinda hampton and Kalyani Yajnanarayan
Introduction[edit | edit source]
Globally, low back pain (along with migraine, age-related and other hearing loss, iron-deficiency anaemia, and major depressive disorder) were the five leading causes of YLDs in 2016, contributing 57·6 million (95% uncertainty interval [UI].[1]
Pain is not always a bad thing! Pain is the body's way to receive messages that there is a threat or something is wrong.
The brain processes this pain message and responds in a way that will reduce the threat. Initially, when tissues are injured, the nerves in the back (which have sensors) send messages of pain to the brain. The brain, very much like a processor in a computer, takes this message or code and decides where it should be stored and which systems should deal with it. Those systems in the brain then send messages back through nerve pathways to the muscles to tell them to move the back gently and carefully so those tissues can heal. It is an amazing system in the brain, influenced by chemicals and the manner in which the pain messages are routed or circuited. Over time tissues heal and the healing process begins immediately. Usually within two weeks any swelling that caused the sensors to light up and send pain messages to the brain has gone away. Most tissues heal completely within four to six weeks.
The brain can be sensitized or desensitized by several things including our beliefs about pain and our understanding of how the body heals. You may have heard stories about how soldiers in war times have stated they felt no pain even with limb amputation. All they remembered feeling was joy, knowing they weren't dead and would get to go home. This is an example of how the brain can interpret pain and desensitize the response It can be sensitized or over-reactive by our emotions, events that occur in our lives that may increase feelings of anxiousness or fear. The amount of pain experienced doesn't always equal the amount of tissue damage. In fact tissues may have healed completely but pain can still be felt..
The good news is that these processes are normal and there are things that can help calm the nerves down that are sensitized or on call.
Clinically Relevant Anatomy.[edit | edit source]
The spine is wonderfully designed to allow movement. It is also designed to help absorb and distribute forces from everyday activities.[2]
The spine is made up of 33 small bones called vertebrae. Together, they form what is know as the vertebral column. There are 7 vertebrae in the cervical region which is your neck; 12 vertebrae in the thoracic region which is your upper back; 5 vertebrae in the lumbar spine; and 5 sacral vertebrae and 4 coccyx which are located below that.
Between each of the vertebrae is a disc that binds the vertebra together like a very strong ligament. It acts as a cushion and a shock absorber. These intervertebral discs are made up of two parts - the nucleus pulposus and the annulus fibrosis. The nucleus pulposus is in the middle of the disc and is jelly-like due to its large water content; it is composed of up to 80% water! The annulus fibrosis surrounds this nucleus and so forms the outer part of the disc. These discs play an important role in keeping the back healthy!
Other important parts of the spine:
- Facet joint: the joint where the vertebrae connect
- Spinal cord
- Nerves: diverge off of the spinal cord and run to different parts of the body
The spine has three natural curves that begin to develop from the moment a baby lifts his/her head and gravity begins to work on the body. The curves keep the spine from being completely rigid and help the spine to tolerate a little bit more compression. To understand the normal curves of a spine, there are 2 terms you need to know—lordosis and kyphosis. Lordosis is when the spine curves inward and a kyphosis is when the spine curves outward. The cervical portion of the spine is in a lordosis, the thoracic portion is in a kyphosis, and the lumbar spine is in a lordosis. The curves of the back increase the load bearing capacity of the spine.
The spine has 4 main motions—forward bending, backward bending, sidebending, and rotation. These motions can also be coupled. For instance, you can have forward bending with rotation or backward bending with sidebending. Below, we demonstrate these motions and report typical lumbar spine active range of motion.
| Forward Bending 60 degrees | Backward Bending 25 degrees | Lateral Flexion 25 degrees | Rotation 30 degrees |

|

|

|

|
Muscles[edit | edit source]
Many muscles work together to help make these spinal motions possible! These back muscles can be classified into three different layers - superficial, intermediate, and deep.[3] The muscles produce spinal movements and also help to keep the spine stable. In order to keep these muscles healthy, it is important to stay active.
About Neck Pain[edit | edit source]
How Common is Neck Pain?[edit | edit source]
Here are a few statistics on the prevalence of neck pain[4]:
- Neck pain reported to be 2nd most common musculoskeletal disorder that leads to disability and injury claims[5]
- 2002: 13.8% of population > 18 years old in U.S. reported neck pain[5]
- Up to 50% of people with neck pain have ongoing symptoms for > 3 months, therefore are categorised as "Chronic" patients[6]
Anatomy of the Neck[edit | edit source]
Just as with low back pain, it is important to understand the anatomy behind neck pain! The neck is anatomically separated into the upper cervical spine and the lower cervical spine. There are 7 vertebrae that make up the cervical spine.
The first cervical vertebra (C1) is called the Atlas. It has no vertebral body or spinous process. This vertebra articulates with the Occiput, which is the base of the skull. This articulation is labeled as the OA joint; its primary motion is flexion and extension at the joint. It also performing side-bending with opposite rotation.
The second cervical vertebra (C2) is called the Axis; it has a large spinous process. The articulation between the Atlas and Axis is called the AA(atlantoaxial) joint and its primary motion is rotation.
The following pictures demonstrate the motions of the lower cervical spine (C3-C7) and report the typical active range of motion.[5]
| Flexion: 54 degrees |
Extension: 77 degrees |
Sidebending: 45 degrees |
Rotation: 70-80 degrees |

|
Muscles[edit | edit source]
The muscle mentioned in the section About Back Pain also can play a role in neck pain, especially those muscles of the superficial layer. Also, deep inside the back of the neck are four important muscles called the suboccipital muscles.[3]
There are certain factors that can increase the risk for neck pain[edit | edit source]
- Working at a desk that is ill fitting to the body
- Working at a computer for long periods of time
- Sitting with bad posture for long periods of time
- Working on above head activities (i.e. painting) for long periods of time
The Cervical Tool Kit to help identify or classify patients based on evidence informed interventions.
Causes of Back Pain[edit | edit source]
Back pain is becoming increasingly prevalent in our population. Pain is an indication that the body is working to protect that part of the body. Pain can be a good guide to the best healing behaviors; understanding pain can help to deal with it effectively.[7] Back pain can be caused by a multitude of structures, but the exact structure causing the pain cannot be identified. This is most likely because of the complex interactions of the brain and spinal nerves often times referred to as the Pain Matrix.
Any structure in the back that has a nerve supply can send messages to the brain if it is injured. Back pain can come from the disc, facet joint, spinal nerve root, ligaments, muscles, bones, fascia or neurogenic claudication.
Intervertebral Disc[edit | edit source]
The natural lordotic posture decreases the pressure on the disc compared to the straight posture which can put pressure on the disc and can push fluid from the nucleus pulposus into the vertebral body (schmorl’s nodes). It is important to differentiate herniated disc (space occupying) which refers into the leg vs other conditions (inflammation reaction, spasms, strains, facet syndrome) which are more localized in pain.
Functional anatomy of the intervertebral disc:[8]
- In forward bending or flexion, the disc bulges anteriorly/forwards and the nucleus pulposus goes posteriorly
- In backward bending or extension, the disc bulges posteriorly/backwards and the nucleus pulposus goes anteriorly
- In sidebending or lateral flexion, the disco bulges towards the side in which in movement is occurring (eg. right sidebending, right disc bulge)
- If the disc looses height, can put pressure on the facet joints, possibly increasing the risk of arthritis, and put pressure the nerve roots by decreasing the foraminal height
Injury to the disc:
- Protrusion: disc bulge posteriorly without rupture of annulus fibrosis
- Prolapse: outermost fibers of the annulus fibrosis contain the nucleus
- Extrusion: annulus fibrosis is perforated and discal material into the epidural space
- Sequestrated: fragments of annulus and nucleus are outside the disc proper (can lead to pressure on neurological tissues and cause an inflammatory response)
Anterior disc herniation:[8]
- Occurs when someone is in extension, or leaning backward, which puts pressure on the anterior/front of the disc causing it to herniated/prolapse/bulge.
- This can put pressure on nerves in the lower abdomen causing weakness or numbness, anterior longitudinal ligament, vertebral body, and Transverse Abdominus which can all cause pain.
Posterior disc herniation:[8]
- Occurs when some is in flexion, leaning forward, which puts pressure on the posterior/back of the disc causing it to herniate/prolapse/bulge.
- This can put pressure on your spinal cord or nerve root causing pain/weakness/numbness/reduced reflexes and the posterior longitudinal ligament causing pain
For Physical Therapists: What information should you be collecting when treating a patient with low back pain? The TREATMENT BASED CLASSIFICATION SYSTEM has been associated with excellent outcomes[5]
Management of Low Back Pain[edit | edit source]
Treatment may include;
- Proper posture
- Aerobic conditioning
- Traction
- Manual therapy (mobilizations, stretching)
- Self-stretching
- Exercise
Physical Therapy Management of Low Back Pain[edit | edit source]
Stanton et al created a treatment based classification based system for low back pain.[9]
Exercise is a significant factor in the rehabilitation process[10]. Studies have found that exercise is more effective at improving function and decreasing pain than seeing a family physician. [11] Goal of exercises: to restore strength and endurance of the Transverse Abdominus and Lumbar Multifidus.
Abdominal bracing[edit | edit source]
- Abdominal bracing with heel slides
- Abdominal bracing with leg lifts
- Abdominal bracing with bridges
- Abdominal bracing with standing row exercise
- Abdominal bracing with walking/standing
Erector Spinae/Multifidus[edit | edit source]
- Quadruped arm lifts and bracing
- Quadruped leg lifts and bracing
- Quadruped alternate arms and legs with bracing
Extension Based Exercises[edit | edit source]
Cow Stretch
Prone Press Ups
Flexion Based Exercises[edit | edit source]
Williams Flexion Exercise - 1) the pelvic tilt 2) the single knee to chest stretch 3) double knee to chest 4) partial sit-up 5) hamstring stretch 6) hip flexor stretch and 7) squatting.
Cat Stretch
Prayer Stretch
Single Knee to Chest
Lumbar Stabilization Exercise[edit | edit source]
Hamstring stretch
Pelvic Tilts in supine lying or standing close to the wall
Specific Exercise Category [12][edit | edit source]
Subjective:
- Symptoms distal to buttocks
Objective:
- Pain centralizes with a specific movement (can be flexion or extension)
Proper Lifting Techniques[edit | edit source]
Squat lift
- Plan The Lift: Know how heavy the object is. Clear a path and know where the object is to be placed.
- Lift Close to the body: This will make the body stronger and more stable. Ensure there is a firm hold on the object and balance it close to the body.
- Feet shoulder width apart: This allows for a solid base of support.
- Bend the knees while keeping the back straight: Avoid any twisting motions.
- Tighten the stomach muscles: This will hold the back in good alignment and prevent excessive force on the spine. Avoid breath holding.
- Lift with the legs: The leg muscles are stronger than the back so use them.
- Avoid straining, get help: Get help if the object is too heavy or it is in an awkward position.
Squat - Remember to:
- Keep back straight
- Knees behind toes
- Keep knees parallel
Golfer’s Lift
- The Golfer’s lift is another lifting technique that is useful for picking something off the floor
- This works best when using something like a chair or table for support when bending
- Kick out the unsupported leg - This helps to keep the back straight
Diagonal Standing
- Stand with one foot slightly in front of the other and distribute the weight evenly between both legs
- This is a preferred position over straight standing
- Avoid putting all of the weight onto one leg while standing.
Aerobic Activity [13][edit | edit source]
Types: Walking, jogging, running, cycling, swimming, climbers, steppers, elliptical machines, ski machines, aerobic dance
Warm up/cool down – low to moderate activity
- 5-10 minutes of warm up (adjust to demands placed on the body)
- 5-10 minutes of cool down (recovery of heart rate and BP)
- 10 minutes of stretching AFTER the warm up OR cool down
ACSM Guidelines:=
- Frequency: 5 days/week
- Duration: 150 minutes per week (minimum)
- Intensity: 40-60% HRmax (HRmax = 220-age)
Benefits of exercise are improved joint health due to low impact exercises, increase bone density due to weight bearing exercises, improving energy, reducing health risks, improving circulation, and reducing stress and improving your mood. Aerobic activity is equally effective at reconditioning muscles as exercise and can also help in decreasing pain, improving your mood, and improving your functional capabilities.[14] Lack of exercise increases your risk of obesity and other co-morbidities increases; this can lead to increased pressure on the spine and decreased flexibility.
Management of Neck Pain?[edit | edit source]
There are specific treatments based on each classification of neck pain: [5]
Cervical Hypomobility[edit | edit source]
- AROM exercises
- Cervical and thoracic mobilization/manipulation isometric or thrust manipulation techniques
- Nonthrust manipulation
Cervical Radiculopathy[edit | edit source]
- Cervical traction (manual/mechanical)
- Upper Limb Tension Tests AROM
- Thoracic spine manipulation
- Postural exercises
Cervical Instability[edit | edit source]
- Postural education
- Cervical stabilization exercise program
- Mobilization/manipulation above and below hypermobilities
- Ergonomic corrections
Acute Pain (Whiplash)[edit | edit source]
- Gentle AROM within patient tolerance
- Activity modification to control pain
- Relative rest
- Physical modalities
- Intermittent use of cervical collar
- Gentle manual therapy and exercises, but avoidance of pain-inducing manual therapy techniques or exercises
Cervicogenic Headache[edit | edit source]
- Cervical and thoracic mobilization/manipulation
- Strengthening neck and postural muscles
- Postural education
Physical Therapy Management of Neck Pain[edit | edit source]
Exercise!
Evidence from the literature says that exercise has a significant effect in reducing chronic non-specific neck pain for short term (<1 month) and intermediate term (1-6 months) [15]
Neck Exercises[edit | edit source]
- OA flexion (chin tuck): A slight nod while keeping your head in neutral
- Flexion with chin tuck: While lying on your back tuck in your chin, lift off until your head clears the table and hold for 3-5 seconds maintaining the chin tuck
- Extension with chin tuck: While laying on your stomach tuck your chin, lift your head off table while maintaining chin tuck and hold 3-5 seconds
- 4-way Isometrics: Lightly press into your hand in flexion, extension, side bending, and rotation
Exercises for Scapular Stabilizers (muscles attached to your shoulder blade)
- Middle Trapezius: With band or lying on stomach, Thumb pointing in the direction exercise is moving, Pinch shoulder blades
- Lower Trapezius: Lying down making a half Y bring your shoulder blade back and down
- Seated Row: Upright Sitting Posture, Pull at elbows, Pinch shoulder blades together
- External Rotation: Elbows at sides, Thumbs pointing out, Shoulders back, Rotate outward
- Scapular Clock: Turn shoulder blade into a clock, Move shoulder blade to each number, retraction and depression are critical, Numbers 9, 8, 7, 6 are important
Stretches[edit | edit source]
Don't forget the thoracic spine![edit | edit source]
A clinical prediction rule was developed to help classify patients with mechanical neck pain that will experience early success from thoracic spine manipulation. Six variables were found: [16]
1. Symptoms < 30 days
2. No symptoms distal to the shoulder
3. Looking up does not aggravate symptoms
4. FABQPA score < 12
5. Diminished upper thoracic spine kyphosis
6. Cervical extension < 30 degrees
If a patient demonstrates 3 of the 6 variables the chance of experiencing a successful outcome improves from 54% to 86%. If a patient has 4 of the 6 variables the chance of a successful outcome rises to 95%.
Resources[edit | edit source]
Chou, MD Lumbar imaging guidelines
APTA Low Back Pain Infographic
Find a PT on the American Physical Therapy Association website
Orthopaedic Section - APTA: Clinical Guidelines for Neck Pain
Orthopaedic Section - APTA: Clinical Guidelines for Low Back Pain
References[edit | edit source]
- ↑ Vos T, Abajobir AA, Abate KH, Abbafati C, Abbas KM, Abd-Allah F, Abdulkader RS, Abdulle AM, Abebo TA, Abera SF, Aboyans V. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet. 2017 Sep 16;390(10100):1211-59.
- ↑ Physicians Plus.Vertebrae. http://www.physiciansplus.net (accessed September 16 2013).
- ↑ 3.0 3.1 Tank P. Grant's Dissector. 15th ed. Little Rock, AR: Wolters Kluwer; 2013.
- ↑ Ahern Family Chiropractic. Seizures. http://ahernfamilychiro.com (accessed September 24 2013).
- ↑ 5.0 5.1 5.2 5.3 5.4 Olson, KA. Manual Physical Therapy of the Spine. St. Louis, MO: Saunders; 2009.
- ↑ Mansfield M, Thacker M, Spahr N, Smith T. Factors associated with physical activity participation in adults with chronic cervical spine pain: a systematic review. PHYSIOTHERAPY [Internet]. [cited 2019 Feb 20];104(1):54–60. Available from: http://ezproxy.aut.ac.nz/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=edswsc&AN=000426458600008&site=eds-live
- ↑ Butler D, Moseley. Explain Pain. Adelaide City Way, SA: Noigroup Publications; 2003.
- ↑ 8.0 8.1 8.2 Neumann, DA. Kinesiology of the Musculoskeletal System: Foundations for Rehabilitation 2nd Edition. St. Louis, MO: Mosby Inc; 2010.
- ↑ Stanton T et al. Evaluation of a Treatment-Based Classification Algorithm for Low Back Pain: A Cross-Sectional Study. Physical Therapy. 2011; 91:496-509.
- ↑ Hicks GE., Fritz JM., Delitto A., McGill SM. Preliminary development of a clinical prediction rule for determining which patients with low back pain will respond to a stabilization exercise program, Arch Phys Med Rehabilitation 2005; 86; 1753-1762
- ↑ Hettinga et al. A systematic review and synthesis of higher quality evidence of the effectiveness of exercise interventions for non-specific low back pain of at least 6 weeks' duration. Physical Therapy Reviews [serial online]. September 2007;12(3):221-232. Available from: CINAHL with Full Text, Ipswich, MA. Accessed October 6, 2013.
- ↑ Browder D, Childs J, Cleland J, Fritz J. Effectiveness of an Extension-Oriented Treatment Approach in a Subgroup of Subjects with Low Back Pain: A Randomized Clinical Trial. Physical Therapy. 2007; 87: 1608-1617.
- ↑ Thompson WR, Gordon NF, Pescatello LS, eds. ACSM's Guidelines for Exercise Testing and Prescription. 8th ed. Baltimore: American College of Sports Medicine; 2010.
- ↑ Hettinga D, Jackson A, Moffett J, May S, Mercer C, Woby S. A systematic review and synthesis of higher quality evidence of the effectiveness of exercise interventions for non-specific low back pain of at least 6 weeks' duration. Physical Therapy Reviews [serial online]. September 2007;12(3):221-232. Available from: CINAHL with Full Text, Ipswich, MA. Accessed October 6, 2013.
- ↑ Bertozzi et. al. Effect of Therapeutic Exercise on Pain and Disability in the Management of Chronic Nonspecific Neck Pain: Systematic Review and Meta-Analysis of Randomized Trials. Phys Ther. 2013; 93:1026-1036
- ↑ Cleland et al. Development of a Clinical Prediction Rule for Guiding Treatment of a Subgroup of Patients with Neck Pain: Use of Thoracic Spine Manipulation, Exercise, and Patient Education. Phys Ther. 2007; 87: 9-23.