Atelectasis: Difference between revisions
Areeba Raja (talk | contribs) No edit summary |
Areeba Raja (talk | contribs) mNo edit summary |
||
| Line 4: | Line 4: | ||
== Introduction == | == Introduction == | ||
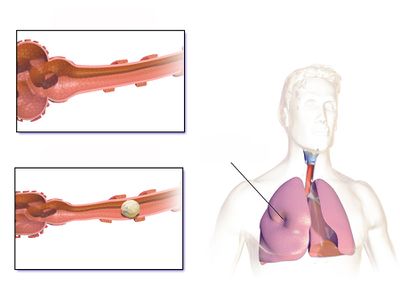
[[File:Atelectasis Normal vs Affected Airway.jpeg|right|frameless|400x400px]] | [[File:Atelectasis Normal vs Affected Airway.jpeg|right|frameless|400x400px]] | ||
Atelectasis describes a state of the collapsed and non-aerated regions of the [[Lung Anatomy|lung]] parenchyma<ref name=":2">Peroni DG, Boner AL. [https://pubmed.ncbi.nlm.nih.gov/12531090/ Atelectasis: mechanisms, diagnosis and management]. Paediatr Respir Rev. 2000;1:274-8.</ref>. It results from the partial or complete, reversible collapse of the small airways leading to an impaired exchange of CO2 and O2 - i.e., intrapulmonary shunt | Atelectasis describes a state of the collapsed and non-aerated regions of the [[Lung Anatomy|lung]] parenchyma<ref name=":2">Peroni DG, Boner AL. [https://pubmed.ncbi.nlm.nih.gov/12531090/ Atelectasis: mechanisms, diagnosis and management]. Paediatr Respir Rev. 2000;1:274-8.</ref>. It results from the partial or complete, reversible collapse of the small airways leading to an impaired exchange of CO2 and O2 - i.e., intrapulmonary shunt.<ref name=":4">Grott K, Dunlap JD. [https://www.ncbi.nlm.nih.gov/books/NBK545316/#!po=10.0000 Atelectasis]. StatPearls [Internet]. 2020 Aug 10.Available from: https://www.ncbi.nlm.nih.gov/books/NBK545316/#!po=10.0000 (accessed 18.4.2021)</ref> | ||
== Epidemiology == | == Epidemiology == | ||
| Line 12: | Line 11: | ||
* There is also no increased incidence of atelectasis in patients with COPD, asthma, or increased age. | * There is also no increased incidence of atelectasis in patients with COPD, asthma, or increased age. | ||
* It is more common in patient's who recently underwent general anesthesia, with the incidence being as high as 90% in this patient population. | * It is more common in patient's who recently underwent general anesthesia, with the incidence being as high as 90% in this patient population. | ||
* It is most commonly seen in the [[Post-Operative Pulmonary Complication|post-operative]] patients whose breathing mechanism is impacted by the procedure, [[Pain Mechanisms|pain]], and prolonged recumbency. | |||
* | * Less commonly, atelectasis is seen in people with conditions signify chronic sputum production or airway obstruction, such as [[COPD (Chronic Obstructive Pulmonary Disease)|COPD]], [[bronchiectasis]], and [[Cystic Fibrosis|cystic fibrosis]]. | ||
* Obese and/or pregnant patients are more likely to develop atelectasis due to cephalad displacement of the diaphragm<ref name=":4" /> | * Obese and/or pregnant patients are more likely to develop atelectasis due to cephalad displacement of the diaphragm<ref name=":4" /> | ||
== | == Classification == | ||
It can be classified as follows<ref name=":5">Stark P. [http://publishingimages.s3.amazonaws.com/eZineImages/PracticePerfect/715/Atelectasis-Types-and-pathogenesis-in-adults-UpToDate.pdf Atelectasis: Types and pathogenesis in adults] [Internet]. 2020. </ref> | |||
1. pathophysiologic mechanism (e.g., compressive atelectasis) | |||
2. the amount of lung involved (e.g., lobar, segmental, or sub segmental atelectasis) | |||
3. the location (i.e., specific lobe or segment location). | |||
=== On the basis of pathophysiology === | |||
Following table comprises the classification of atelectasis based on pathophysiologic mechanism<ref name=":2" /><ref name=":4" /><ref name=":5" /><ref>Raman TS, Mathew S, Garcha PS. [https://pubmed.ncbi.nlm.nih.gov/10216624/ Atelectasis in children.] Indian pediatrics. 1998 May;35(5):429-35.</ref><ref>Culiner MM. [https://pubmed.ncbi.nlm.nih.gov/5947916/ The right middle lobe syndrome, a non-obstructive complex.] Diseases of the Chest. 1966; 50(1):57-66.</ref><ref>Sutnick AI, Soloff LA. [https://pubmed.ncbi.nlm.nih.gov/14104855/ Atelectasis with pneumonia: a pathophysiologic study.] Annals of internal medicine. 1964;60:39-46.</ref><ref>Magnusson L, Spahn DR. "[https://pubmed.ncbi.nlm.nih.gov/12821566/ New concepts of atelectasis during general anaesthesia.]" BR J Anaesth. 2003;91.1: 61-72.</ref><ref>Woodring J H, & Reed JC . [https://pubmed.ncbi.nlm.nih.gov/8820021/ Types and mechanisms of pulmonary atelectasis]. J Thorac Imag 1996;11:92-108''.''</ref><ref>Nazir A Lone, MD, MBBS, MPH, FACP, FCCP. [https://emedicine.medscape.com/article/1001160-clinical#showall Pulmonary Atelectasis Clinical Presentation: History, Physical, Causes] [Internet]. Medscape.com. Medscape; 2020 [cited 2021 Nov 19]. </ref><ref>Duggan M, Kavanagh Brian P, Warltier David C. [https://watermark.silverchair.com/0000542-200504000-00021.pdf?token=AQECAHi208BE49Ooan9kkhW_Ercy7Dm3ZL_9Cf3qfKAc485ysgAAAvkwggL1BgkqhkiG9w0BBwagggLmMIIC4gIBADCCAtsGCSqGSIb3DQEHATAeBglghkgBZQMEAS4wEQQM1M0kQp1WSf9k3E1pAgEQgIICrLMn-sN1G756LQkSnJ_jRLF23z5xUtHzyRTvKKqa6S2JY74yR68UsnLh8BNiq5XazGaZmYCwX6jMqwhqGyXljP8w9iRmCqNG3VAPCNodaTv3AZ5C3WwjFWriShxwo2TGcwzS-OZ3peld3sILyDNKQbB_6uqtsYSKhOFpvx9EPgG030EMF5Dy3_frh4odd-wqYniZRDycQTGWXI2fafXX6b3bnOyxguU6PHdRpk2vz6278whwwmYxqVo9qHmM0N1xCMiU4ug-ZSvqbKDzLX-ogkLQnglLya866_RflkevOGtSMVTyTKY7DH15zsIUQwHI2idz3hV1r8C64XLsgV8QmoRJ7XAZ8RLGtjmfHEBq07iieihFK2y22aUH4JMzbk1ocI-xI0k5yFDJylttJ2xZK-AzaZlgdUENRb1z_Oeb-ZwCH2dhdZmbSsoxgnn1kF5uKQOhEQHuyU93f91F9F_Nn2G7BR4EV6zRSGKj1RJQz76TUMwX8uF5VogWIu2ifSLEqP15sRuioXrJ5S30L7nEd9BO-WDuNsrITy8Q-NlOKaQgcgi2Souw6eNgAW9E_CabAoaOohLFhJViafBXNCJklI1xCW5oefxrJvZmagpMfCfbK3GOd5kBAyhGvsHEWZf5JKsODwgYUhO1yyy9IZQABb0kPrQY7EFOaqaqPCxh05GTpc2MLqZmtVXIoPRaxcLNAhV3Ftbhau8sQ48Z0uHBNbErgIBG_lhnnwb4yadf950l9UWb55kyJZOUFP_zXkuBknMkCoDl8I2XLkcr7tIVo4fX_Nxa15wRKjFbzyoUF8BMzOQRrBsYdcwS9-rLE7T1xCrrUgqZVQ_S2jOW_U4EfeALlCJz_YBOxa7gIzoDfAX6zOHPoxJHQb5bEEbij3GcBdM1X-IDIl5l7np8wA Pulmonary Atelectasis. Anesthesiology] [Internet]. 2005 Apr 1 [cited 2021 Nov 19];102(4):838–54.</ref><ref>Priftis KN, Rubin B. [https://www.semanticscholar.org/paper/Atelectasis%2C-Middle-Lobe-Syndrome-and-Plastic-Priftis-Rubin/7f3852fc6ba113a1c95e1d7166ff58e02dda16c3 Atelectasis, Middle Lobe Syndrome and Plastic Bronchitis]. Paediatric Bronchoscopy [Internet]. 2010 [cited 2021 Nov 20];149–55. </ref><ref name=":6">Ray K, Bodenham A, Paramasivam E. [https://watermark.silverchair.com/mkt064.pdf?token=AQECAHi208BE49Ooan9kkhW_Ercy7Dm3ZL_9Cf3qfKAc485ysgAAAsgwggLEBgkqhkiG9w0BBwagggK1MIICsQIBADCCAqoGCSqGSIb3DQEHATAeBglghkgBZQMEAS4wEQQM6sUz4wOAKvLg7PbLAgEQgIICewEV0T1o9_DHIcoWCsmVEIfcOQyXRIBHru78h1ENbk1onzvDrHSaG_5k0flU4ewkzrK8YCpFTMiVBK4XYTrJEXhy07LgeAOG_-0Tz4L59ygf-48ZT-LmB1SclpqKKuzMoscfc136qKONmokL8UXUV4OIbqNvXleepZh84cpdOUz6K5WjGTmfeqNM4SHbQ7sDYUtczDVXtcP90x_oG2UuliCdOSHZx9bO6jtzy2ktVWIuObqQ-WOU20Tv-yhEKZnjMS_kqR1-TQWaGYYS8eCo8kmDutZ2RGnLTEwgVQOxBZz9B74WsVZ95f7gh89FRD7CwOf06zNZxcpZCgSZzq4YMV4no5tK1b1mGkZdMW14FBOd9MLbcaJklbtqGlkikp_EdRjWRSONBUGPbKT6WoLvqqSMmiRh3U0QcqNkTSznJKA-48UKmI8NUCLPkdhsRzJSljTMSO9KKnIzBM4nBc0N47FJr-OUA7BzU89l0Fucn5R7VeXNC6CQEJEPK8NAhkjoAUhU_UR0c8YCxX0KGXp8w-FyGkxt2ItCADar39MZh7Q94n2Ir6PlZx6VfrHeaOoxgTESar8m2KLedJiVYgvQi916-YcJpOjrdDFisgij4wUshEJ3fvgZRZKCBt_Dgctg_IRKmu6Jl4-4_YxSPqJsxmeRF_90DhMHz89RuDr2rd_M6Ki8zXejxqZX_Yw0hfYSs9YWhNCzmvQCmOTNKRS27Dc0kvgTIR2BOjTIEJ1XMFW-2ck5y0--WBYJ89LAvo10_rI9HcsrTLFzp3RjOZII0TFl31RamZw-InFWGLw6pp-shqscXvQ7fIFBZLvfQAuB-PSn1QLDAQawjfKY Pulmonary atelectasis in anaesthesia and critical care.] Continuing Education in Anaesthesia Critical Care & Pain [Internet]. 2014 Oct [cited 2021 Nov 19];14(5):236–45. </ref><ref>Domino KB. [https://watermark.silverchair.com/20191000_0-00012.pdf?token=AQECAHi208BE49Ooan9kkhW_Ercy7Dm3ZL_9Cf3qfKAc485ysgAAAucwggLjBgkqhkiG9w0BBwagggLUMIIC0AIBADCCAskGCSqGSIb3DQEHATAeBglghkgBZQMEAS4wEQQMxYo4pkl59eKRPec3AgEQgIICmnv-XL-UKZ_D6uk8clbSqJAlFrh4vk2w2BuKeobo1Ng230DAe5scvejktVy0eBEsTX7F2SEyCxulihfxY9rz1UnuccPznOO9fBYCS_C5tcdbMZrgUWkO2YFRhlxSWFAGjj8XyR4VpDYUjQvqfj6mI99wQtGhFS0CTq2pMLF9xIAXwicIqAve6xnXzS3W2mynrcvlc3jQjWJ5r0g4OO_tVSVDlNPwS_3wddv0kpYU-3KfPgABC_toy4iszzDTqepWt9RA3e5W8GDQKI3pYpTG36IwBBROKE6falj64kvO_51QM9OyMjh0zruZlxYpD8i4SrcBabJqChJ4quLWjoqn3GuQfrWz0IVcnVPSQqmWM-UJRdEwB5Ll7eaNQ3vRUke8nuc7zgOfErwmHfikUsBCKCIjKMaVpUnMmXHbN_01vfVxKOfkIYZoOvvmFB8a6Rdiow7xLyuz__wMqmjKrpfg6-svS7id6_ei-5vEA--NKpbV3Jm8_h-sQQvv0kbWq2WEBDc5e2kGgv-1_jtqxcqTQ6iZANE_HzL413E10pfDIGpgjGDYF_WyLP3rgPohgWzg6l_mFqDN8LMqZzSp2DgmCljEdG51RSCmXdotJgNz8Dazl9NTX5Ai6YgMLOpIBjwcfzAkcvY3lhAS3TLqVVRdew11iXJDJMYAZAjznZE3idCZI4iRUwXTKVID3JxOcF95BRV9zE8DDKJBGjWLlAqqttae_hROsZSdYMil2qhzutMs35K4sjKoGaYxKDgJWTdEYvWBoI58UqPlFos2RHDEgUEIjowRCHf6UtQACovkZJmMldkoGyKFTD64leG4Eg4Jrr0Qta85vTu-Mh7l-KQFiRH7MHoQpgWwlhxtjKiLzPF8Va-oItrjSirgSQ Pre-emergence Oxygenation and Postoperative Atelectasis.] Anesthesiology [Internet]. 2019 Oct 1 [cited 2021 Nov 20];131(4):771–3. </ref><ref>Kavanagh BP. [https://www.minervamedica.it/en/getfreepdf/TnpVang3bXVBU1JPeVdsTU1BY3Y0V3pMblJrS2VZZFE4UjBNd3JJZW0rY09xclZ3bFhzdnBsdmptWjdpRzFZUA%253D%253D/R02Y2008N06A0285.pdf Perioperative atelectasis.] Minerva anestesiologica [Internet]. 2021 [cited 2021 Nov 19];74(6).</ref><ref name=":7">Restrepo RD, Braverman J. [https://www.tandfonline.com/doi/pdf/10.1586/17476348.2015.996134?needAccess=true Current challenges in the recognition, prevention and treatment of perioperative pulmonary atelectasis.] Expert Review of Respiratory Medicine [Internet]. 2014 Dec 26 [cited 2021 Nov 19];9(1):97–107. </ref><ref>Johnston C, Carvalho WB de. [https://pubmed.ncbi.nlm.nih.gov/18989568/ Atelectasias em pediatria: mecanismos, diagnóstico e tratamento. Revista da Associação Médica Brasileira] [Internet]. 2008 Oct [cited 2021 Nov 19];54(5). </ref><ref>Atağ E. [https://jag.journalagent.com/hnhjournal/pdfs/HNHJ_61_2_139_144.pdf Etiology, diagnosis and treatment in childhood atelectasis.] Haydarpasa Numune Training and Research Hospital Medical Journal [Internet]. 2020 [cited 2021 Nov 19]; Available from: <nowiki>https://jag.journalagent.com/hnhjournal/pdfs/HNHJ_61_2_139_144.pdf</nowiki></ref><ref>Navas-Blanco JR, Dudaryk R. [https://link.springer.com/content/pdf/10.1186/s12871-020-01095-7.pdf Management of Respiratory Distress Syndrome due to COVID-19 infection.] BMC Anesthesiology [Internet]. 2020 Jul 20 [cited 2021 Nov 20];20(1). </ref> | |||
{| class="wikitable" | |||
|+ | |||
!Pathophysiologic Mechanism | |||
!Pathogenesis | |||
!Associated Types of Atelectasis | |||
!Cause | |||
|- | |||
|Compression of Lung Tissue | |||
|This mechanism of atelectasis occurs through compression. This means that the net balance of forces across an alveolar wall shifts toward ensuring its collapse. | |||
| | |||
* Passive Atelectasis | |||
* Compressive Atelectasis | |||
| | |||
* [[Airway Stenosis]] | |||
* Inflammation and edema caused by aspiration or inhalation injury (smoke, chemical agents) | |||
* [[Edema Assessment|Edema]] of the airway | |||
* Bronchial tumor | |||
* Granuloma | |||
* Papilloma | |||
* Cardiomegaly | |||
* Lobar [[Emphysema]] | |||
* Vascular ring (innominate artery) | |||
* Lymph node hypertrophy (tuberculosis) | |||
* Tumors (mediastinum) | |||
* Chylothorax | |||
* [[Hemothorax]] | |||
* [[Pneumothorax]] | |||
* General anesthesia | |||
|- | |||
|Absorption of Alveolar Air | |||
|A second major reason is gas resorption. This may occur in two ways. | |||
* If airway occlusion is complete, alveolar gas can exit from the alveolar units only through the blood stream. Thus, atelectasis can develop in the face of obstruction. | |||
* The second and perhaps more important mechanism of gas resorption may occur in areas that are poorly ventilated and well perfused. If the inspired oxygen concentration increases, the alveolar oxygen, but not nitrogen, uptake will be high; thus, there is less alveolar splinting and a loss of lung volume. | |||
| | |||
* Obstructive Atelectasis | |||
* Cicatrizion Atelectasis | |||
| | |||
* Foreign Body Aspiration | |||
* Secretion Plugs | |||
* [[Cystic Fibrosis]] | |||
* Ciliary Dyskinesia Syndrome | |||
* C | |||
* [[Asthma]] | |||
* [[Bronchiolitis]] | |||
* Bronchospasm | |||
* Histoplasmosis | |||
* General Anesthesia | |||
|- | |||
|Impairment of Surfactant Function | |||
|Insufficient surfactant function can result from deficiency of acquired dysfunction (e . g ., as for premature neonates), and this occurs in the context of lung injury. Once inactivated, increased local surface tension results in decreased expansion; on a global level, this produces a reduction of resting lung volume. | |||
| | |||
* Adhesive atelectasis | |||
| | |||
* Hyaline Membrane Disease | |||
* [[Coronavirus Disease (COVID-19)|COVID-19]] | |||
* [[Acute Respiratory Distress Syndrome (ARDS)]] | |||
* [[Pneumonia]] | |||
* Pulmonary Edema | |||
* Almost Drowning | |||
* General Anesthesia | |||
|} | |||
{{#ev:youtube|watch?v=gjLCu8qe2nI&ab_channel=NinjaNerdLectures}} | |||
Atelectasis can be | === On the basis of location === | ||
Atelectasis can be classified on the basis of location according to radiological patterns of collapse<ref name=":6" /> | |||
==== Complete collapse ==== | |||
Collapse of an entire lung leads to complete opacification of a hemithorax (a so-called ‘white out’). This is often confused with a large [[Pleural Effusion|pleural effusion]], but can be distinguished by the presence of mediastinal shift towards a collapsed lung compared with movement away from a pleural effusion. | |||
This | |||
==== Lobar collapse ==== | |||
Characteristic features associated with individual lobar collapse are as follows: | |||
* Right upper lobe (RUL) collapse | |||
* | * Right middle lobe (RML) collapse | ||
* Right lower lobe (RLL) collapse | |||
* Left upper lobe (LUL) collapse | |||
* Left Lower Lobe (LLL) collapse | |||
== Clinical Implications == | |||
Following are the clinical implications of atelectasis <ref name=":7" /><ref>Zeng C, Lagier D, Lee J-W, Vidal Melo MF. [https://pubs.asahq.org/anesthesiology/article-abstract/doi/10.1097/ALN.0000000000003943/117098/Perioperative-Pulmonary-Atelectasis-Part-I-Biology?redirectedFrom=fulltext Perioperative Pulmonary Atelectasis: Part I. Biology and Mechanisms.] Anesthesiology [Internet]. 2021 Sep 8 [cited 2021 Nov 19]; </ref> | |||
* Decreased lung compliance | |||
* [[Hypoxaemia|Hypoxemia]] | |||
* Increased pulmonary vascular resistance (PVR) | |||
* Inflammation as a local tissue biologic response | |||
* Local immune dysfunction | |||
* Damage of the alveolar capillary barrier | |||
* Potential loss of lung fluid clearance | |||
* Increased lung protein permeability | |||
* Susceptibility to infection | |||
* Impaired penetration of antibiotics into lung tissue | |||
* Factors that can initiate or exaggerate lung injury | |||
* Acute respiratory failure. | |||
== Clinical Presentation == | == Clinical Presentation == | ||
| Line 55: | Line 140: | ||
* Hypoxia/[[Hypoxaemia|hypoxemia]] | * Hypoxia/[[Hypoxaemia|hypoxemia]] | ||
* [[ | === Diagnosis === | ||
*[[Chest X-Rays|Chest X-ray]]<ref name=":4" /><ref>Khan AN, Al-Jahdali H, AL-Ghanem S, Gouda A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714572/pdf/ATM-04-149.pdf Reading chest radiographs in the critically ill (Part II): Radiography of lung pathologies common in the ICU patient.] Annals of Thoracic Medicine [Internet]. 2009;4(3):149–57. </ref> | |||
* Bronchoscopy<ref name=":8">Woodring J. [https://www.ajronline.org/doi/pdfplus/10.2214/ajr.150.4.757 Determining the cause of pulmonary atelectasis: a comparison of plain radiography and CT.] American Journal of Roentgenology. 1988 Apr;150(4):757–63.</ref> | |||
* [[CT Scans|CT Scan]]<ref name=":8" /> | |||
* [[Ultrasound Scans|Ultrasound]]<ref>Lichtenstein D, Meziere G. [https://www.researchgate.net/publication/287527270_Ultrasound_diagnosis_of_atelectasis Ultrasound diagnosis of atelectasis] [Internet]. ResearchGate. unknown; 2005 [cited 2021 Nov 20]. </ref><ref>Liu J, Chen S-W, Liu F, Li Q-P, Kong X-Y, Feng Z-C. [https://pubmed.ncbi.nlm.nih.gov/25341049/ The Diagnosis of Neonatal Pulmonary Atelectasis Using Lung Ultrasonography.] Chest [Internet]. 2015 Apr [cited 2021 Nov 20];147(4):1013–9. </ref><ref>Acosta CM, Maidana GA, Jacovitti D, Belaunzarán A, Cereceda S, Rae E, et al. [https://pubs.asahq.org/anesthesiology/article/120/6/1370/11911/Accuracy-of-Transthoracic-Lung-Ultrasound-for Accuracy of Transthoracic Lung Ultrasound for Diagnosing Anesthesia-induced Atelectasis in Children.] Anesthesiology [Internet]. 2014 Jun 1 [cited 2021 Nov 20];120(6):1370–9. </ref> | |||
{{#ev:youtube|watch?v=OcIxL56an3c}} | {{#ev:youtube|watch?v=OcIxL56an3c}} | ||
| Line 66: | Line 155: | ||
* Prophylactic measures, such as [[Incentive Spirometry|incentive spirometry]], should be taught and instituted before surgery and continued on an hourly basis following surgery until discharge to obtain the maximal benefit<ref name=":4" />. | * Prophylactic measures, such as [[Incentive Spirometry|incentive spirometry]], should be taught and instituted before surgery and continued on an hourly basis following surgery until discharge to obtain the maximal benefit<ref name=":4" />. | ||
[[File:Le-minh-phuong-niH7Z81S44g-unsplash.jpg|right|frameless|361x361px]] | [[File:Le-minh-phuong-niH7Z81S44g-unsplash.jpg|right|frameless|361x361px]] | ||
'''[[Respiratory Physiotherapy|Airway clearance techniques]]''' | |||
=== '''[[Respiratory Physiotherapy|Airway clearance techniques]]''' === | |||
As atelectasis can be caused by blockage of bigger airways, physiotherapy treatment to assist in airway clearance can improve atelectasis. Examples of airway clearance technique include: | |||
'''Breathing exercises:''' | * [[Active Cycle of Breathing Technique|Active cycle breathing techniques]]<ref name=":0">Stiller K, Geake T, Taylor J, Grant R, Hall B. [https://pubmed.ncbi.nlm.nih.gov/2245671/ Acute lobar atelectasis: a comparison of two chest physiotherapy regimens.] Chest. 1990 Dec 1;98(6):1336-40.</ref><ref name=":1">Schindler MB. [https://pubmed.ncbi.nlm.nih.gov/16137380/ Treatment of atelectasis: where is the evidence?.] Critical Care. 2005 Aug;9(4):341.</ref> | ||
* Supported cough<ref name=":1" /> | |||
* Positioning<ref name=":0" /> | |||
* Postural drainage<ref name=":0" /> | |||
=== '''Breathing exercises:''' === | |||
* [[Incentive Spirometry|Incentive spirometry]] can be useful for treating or preventing atelectasis in post-operative patients, it gives visual feedback to the patient on how he is performing. Consists of a deep and slow maximal inspiration, through the mouth, followed by a post-inspiratory pause and exhalation up to functional residual capacity<ref name=":3" />. | * [[Incentive Spirometry|Incentive spirometry]] can be useful for treating or preventing atelectasis in post-operative patients, it gives visual feedback to the patient on how he is performing. Consists of a deep and slow maximal inspiration, through the mouth, followed by a post-inspiratory pause and exhalation up to functional residual capacity<ref name=":3" />. | ||
* Sustained maximal inspiration (SMI): is the same as incentive spirometry but it does not require material <ref name=":3" />. SMI is often used to prevent and manage atelectasis in abdominal and thoracic surgery patients.<ref>Tan AK. [https://pubmed.ncbi.nlm.nih.gov/8537988/ Incentive spirometry for tracheostomy and laryngectomy patients]. The Journal of otolaryngology. 1995 Oct;24(5):292-4.</ref> Its effects are often compared with incentive spirometry, and interestingly evidence has shown similar effects in SMI in improving breathing patterns, chest expansion, and thoracoabdominal asynchrony.<ref name=":3">Mendes LP, Teixeira LS, da Cruz LJ, Vieira DS, Parreira VF. [https://pubmed.ncbi.nlm.nih.gov/30654164/ Sustained maximal inspiration has similar effects compared to incentive spirometers]. Respiratory physiology & neurobiology. 2019 Mar 1;261:67-74. | * Sustained maximal inspiration (SMI): is the same as incentive spirometry but it does not require material <ref name=":3" />. SMI is often used to prevent and manage atelectasis in abdominal and thoracic surgery patients.<ref>Tan AK. [https://pubmed.ncbi.nlm.nih.gov/8537988/ Incentive spirometry for tracheostomy and laryngectomy patients]. The Journal of otolaryngology. 1995 Oct;24(5):292-4.</ref> Its effects are often compared with incentive spirometry, and interestingly evidence has shown similar effects in SMI in improving breathing patterns, chest expansion, and thoracoabdominal asynchrony.<ref name=":3">Mendes LP, Teixeira LS, da Cruz LJ, Vieira DS, Parreira VF. [https://pubmed.ncbi.nlm.nih.gov/30654164/ Sustained maximal inspiration has similar effects compared to incentive spirometers]. Respiratory physiology & neurobiology. 2019 Mar 1;261:67-74. | ||
| Line 75: | Line 169: | ||
{{#ev:youtube|watch?v=-O-Zawtb32o&feature=emb_logo&ab_channel=MyDoctor-KaiserPermanente}} | {{#ev:youtube|watch?v=-O-Zawtb32o&feature=emb_logo&ab_channel=MyDoctor-KaiserPermanente}} | ||
'''Early mobilization<ref name=":0" />'''<ref>Possa SS, Amador CB, Costa AM, Sakamoto ET, Kondo CS, Vasconcellos AM, et al. I[https://pubmed.ncbi.nlm.nih.gov/24290563/ mplementation of a guideline for physical therapy in the postoperative period of upper abdominal surgery reduces the incidence of atelectasis and length of hospital stay.] Rev Port Neumol 2014;20(2): 69-77.</ref><ref>Moradian ST, Najafloo M, Mahmoudi H, Ghiasi MS. [https://pubmed.ncbi.nlm.nih.gov/28838589/ Early mobilization reduces the atelectasis and pleural effusion in patients undergoing coronary artery bypass graft surgery: A randomized clinical trial]. J Vasc Nurs 2017;35(3):141–145. </ref> | === '''Early mobilization<ref name=":0" />'''<ref>Possa SS, Amador CB, Costa AM, Sakamoto ET, Kondo CS, Vasconcellos AM, et al. I[https://pubmed.ncbi.nlm.nih.gov/24290563/ mplementation of a guideline for physical therapy in the postoperative period of upper abdominal surgery reduces the incidence of atelectasis and length of hospital stay.] Rev Port Neumol 2014;20(2): 69-77.</ref><ref>Moradian ST, Najafloo M, Mahmoudi H, Ghiasi MS. [https://pubmed.ncbi.nlm.nih.gov/28838589/ Early mobilization reduces the atelectasis and pleural effusion in patients undergoing coronary artery bypass graft surgery: A randomized clinical trial]. J Vasc Nurs 2017;35(3):141–145. </ref> === | ||
This fits in the picture of both post-operative patients and populations with acute respiratory conditions, such as acute [[pneumonia]]. When a patient is medically stable enough, the physiotherapist should assist with mobilization in accordance with the patient's status. Early mobilization, includes sitting position and ambulation either with/without aids (onset <48h after surgery). It is believed that early mobilization results in increased lung volume, preventing therefore of atelectasis. | This fits in the picture of both post-operative patients and populations with acute respiratory conditions, such as acute [[pneumonia]]. When a patient is medically stable enough, the physiotherapist should assist with mobilization in accordance with the patient's status. Early mobilization, includes sitting position and ambulation either with/without aids (onset <48h after surgery). It is believed that early mobilization results in increased lung volume, preventing therefore of atelectasis. | ||
Revision as of 15:30, 20 November 2021
Introduction[edit | edit source]
Atelectasis describes a state of the collapsed and non-aerated regions of the lung parenchyma[1]. It results from the partial or complete, reversible collapse of the small airways leading to an impaired exchange of CO2 and O2 - i.e., intrapulmonary shunt.[2]
Epidemiology[edit | edit source]
- Atelectasis does not preferentially affect either sex.
- There is also no increased incidence of atelectasis in patients with COPD, asthma, or increased age.
- It is more common in patient's who recently underwent general anesthesia, with the incidence being as high as 90% in this patient population.
- It is most commonly seen in the post-operative patients whose breathing mechanism is impacted by the procedure, pain, and prolonged recumbency.
- Less commonly, atelectasis is seen in people with conditions signify chronic sputum production or airway obstruction, such as COPD, bronchiectasis, and cystic fibrosis.
- Obese and/or pregnant patients are more likely to develop atelectasis due to cephalad displacement of the diaphragm[2]
Classification[edit | edit source]
It can be classified as follows[3]
1. pathophysiologic mechanism (e.g., compressive atelectasis)
2. the amount of lung involved (e.g., lobar, segmental, or sub segmental atelectasis)
3. the location (i.e., specific lobe or segment location).
On the basis of pathophysiology[edit | edit source]
Following table comprises the classification of atelectasis based on pathophysiologic mechanism[1][2][3][4][5][6][7][8][9][10][11][12][13][14][15][16][17][18]
| Pathophysiologic Mechanism | Pathogenesis | Associated Types of Atelectasis | Cause |
|---|---|---|---|
| Compression of Lung Tissue | This mechanism of atelectasis occurs through compression. This means that the net balance of forces across an alveolar wall shifts toward ensuring its collapse. |
|
|
| Absorption of Alveolar Air | A second major reason is gas resorption. This may occur in two ways.
|
|
|
| Impairment of Surfactant Function | Insufficient surfactant function can result from deficiency of acquired dysfunction (e . g ., as for premature neonates), and this occurs in the context of lung injury. Once inactivated, increased local surface tension results in decreased expansion; on a global level, this produces a reduction of resting lung volume. |
|
|
On the basis of location[edit | edit source]
Atelectasis can be classified on the basis of location according to radiological patterns of collapse[12]
Complete collapse[edit | edit source]
Collapse of an entire lung leads to complete opacification of a hemithorax (a so-called ‘white out’). This is often confused with a large pleural effusion, but can be distinguished by the presence of mediastinal shift towards a collapsed lung compared with movement away from a pleural effusion.
Lobar collapse[edit | edit source]
Characteristic features associated with individual lobar collapse are as follows:
- Right upper lobe (RUL) collapse
- Right middle lobe (RML) collapse
- Right lower lobe (RLL) collapse
- Left upper lobe (LUL) collapse
- Left Lower Lobe (LLL) collapse
Clinical Implications[edit | edit source]
Following are the clinical implications of atelectasis [15][19]
- Decreased lung compliance
- Hypoxemia
- Increased pulmonary vascular resistance (PVR)
- Inflammation as a local tissue biologic response
- Local immune dysfunction
- Damage of the alveolar capillary barrier
- Potential loss of lung fluid clearance
- Increased lung protein permeability
- Susceptibility to infection
- Impaired penetration of antibiotics into lung tissue
- Factors that can initiate or exaggerate lung injury
- Acute respiratory failure.
Clinical Presentation[edit | edit source]
The signs and symptoms of atelectasis are often non-specific:[1][20]
- Chest pain
- Shallow breathing pattern
- Reduced chest expansion
- Increased respiratory rate
- Increased work of breathing
- Reduced breath sound on the ipsilateral side of auscultation. In cases of the upper lobe atelectasis, bronchial sounds may be heard, because of the proximity to the major airways.
- Hypoxia/hypoxemia
Diagnosis[edit | edit source]
- Chest X-ray[2][21]
- Bronchoscopy[22]
- CT Scan[22]
- Ultrasound[23][24][25]
Physiotherapy[edit | edit source]
Most atelectasis that appears during general anesthesia leads to transient lung dysfunction that resolves within 24 hours after surgery. Nevertheless, some patients develop significant perioperative respiratory complications that can lead to increased morbidity and mortality if not treated.
- Atelectasis is preventable through avoidance of general anesthesia, early mobilization, adequate pain control, and minimizing parenteral opioid administration.
- Changing position from supine to upright increases FRC and decreases atelectasis.
- Encouraging patients to take deep breaths, early ambulation, incentive spirometry, use of Positive Expiratory Pressure (PEP) Device, chest physiotherapy, tracheal suctioning (in intubated patients), and/or positive pressure ventilation has been shown to decrease atelectasis.
- Prophylactic measures, such as incentive spirometry, should be taught and instituted before surgery and continued on an hourly basis following surgery until discharge to obtain the maximal benefit[2].
Airway clearance techniques[edit | edit source]
As atelectasis can be caused by blockage of bigger airways, physiotherapy treatment to assist in airway clearance can improve atelectasis. Examples of airway clearance technique include:
Breathing exercises:[edit | edit source]
- Incentive spirometry can be useful for treating or preventing atelectasis in post-operative patients, it gives visual feedback to the patient on how he is performing. Consists of a deep and slow maximal inspiration, through the mouth, followed by a post-inspiratory pause and exhalation up to functional residual capacity[28].
- Sustained maximal inspiration (SMI): is the same as incentive spirometry but it does not require material [28]. SMI is often used to prevent and manage atelectasis in abdominal and thoracic surgery patients.[29] Its effects are often compared with incentive spirometry, and interestingly evidence has shown similar effects in SMI in improving breathing patterns, chest expansion, and thoracoabdominal asynchrony.[28] Hence, it could be an alternative where incentive spirometry is unavailable.
Early mobilization[26][30][31][edit | edit source]
This fits in the picture of both post-operative patients and populations with acute respiratory conditions, such as acute pneumonia. When a patient is medically stable enough, the physiotherapist should assist with mobilization in accordance with the patient's status. Early mobilization, includes sitting position and ambulation either with/without aids (onset <48h after surgery). It is believed that early mobilization results in increased lung volume, preventing therefore of atelectasis.
Complications[edit | edit source]
Atelectasis is one of the most common respiratory complications in the perioperative period, and it may contribute to significant morbidity and mortality, including the development of pneumonia and acute respiratory failure. Prevention of atelectasis is vital to improving patient outcomes in the postoperative period. Despite employing these strategies, atelectasis is not always preventable and, therefore, early recognition and treatment are equally important.[2]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Peroni DG, Boner AL. Atelectasis: mechanisms, diagnosis and management. Paediatr Respir Rev. 2000;1:274-8.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Grott K, Dunlap JD. Atelectasis. StatPearls [Internet]. 2020 Aug 10.Available from: https://www.ncbi.nlm.nih.gov/books/NBK545316/#!po=10.0000 (accessed 18.4.2021)
- ↑ 3.0 3.1 Stark P. Atelectasis: Types and pathogenesis in adults [Internet]. 2020.
- ↑ Raman TS, Mathew S, Garcha PS. Atelectasis in children. Indian pediatrics. 1998 May;35(5):429-35.
- ↑ Culiner MM. The right middle lobe syndrome, a non-obstructive complex. Diseases of the Chest. 1966; 50(1):57-66.
- ↑ Sutnick AI, Soloff LA. Atelectasis with pneumonia: a pathophysiologic study. Annals of internal medicine. 1964;60:39-46.
- ↑ Magnusson L, Spahn DR. "New concepts of atelectasis during general anaesthesia." BR J Anaesth. 2003;91.1: 61-72.
- ↑ Woodring J H, & Reed JC . Types and mechanisms of pulmonary atelectasis. J Thorac Imag 1996;11:92-108.
- ↑ Nazir A Lone, MD, MBBS, MPH, FACP, FCCP. Pulmonary Atelectasis Clinical Presentation: History, Physical, Causes [Internet]. Medscape.com. Medscape; 2020 [cited 2021 Nov 19].
- ↑ Duggan M, Kavanagh Brian P, Warltier David C. Pulmonary Atelectasis. Anesthesiology [Internet]. 2005 Apr 1 [cited 2021 Nov 19];102(4):838–54.
- ↑ Priftis KN, Rubin B. Atelectasis, Middle Lobe Syndrome and Plastic Bronchitis. Paediatric Bronchoscopy [Internet]. 2010 [cited 2021 Nov 20];149–55.
- ↑ 12.0 12.1 Ray K, Bodenham A, Paramasivam E. Pulmonary atelectasis in anaesthesia and critical care. Continuing Education in Anaesthesia Critical Care & Pain [Internet]. 2014 Oct [cited 2021 Nov 19];14(5):236–45.
- ↑ Domino KB. Pre-emergence Oxygenation and Postoperative Atelectasis. Anesthesiology [Internet]. 2019 Oct 1 [cited 2021 Nov 20];131(4):771–3.
- ↑ Kavanagh BP. Perioperative atelectasis. Minerva anestesiologica [Internet]. 2021 [cited 2021 Nov 19];74(6).
- ↑ 15.0 15.1 Restrepo RD, Braverman J. Current challenges in the recognition, prevention and treatment of perioperative pulmonary atelectasis. Expert Review of Respiratory Medicine [Internet]. 2014 Dec 26 [cited 2021 Nov 19];9(1):97–107.
- ↑ Johnston C, Carvalho WB de. Atelectasias em pediatria: mecanismos, diagnóstico e tratamento. Revista da Associação Médica Brasileira [Internet]. 2008 Oct [cited 2021 Nov 19];54(5).
- ↑ Atağ E. Etiology, diagnosis and treatment in childhood atelectasis. Haydarpasa Numune Training and Research Hospital Medical Journal [Internet]. 2020 [cited 2021 Nov 19]; Available from: https://jag.journalagent.com/hnhjournal/pdfs/HNHJ_61_2_139_144.pdf
- ↑ Navas-Blanco JR, Dudaryk R. Management of Respiratory Distress Syndrome due to COVID-19 infection. BMC Anesthesiology [Internet]. 2020 Jul 20 [cited 2021 Nov 20];20(1).
- ↑ Zeng C, Lagier D, Lee J-W, Vidal Melo MF. Perioperative Pulmonary Atelectasis: Part I. Biology and Mechanisms. Anesthesiology [Internet]. 2021 Sep 8 [cited 2021 Nov 19];
- ↑ Duggan M, Kavanagh BP. Atelectasis in the perioperative patient. Curr Opin Anaesthesiol. 2007;20:37-42.
- ↑ Khan AN, Al-Jahdali H, AL-Ghanem S, Gouda A. Reading chest radiographs in the critically ill (Part II): Radiography of lung pathologies common in the ICU patient. Annals of Thoracic Medicine [Internet]. 2009;4(3):149–57.
- ↑ 22.0 22.1 Woodring J. Determining the cause of pulmonary atelectasis: a comparison of plain radiography and CT. American Journal of Roentgenology. 1988 Apr;150(4):757–63.
- ↑ Lichtenstein D, Meziere G. Ultrasound diagnosis of atelectasis [Internet]. ResearchGate. unknown; 2005 [cited 2021 Nov 20].
- ↑ Liu J, Chen S-W, Liu F, Li Q-P, Kong X-Y, Feng Z-C. The Diagnosis of Neonatal Pulmonary Atelectasis Using Lung Ultrasonography. Chest [Internet]. 2015 Apr [cited 2021 Nov 20];147(4):1013–9.
- ↑ Acosta CM, Maidana GA, Jacovitti D, Belaunzarán A, Cereceda S, Rae E, et al. Accuracy of Transthoracic Lung Ultrasound for Diagnosing Anesthesia-induced Atelectasis in Children. Anesthesiology [Internet]. 2014 Jun 1 [cited 2021 Nov 20];120(6):1370–9.
- ↑ 26.0 26.1 26.2 26.3 Stiller K, Geake T, Taylor J, Grant R, Hall B. Acute lobar atelectasis: a comparison of two chest physiotherapy regimens. Chest. 1990 Dec 1;98(6):1336-40.
- ↑ 27.0 27.1 Schindler MB. Treatment of atelectasis: where is the evidence?. Critical Care. 2005 Aug;9(4):341.
- ↑ 28.0 28.1 28.2 Mendes LP, Teixeira LS, da Cruz LJ, Vieira DS, Parreira VF. Sustained maximal inspiration has similar effects compared to incentive spirometers. Respiratory physiology & neurobiology. 2019 Mar 1;261:67-74.
- ↑ Tan AK. Incentive spirometry for tracheostomy and laryngectomy patients. The Journal of otolaryngology. 1995 Oct;24(5):292-4.
- ↑ Possa SS, Amador CB, Costa AM, Sakamoto ET, Kondo CS, Vasconcellos AM, et al. Implementation of a guideline for physical therapy in the postoperative period of upper abdominal surgery reduces the incidence of atelectasis and length of hospital stay. Rev Port Neumol 2014;20(2): 69-77.
- ↑ Moradian ST, Najafloo M, Mahmoudi H, Ghiasi MS. Early mobilization reduces the atelectasis and pleural effusion in patients undergoing coronary artery bypass graft surgery: A randomized clinical trial. J Vasc Nurs 2017;35(3):141–145.