Arachnoiditis: Difference between revisions
Reem Ramadan (talk | contribs) No edit summary |
Reem Ramadan (talk | contribs) No edit summary |
||
| Line 5: | Line 5: | ||
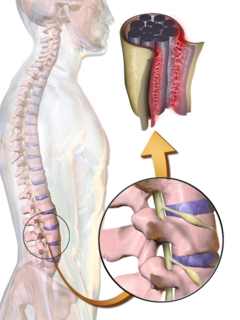
<div class="noeditbox">==Page Under Review== This article is currently under review and may not be up to date. Please come back soon to see the finished work! ({{REVISIONDAY}}/{{REVISIONMONTH}}/{{REVISIONYEAR}}) </div>[[File:Arachnoiditis_Image.png|alt=Arachnoiditis|320x320px|Arachnoiditis|right]] | <div class="noeditbox">==Page Under Review== This article is currently under review and may not be up to date. Please come back soon to see the finished work! ({{REVISIONDAY}}/{{REVISIONMONTH}}/{{REVISIONYEAR}}) </div>[[File:Arachnoiditis_Image.png|alt=Arachnoiditis|320x320px|Arachnoiditis|right]] | ||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
The central nervous system (CNS) which is made up of the brain and the spinal cord is covered and protected by [[meninges]]. Meninges are generally three membrane layers, the Dura Matter which is the outer layer, Arachnoid Matter which is the middle layer, and the Pia Matter which is the inner layer. There are 31 pairs of spinal nerves that exit the vertebral column, one on the right side and the other on the left, through vertebral foramina<ref>Moore KL, Dalley AF, Agur AM. Clinically oriented anatomy. 7th ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins Health; 2014. </ref>. | |||
== Pathological Process == | |||
== | |||
Arachnoiditis is a progressive disorder that involves the brain and/or the spinal cord caused by inflammation of the arachnoid membrane. There are several types of Arachnoiditis including Adhesive Arachnoiditis which is the most severe type and occurs when spinal nerves stick together, Arachnoiditis ossificans which occurs when arachnoid turns to bone, Cerebral arachnoiditis which affects the membranes surrounding the brain, Hereditary arachnoiditis which is congenital and rare and occurs due to defects affecting the meninges, Neoplastic arachnoiditis which occurs due to cancer and Optochiasmatic arachnoiditis which involves optic nerve<ref>Peng H, Conermann T. Arachnoiditis. InStatPearls. 2021 Nov 8. StatPearls Publishing.</ref>. <br>There are 3 main stages of Arachnoiditis. The first stage involves the inflammation of the spinal nerves, hyperemia, the disappearance of the subarachnoid space and the scare tissue begins to form. The second stage involves the scar tissue formation process increasing and the nerves further adhere to each other and to the dura. The third stage involves the complete encapsulation of the nerve roots, compression causes atrophy of the nerve roots and the scarring tissues prevent the production of spinal fluid in that area. In some cases, the scar tissue calcifies and is then termed Arachnoiditis Ossificans<ref>Deshmukh, V.R. Encyclopedia of the Neurological Sciences (Second Edition). Brain and Spine Institute, Portland, OR, USA. 2014. </ref>. | |||
== Etiologies == | |||
Arachnoiditis can be caused by: | |||
'''Trauma/Surgery-induced''': Arachnoiditis considered a rare complication of spinal surgery specifically after multiple of complex surgeries or trauma to the spine. Multiple lumbar punctures, advanced stages of spinal stenosis and chronic degenerative disc disease may also lead to arachnoiditis. This may result in blood penetration in the subarachnoid space causing inflammation. '''Chemical-induced''': Myelograms have been considered recently to cause this condition. A myelogram which is a diagnostic test that contains a dye is usually injected in the area surrounding the spinal cord and nerves and is visible on various diagnostic imaging such as X-ray, MRI and CT scan. The repetitive exposure to oil based radiographic contrast agents used in myelograms causes Arachnoiditis. In addition to that, medications found in epidural steroid injections can cause Arachnoiditis especially if they enter the cerebral spinal fluid (CSF). It's also important to note that, Arachnoiditis due to surgery is precisely localized, meanwhile the one due to epidural injections is more diffuse.<br>'''Infection-induced''': Arachnoiditis can also be caused by viral or bacterial meningitis, tuberculosis and syphilis affect the spine.<br>Arachnoiditis is also the third most common cause of Failed Back Surgery Syndrome (FBSS). | |||
== Clinical Presentation == | == Clinical Presentation == | ||
| Line 29: | Line 29: | ||
add links to outcome measures here (see [[Outcome Measures|Outcome Measures Database]]) | add links to outcome measures here (see [[Outcome Measures|Outcome Measures Database]]) | ||
== Management / Interventions | == Management / Interventions == | ||
==== Medical/Surgical Management: ==== | ==== Medical/Surgical Management: ==== | ||
| Line 41: | Line 41: | ||
== Differential Diagnosis<br> == | == Differential Diagnosis<br> == | ||
Disc fragments, recurrent disc herniation, stenosis, spondylosis, epidural fibrosis and other causes of polyneuropathy such as multiple sclerosis. | Disc fragments, recurrent disc herniation, stenosis, spondylosis, epidural fibrosis and other causes of polyneuropathy such as multiple sclerosis. | ||
== References == | |||
<references /> | <references /> | ||
[[Category:Neurological - Conditions]] | [[Category:Neurological - Conditions]] | ||
Revision as of 16:24, 14 February 2023
Clinically Relevant Anatomy[edit | edit source]
The central nervous system (CNS) which is made up of the brain and the spinal cord is covered and protected by meninges. Meninges are generally three membrane layers, the Dura Matter which is the outer layer, Arachnoid Matter which is the middle layer, and the Pia Matter which is the inner layer. There are 31 pairs of spinal nerves that exit the vertebral column, one on the right side and the other on the left, through vertebral foramina[1].
Pathological Process[edit | edit source]
Arachnoiditis is a progressive disorder that involves the brain and/or the spinal cord caused by inflammation of the arachnoid membrane. There are several types of Arachnoiditis including Adhesive Arachnoiditis which is the most severe type and occurs when spinal nerves stick together, Arachnoiditis ossificans which occurs when arachnoid turns to bone, Cerebral arachnoiditis which affects the membranes surrounding the brain, Hereditary arachnoiditis which is congenital and rare and occurs due to defects affecting the meninges, Neoplastic arachnoiditis which occurs due to cancer and Optochiasmatic arachnoiditis which involves optic nerve[2].
There are 3 main stages of Arachnoiditis. The first stage involves the inflammation of the spinal nerves, hyperemia, the disappearance of the subarachnoid space and the scare tissue begins to form. The second stage involves the scar tissue formation process increasing and the nerves further adhere to each other and to the dura. The third stage involves the complete encapsulation of the nerve roots, compression causes atrophy of the nerve roots and the scarring tissues prevent the production of spinal fluid in that area. In some cases, the scar tissue calcifies and is then termed Arachnoiditis Ossificans[3].
Etiologies[edit | edit source]
Arachnoiditis can be caused by:
Trauma/Surgery-induced: Arachnoiditis considered a rare complication of spinal surgery specifically after multiple of complex surgeries or trauma to the spine. Multiple lumbar punctures, advanced stages of spinal stenosis and chronic degenerative disc disease may also lead to arachnoiditis. This may result in blood penetration in the subarachnoid space causing inflammation. Chemical-induced: Myelograms have been considered recently to cause this condition. A myelogram which is a diagnostic test that contains a dye is usually injected in the area surrounding the spinal cord and nerves and is visible on various diagnostic imaging such as X-ray, MRI and CT scan. The repetitive exposure to oil based radiographic contrast agents used in myelograms causes Arachnoiditis. In addition to that, medications found in epidural steroid injections can cause Arachnoiditis especially if they enter the cerebral spinal fluid (CSF). It's also important to note that, Arachnoiditis due to surgery is precisely localized, meanwhile the one due to epidural injections is more diffuse.
Infection-induced: Arachnoiditis can also be caused by viral or bacterial meningitis, tuberculosis and syphilis affect the spine.
Arachnoiditis is also the third most common cause of Failed Back Surgery Syndrome (FBSS).
Clinical Presentation[edit | edit source]
Most patients have symptoms in the lower back, hip, legs, feet, perineum, abdomen or ,in the most severe cases, throughout the body. These symptoms are: chronic, burning pain; tingling; weakness in the legs; sensory loss; muscle cramps; spasms; uncontrolled twitching; bladder and sexual dysfunctions[4].
Diagnostic Procedures[edit | edit source]
Magnetic resonance imaging (MRI) is the study of choice for the diagnostic evaluation of arachnoiditis[5]. For patients in whom MRI is contraindicated, computed tomography (CT) myelography is an acceptable alternative.
Outcome Measures[edit | edit source]
add links to outcome measures here (see Outcome Measures Database)
Management / Interventions[edit | edit source]
Medical/Surgical Management:[edit | edit source]
There is no cure, only treatment of the chronic symptoms.
-Oral medication or medication through an intrathecal pump such as: non-steroidal anti-inflammatory drugs (NSAIDs), methadon, morphine, can be used to release neuropathic pain. Antidepressants may reduce burning neuropathic pain, but in much lower doses than for depression. Diazepam is used for muscle relaxation.
-Invasive treatment such as intraspinal narcotic analgesia (INA), epidural steroid and local anaesthetic injections are not indicated because there is a risk of exacerbating the inflammation and worsening the patient’s condition.
-Spinal cord Electrostimulation (SCS) stand for electrical stimulation by implanted electrodes around the spinal cord in the area that is most involved in causing pain. Some studies indicate a 50% success rate when all types of chronic pain are considered[6].
-Surgery is not recommended because it causes more scar tissue and more trauma to the already irritated spinal cord.
Physiotherapy:[edit | edit source]
Physiotherapy has a role in the management of the chronic pain caused by Arachnoiditis.
Differential Diagnosis
[edit | edit source]
Disc fragments, recurrent disc herniation, stenosis, spondylosis, epidural fibrosis and other causes of polyneuropathy such as multiple sclerosis.
References[edit | edit source]
- ↑ Moore KL, Dalley AF, Agur AM. Clinically oriented anatomy. 7th ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins Health; 2014.
- ↑ Peng H, Conermann T. Arachnoiditis. InStatPearls. 2021 Nov 8. StatPearls Publishing.
- ↑ Deshmukh, V.R. Encyclopedia of the Neurological Sciences (Second Edition). Brain and Spine Institute, Portland, OR, USA. 2014.
- ↑ MATLOCK, C.L., ‘Physiotherapy and spinal nerve root adhesions: a caution’, Physiotherapy research international, vol: 9(4), p. 164-173,2004.
- ↑ Malani AN, Vandenberg DM, Singal B, Kasotakis M, Koch S, Moudgal V, et al. Magnetic resonance imaging screening to identify spinal and paraspinal infections associated with injections of contaminated methylprednisolone acetate. JAMA. Jun 19 2013;309(23):2465-72.
- ↑ FREY, M.E., MANCHIKANTI, L., BENYAMIN, R.M., SCHULTZ, D.M.,SMITH, H.S.,COHEN, S.P., ‘Spinal Cord Stimulation for Patients with Failed Back Surgery Syndrome: A Systematic Review’, Pain Physician, vol: 12:379-397, 2009