Apley's Test: Difference between revisions
mNo edit summary |
Evan Thomas (talk | contribs) mNo edit summary |
||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- [[User:Tomas Whyatt|Tom Whyatt]], [[User:Eilis Fitzgerald|Eilis Fitzgerald]], [[User:Faisal alanezi|Faisal Alanezi]], [[User:Abdulkareem Almutairi|Abdulkareem Almutairi]], [[User:Sinead McCarthy|Sinead McCarthy]], [[User:Conor Mc Hugh|Conor McHugh]] (as part of the [[User:RCSI]] student project). | '''Original Editor ''' - [[User:Tomas Whyatt|Tom Whyatt]], [[User:Eilis Fitzgerald|Eilis Fitzgerald]], [[User:Faisal alanezi|Faisal Alanezi]], [[User:Abdulkareem Almutairi|Abdulkareem Almutairi]], [[User:Sinead McCarthy|Sinead McCarthy]], [[User:Conor Mc Hugh|Conor McHugh]] (as part of the [[User:RCSI]] student project). | ||
''' | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Background to Apley's == | |||
== Test Description | The Appley's grind test is used to evaluate individuals for problems of the meniscus in the knee. This test is named after Alan Graham Appley (1914 - 1996), a British orthopedic surgeon, who discovered this assessment technique<ref>Who Named It. Alan Graham Apley, Available from: [http://www.whonamedit.com/doctor.cfm/203.html http://www.whonamedit.com/doctor.cfm/203.html] [last accessed 28/5/9]</ref>.Diagnosis of meniscal injuries can be difficult as the menisci are avascular and have no nerve supply on their inner two thirds, resulting in very little pain or swelling when an injury occurs<ref name="Magee">David J. Magee. Orthopedic Physical Assessment. 5th Edition. W.B. Saunders, London; 2002.</ref> | ||
== Test Description == | |||
Appley's grinding test involves placing the patient in the prone position with the knee flexed to 90 degrees<ref>Christopher Norris. Sports Injuries: Diagnosis and Management, Third Edition. Butterworth-Heinemann;2004.</ref>. The patient's thigh is then rooted to the examining table with the examiner's knee. The examiner laterally and medially rotates the tibia, combined first with distraction, while noting any excessive movement, restriction or discomfort. The process is then repeated using compression instead of distraction<ref name="Magee" />. If rotation plus distraction is more painful or shows increased rotation relative to the normal side, the lesion is most likely to be ligamentous<ref name="Magee" />. If the rotation plus compression is more painful or shows decreased rotation relative to the normal side, the lesion is most likely to be a meniscus injury<ref name="Magee" />. | Appley's grinding test involves placing the patient in the prone position with the knee flexed to 90 degrees<ref>Christopher Norris. Sports Injuries: Diagnosis and Management, Third Edition. Butterworth-Heinemann;2004.</ref>. The patient's thigh is then rooted to the examining table with the examiner's knee. The examiner laterally and medially rotates the tibia, combined first with distraction, while noting any excessive movement, restriction or discomfort. The process is then repeated using compression instead of distraction<ref name="Magee" />. If rotation plus distraction is more painful or shows increased rotation relative to the normal side, the lesion is most likely to be ligamentous<ref name="Magee" />. If the rotation plus compression is more painful or shows decreased rotation relative to the normal side, the lesion is most likely to be a meniscus injury<ref name="Magee" />. | ||
| Line 15: | Line 15: | ||
{{#ev:youtube|6Z_9lfX_Pc8}}<ref> Physiotutors. Apley's Test⎟Meniscus Damage. Available from: https://www.youtube.com/watch?v=6Z_9lfX_Pc8</ref> | {{#ev:youtube|6Z_9lfX_Pc8}}<ref> Physiotutors. Apley's Test⎟Meniscus Damage. Available from: https://www.youtube.com/watch?v=6Z_9lfX_Pc8</ref> | ||
== Reliability of | == Reliability of the Test == | ||
Many studies have attempted to quantitate the reliability of various physical examination findings. In a prospective study comparing preoperative joint line tenderness to arthroscopic findings of meniscal tears, the sensitivity of joint line tenderness was found to be 86% and 92% with an overall accuracy rate of 74% and 96% for the medial and lateral meniscus, respectively, another study found similar results, with joint line tenderness having a sensitivity of 74%. The only significant McMurray sign to correlate with a meniscal injury was a “thud” elicited on the medial joint line with a medial meniscal tear. However, the McMurray and Apley tests were found by others to have less than 75% sensitivity for diagnosing meniscal tears<ref>Patrick J. McMahon (2006). Current diagnosis & treatment in sports medicine. McGraw-Hill Medical.</ref><br> | Many studies have attempted to quantitate the reliability of various physical examination findings. In a prospective study comparing preoperative joint line tenderness to arthroscopic findings of meniscal tears, the sensitivity of joint line tenderness was found to be 86% and 92% with an overall accuracy rate of 74% and 96% for the medial and lateral meniscus, respectively, another study found similar results, with joint line tenderness having a sensitivity of 74%. The only significant McMurray sign to correlate with a meniscal injury was a “thud” elicited on the medial joint line with a medial meniscal tear. However, the McMurray and Apley tests were found by others to have less than 75% sensitivity for diagnosing meniscal tears<ref>Patrick J. McMahon (2006). Current diagnosis & treatment in sports medicine. McGraw-Hill Medical.</ref><br> | ||
== Sensitivity of the Test | == Sensitivity of the Test == | ||
Diagnostic accuracy studies of meniscal tests are described to have poor methodologic quality with highly heterogeneous results, therefore poor value for clinical practice<ref>Scholten RJ, Deville WL, Opstelten W, Bijl D, van der Plas CG, Bouter LM. The accuracy of physical diagnostic tests for assessing meniscal lesions of the knee: a meta-analysis. J Fam Pract. 2001; 50:938-944.</ref>. A recent meta-analysis reports sensitivity and specificity to be 60% and 70% respectively<ref>Hegedus EJ, Cook C, Hasselblad V, Goode A, McCrory DC. Physical examination tests for assessing a torn meniscus in the knee: a systematic review with meta-analysis. Journal of Orthopaedic and Sports Physical Therapy, 2007; 37(9), 541-50.</ref>. | Diagnostic accuracy studies of meniscal tests are described to have poor methodologic quality with highly heterogeneous results, therefore poor value for clinical practice<ref>Scholten RJ, Deville WL, Opstelten W, Bijl D, van der Plas CG, Bouter LM. The accuracy of physical diagnostic tests for assessing meniscal lesions of the knee: a meta-analysis. J Fam Pract. 2001; 50:938-944.</ref>. A recent meta-analysis reports sensitivity and specificity to be 60% and 70% respectively<ref>Hegedus EJ, Cook C, Hasselblad V, Goode A, McCrory DC. Physical examination tests for assessing a torn meniscus in the knee: a systematic review with meta-analysis. Journal of Orthopaedic and Sports Physical Therapy, 2007; 37(9), 541-50.</ref>. | ||
| Line 30: | Line 30: | ||
[[Image:Knee meniscus surgery rationale02-1-.jpg]]Torn Meniscus image<ref>[http://www.eorthopod.com/images/ContentImages/knee/knee_meniscus_surgery/knee_meniscus_surgery_rationale02.jpg www.eorthopod.com/images/ContentImages/knee/knee_meniscus_surgery/knee_meniscus_surgery_rationale02.jpg]</ref> | [[Image:Knee meniscus surgery rationale02-1-.jpg]]Torn Meniscus image<ref>[http://www.eorthopod.com/images/ContentImages/knee/knee_meniscus_surgery/knee_meniscus_surgery_rationale02.jpg www.eorthopod.com/images/ContentImages/knee/knee_meniscus_surgery/knee_meniscus_surgery_rationale02.jpg]</ref> | ||
<br> | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Assessment]] [[Category:Special_Tests]] [[Category:Knee]] [[Category:Knee_Examination]] [[Category:Musculoskeletal/Orthopaedics]] | [[Category:Assessment]] [[Category:Special_Tests]] [[Category:Knee]] [[Category:Knee_Examination]] [[Category:Musculoskeletal/Orthopaedics]] | ||
Revision as of 06:59, 6 December 2017
Original Editor - Tom Whyatt, Eilis Fitzgerald, Faisal Alanezi, Abdulkareem Almutairi, Sinead McCarthy, Conor McHugh (as part of the User:RCSI student project).
Top Contributors - Admin, Eilis Fitzgerald, Sinead McCarthy, Rachael Lowe, Kim Jackson, Adam Vallely Farrell, Redisha Jakibanjar, Kai A. Sigel, Abdulkareem Almutairi, Faisal alanezi, Evan Thomas, WikiSysop, Claire Knott, 127.0.0.1, Wanda van Niekerk, Tony Lowe, Conor Mc Hugh and Laura Ritchie
Background to Apley's[edit | edit source]
The Appley's grind test is used to evaluate individuals for problems of the meniscus in the knee. This test is named after Alan Graham Appley (1914 - 1996), a British orthopedic surgeon, who discovered this assessment technique[1].Diagnosis of meniscal injuries can be difficult as the menisci are avascular and have no nerve supply on their inner two thirds, resulting in very little pain or swelling when an injury occurs[2]
Test Description[edit | edit source]
Appley's grinding test involves placing the patient in the prone position with the knee flexed to 90 degrees[3]. The patient's thigh is then rooted to the examining table with the examiner's knee. The examiner laterally and medially rotates the tibia, combined first with distraction, while noting any excessive movement, restriction or discomfort. The process is then repeated using compression instead of distraction[2]. If rotation plus distraction is more painful or shows increased rotation relative to the normal side, the lesion is most likely to be ligamentous[2]. If the rotation plus compression is more painful or shows decreased rotation relative to the normal side, the lesion is most likely to be a meniscus injury[2].
Reliability of the Test[edit | edit source]
Many studies have attempted to quantitate the reliability of various physical examination findings. In a prospective study comparing preoperative joint line tenderness to arthroscopic findings of meniscal tears, the sensitivity of joint line tenderness was found to be 86% and 92% with an overall accuracy rate of 74% and 96% for the medial and lateral meniscus, respectively, another study found similar results, with joint line tenderness having a sensitivity of 74%. The only significant McMurray sign to correlate with a meniscal injury was a “thud” elicited on the medial joint line with a medial meniscal tear. However, the McMurray and Apley tests were found by others to have less than 75% sensitivity for diagnosing meniscal tears[5]
Sensitivity of the Test[edit | edit source]
Diagnostic accuracy studies of meniscal tests are described to have poor methodologic quality with highly heterogeneous results, therefore poor value for clinical practice[6]. A recent meta-analysis reports sensitivity and specificity to be 60% and 70% respectively[7].
Graphics/ Photos[edit | edit source]
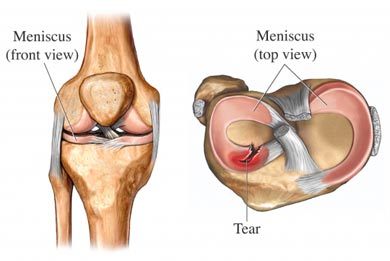 Meniscus image[8]
Meniscus image[8]
 MRI showing Normal Meniscus Vs Torn Meniscus[9]
MRI showing Normal Meniscus Vs Torn Meniscus[9]
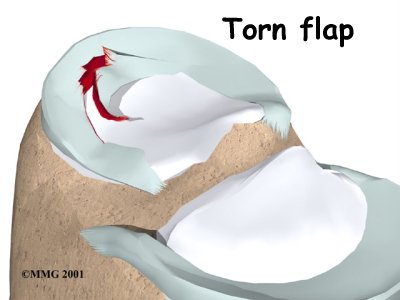 Torn Meniscus image[10]
Torn Meniscus image[10]
References[edit | edit source]
- ↑ Who Named It. Alan Graham Apley, Available from: http://www.whonamedit.com/doctor.cfm/203.html [last accessed 28/5/9]
- ↑ 2.0 2.1 2.2 2.3 David J. Magee. Orthopedic Physical Assessment. 5th Edition. W.B. Saunders, London; 2002.
- ↑ Christopher Norris. Sports Injuries: Diagnosis and Management, Third Edition. Butterworth-Heinemann;2004.
- ↑ Physiotutors. Apley's Test⎟Meniscus Damage. Available from: https://www.youtube.com/watch?v=6Z_9lfX_Pc8
- ↑ Patrick J. McMahon (2006). Current diagnosis & treatment in sports medicine. McGraw-Hill Medical.
- ↑ Scholten RJ, Deville WL, Opstelten W, Bijl D, van der Plas CG, Bouter LM. The accuracy of physical diagnostic tests for assessing meniscal lesions of the knee: a meta-analysis. J Fam Pract. 2001; 50:938-944.
- ↑ Hegedus EJ, Cook C, Hasselblad V, Goode A, McCrory DC. Physical examination tests for assessing a torn meniscus in the knee: a systematic review with meta-analysis. Journal of Orthopaedic and Sports Physical Therapy, 2007; 37(9), 541-50.
- ↑ http://services.epnet.com/getimage.aspx?imageiid=7305
- ↑ Athletic Advisor. Meniscal MRI. Available from: www.athleticadvisor.com/Injuries/LE/Knee/mensical_mri.htm [last accessed 28/5/9]
- ↑ www.eorthopod.com/images/ContentImages/knee/knee_meniscus_surgery/knee_meniscus_surgery_rationale02.jpg






